Multiple ring enhancing lesions in brain: Neurocysticercosis or Tuberculoma? An extremely unusual / uncommon radiological presentation of a common disease: central nervous system tuberculosis
Manjunath M N, Bhakyalakshmi, Lakshmi, Chaitanya and Sharanya
Cite this article as: BJMP 2016;9(1):a907
|
|
Abstract Cerebral tuberculomas is a rare and serious form of tuberculosis (TB) due to the haematogenous spread of Mycobacterium Tuberculosis (MT). Symptoms and radiologic features are nonspecific, leading sometimes to misdiagnosis. Multiple ring-enhancing lesions in the brain often raise many questions about the true diagnosis. It can present as tuberculous meningitis with complications such as infractions of cerebral cortex, cranial nerve dysfunction, brain stem being the site of greatest involvement, hydrocephalus, cerebral edema and tuberculoma. The clinical progression of tuberculous meningitis may be rapid or gradual. Rapid progression is more often seen in young children. The diagnoses can be difficult early in its course and radiographic studies can aid in diagnosis. Tuberculoma may be confused with Neurocysticercosis radiologically, however various distinguishing features exist. We present a case of CNS tuberculosis presenting as multiple tuberculomas causing great difficulty to distinguish with other similar radiological lesions. Keywords: Tuberculoma, Neurocysticercosis, Gene-Xpert, Ring enhancing lesionsAbbreviations: MT- Mycobacterium Tuberculosis, AFB- Acid fast bacilli, ATT- Anti tubercular therapy, EVD- External ventricular drain |
Case Summary
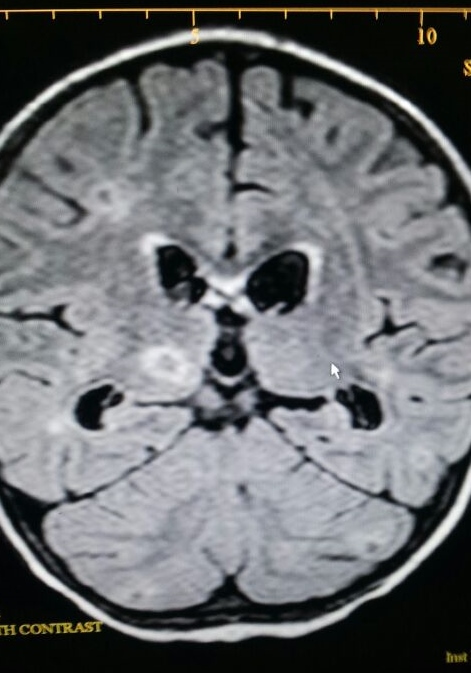
Three and half year old male child presented to PICU, Narayana health BANGALORE, with a short history of fever of 8 days with headache and cough for 2 days. At admission the child was febrile, dull looking, haemodynamically stable with no meningeal signs or focal neurological deficit. He was admitted and evaluated for the cause of fever. Same day child developed generalized seizures along with fever, hence a possibility of meningitis or electrolyte imbalance (hyponatremia) kept as child had initial serum sodium of 128meq/l. The cause of hyponatremia was looked into and child managed with antiepileptic drugs and 3% normal saline infusion. The initial sepsis screen was in-conclusive and CSF analysis showed 3 lymphocytes with low glucose and elevated protein levels, hence partially treated meningitis was considered (as h/o admission to a hospital for 3 days prior to admission in our hospital). The antimeningitic dose of IV antibiotics were given. On day 3 of admission child developed meningeal signs with worsening sensorium, hence neuro imaging was done (MRI brain) which showed multiple well defined ring enhancing lesion at bilateral central and cerebrallar hemisphere, thalamus, pons with mild perilesional edema. This radiological picture suggested a possibility of nerucysticercosis, however the clinical picture did not match with the same, hence pediatric neurology opinion was taken and simultaneous workup for tuberculosis were started. Child was also started on IV steroid. A strong possibility of CNS toxoplasmosis was kept by neurologist based on radiological picture. The workup for TB was inconclusive (negative mantoux, normal ESR, negative gastric aspirate for AFB) however child was empirically started on category II ATT in view of deteriorating clinical state. Repeat CSF evaluation showed increasing cell counts and similar biochemical picture as before, the sample was also send for Gene-Xpert (DNA amplification study). On day 6 of admission child developed lethargy and drowsiness hence antiedema measures were initiated. Same day he developed tonic posturing with unequal pupil, hypertension and bradycardia indicating raised Intracranial pressure (ICP), for which he was intubated and ventilated and urgent repeat CT head was done which showed increase in ventricular size and hydrocephalus. Immediately EVD was put by neurosurgeons after which there was gradual improvement in child’s condition and he was extubated within 48 hours. The reports showed negative HIV and toxoplasma serology and positive CSF gene study for AFB confirming the diagnosis of CNS tuberculosis, hence ATT and antiedema measures were continued and the EVD was later converted into VP shunt. Child by 2nd week of illness became afebrile with improved sensorium and function.
Fig 1 & 2: MRI showing multiple ring enhancing lesions

Discussion
Tuberculosis remains a leading cause of morbidity and mortality in the developing world. CNS involvement is thought to occur in 2-5% of patients with tuberculosis and up to 15% of those with AIDS related tuberculosis 1,2. Although CNS involvement by tuberculosis is seen in all age groups, there is a predilection for younger patients, with 60-70% of cases occurring in patients younger than 20 years of age 2. Haematogeneous spread from the lungs or gastrointestinal tract is most common, leading to small subpial or subependymal infective foci. These are termed Rich foci and form a reservoir from which intracranial manifestations may arise 3,4. Tuberculomas often present with symptoms and signs of focal neurological deficit without evidence of systemic disease. The radiologic features are also nonspecific and differential diagnosis includes malignant lesions, sarcoidosis, pyogenic abscess, toxoplasmosis and cysticercosis.5,6
Regarding treatment, the Center for Disease Control and Prevention recommends 12 months of treatment for CNS TB when the MT strain is sensitive to all drugs.7 However numerous variables can affect the response of the disease to therapy and it has been suggested that treatment duration should be tailored to the radiological response.8 After 12 months of treatment more than two-thirds of the patients still have contrast enhancing lesions. Although it is not clear if this represents an active lesion or just inflammation, continuing treatment is probably prudent. Total resolution of the tuberculoma is observed when scans demonstrate no enhancing lesions or only an area of calcification.8
In the case described above child had tubercular mengitis, multiple tuberculous, hydrocephalus and raised ICP. Although clinical presentations were suggestive of same, however the radiological picture and initial CSF finding raised suspicion is diagnosis. As tuberculoma and NCC shows many common clinical features, there are few distinguishing features such as the cysticercosis is smaller, less perilesional edema, multiple numbers and less of midline shift as compared to tuberculoma. However in our patient the multiple tuberculi gave a suspicion of NCC. It was only gene expert which confirmed our diagnosis.
Hence clinical cases like Tuberculoma, the radiological findings of which can usually be distinguished from other common illness like Neurocysticercosis or Toxoplasmosis, sometimes pose challenge in terms of radiological diagnosis suggesting the need for detailed evaluation to reach the diagnosis and guide treatment.
|
Acknowledgements None Competing Interests None declared Author Details MANJUNATH M N, Junior Consultant, Columbia Asia Hospitals, Bangalore. LAKSHMI.K.N, Registrar, Rainbow Hospital, Bangalore. BHAKYALAKSHMI, Junior Consultant, Columbia Asia Hospitals, Bangalore. CHAITANYA NAIR, Registrar, Narayana Health, Bangalore. SHARANYA R, Registrar. CORRESPONDENCE: DR MANJUNATH M N, Junior Consultant, Columbia Asia Hospitals, Bangalore. Email: drmanju.drmanju@gmail.com |
References
- Burrill J, Williams CJ, Bain G et-al. Tuberculosis: a radiologic review. Radiographics. 27 (5): 1255-73. doi:10.1148/rg.275065176 - Pubmed citation.
- Kornienko VN, Pronin IN. Diagnostic Neuroradiology. Springer Verlag. (2009) ISBN:3540756523. Read it at Google Books - Find it at Amazon.
- Engin G, Acunaş B, Acunaş G et-al. Imaging of extrapulmonary tuberculosis. Radiographics. 20 (2): 471-88. Radiographics (full text) - Pubmed citation
- Gupta RK, Lufkin RB. MR imaging and spectroscopy of central nervous system infection. Springer Us. (2001) ISBN:0306465515. Read it at Google Books - Find it at Amazon
- S.Sahaiu-Srivastava, B. Jones Brainstem tuberculoma in the immunocompetent: case report and literature review Clinical Neurology and Neurosurgery, 110 (2008), pp. 302–304
- G.I. Ogbole, O.S. Bassey, C.A. Okolo, S.O. Ukperi, A.O. Ogunseyinde Testicular tuberculosis presenting with metastatic intracranial tuberculomas: a case report.
- Centers for Disease Control and Prevention. Treatment of Tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR 2003; 52 .
- S.I. Poonnoose, V. Rajshekhar Rate of resolution of histologically verified intracranial tuberculomas Neurosurgery, 53 (2003), pp. 873–879

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




