The use of dermoscopy amongst dermatology trainees in the United Kingdom
Claire Reid, Kimberlee Lim & Catriona Henderson
Cite this article as: BJMP 2018;11(2):a1110
|
A dermatoscope is a hand-held device for examining the appearance of the skin. Dermoscopy has become an increasingly used and valued tool in the assessment of various skin lesions, and more recently, inflammatory rashes. It is quick, cheap and when used correctly, dermoscopy is an essential tool in helping clinicians detect early stage skin cancer. Various national and international guidelines recommend routine use of dermoscopy in the assessment of pigmented lesions1,2 because it enhances melanoma detection rates3,4 and can help confirm the diagnosis of benign lesions such as haemangiomas and seborrhoeic keratoses. As with any skill, competency takes time to develop and a combination of various learning and assessment methods is best. The dermatology specialist training curriculum in the United Kingdom (UK) states that trainees should be competent in using a dermatoscope and interpreting findings, while recognizing the limitations of this tool5. Assessment of these clinical skill and behavioural competencies using direct observation of procedural skills (DOPS), case-based discussion (CBD), mini clinical examination (mini-CEX), and/or multisource feedback (MSF) is suggested. There is no specific guidance on what resources a trainee should use to achieve these competencies, nor on what is the minimum expected dermoscopy skillset at completion of specialist training.
The aim of this survey was to explore dermoscopy use amongst dermatology specialist trainee registrars in the UK including frequency of use, how it is being taught and whether trainees feel their dermoscopy training has been adequate.
An online survey was designed and distributed to dermatology trainees in the United Kingdom using an email link and hard copies were distributed at a national dermoscopy course. Respondents who did not identify themselves as dermatology trainees were removed from the analysis. Responses were collected anonymously, then collated and analysed using SurveyMonkey® computer software.
Twenty-five percent (59/238) of dermatology trainees completed the survey. On average, 92% (54/59) use dermoscopy more than once daily. Eighty-five percent (50/59) always use dermoscopy when assessing pigmented lesions while 34% (20/59) always and 59% (35/59) sometimes use it to assess non-pigmented lesions. When asked about specific tools used to learn dermoscopy, 41% (24/59) have been on a previous course, 42% (25/59) reported attendance at a lecture or seminar, 46% (27/59) have used a dermoscopy text book, 14% (8/59) have attended a conference, 19% (11/59) have used online resources. Seventeen percent (10/59) have never used any of the above learning methods. (Figure 1a). Amongst those who have attended a formal dermoscopy course (n=24), 92% (22/24) of these were ≤1 day in duration. When questioned about informal teaching in clinical practice, 12% (7/59) frequently, 56% (33/59) sometimes, 31% (18/59) rarely and 2% (1/59) never receive teaching from their supervising dermatology consultant. (Figure 1b). Fifty-four percent (32/59) feel they have received adequate training in dermoscopy while the remaining 46% (27/59) feel their dermoscopy training is inadequate for their training stage (Figure 1c). Seventy-three percent (43/59) have access to dermoscopic photography within their local dermatology department.
Fig 1a - Have you undertaken any formal study in dermoscopy? 49% of trainees have attended a lecture, 2% a seminar, 14% a conference, 41% a course, 19% have used an online resource, 46% have used a book, 17% have not used any resource.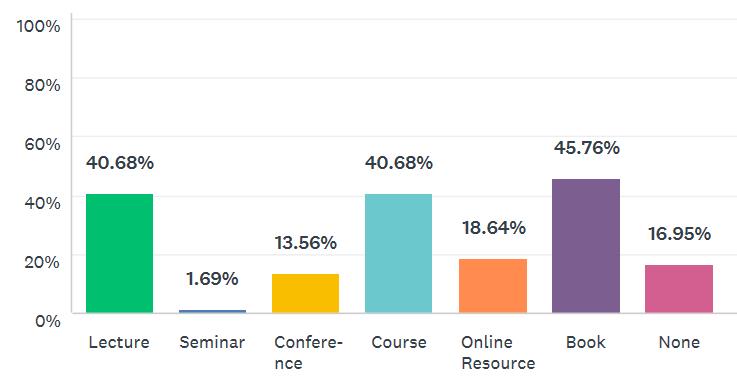
Fig 1b- Do you receive dermoscopy training from your supervisor in clinic? 56% of trainees sometimes, 31% rarely, 12% frequently, and 2% have never received training from their seniors in clinic.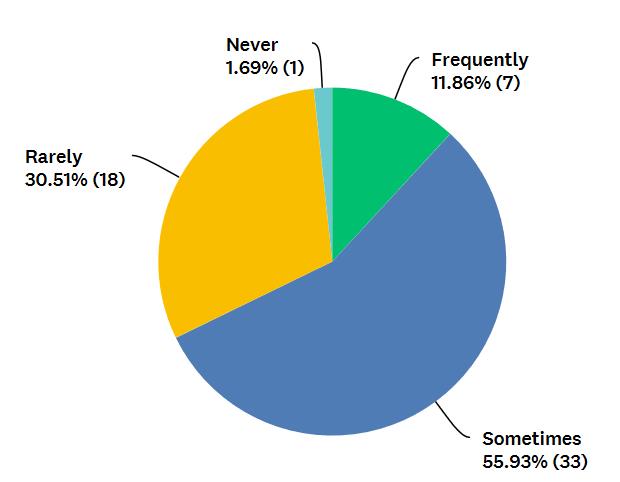
Fig 1c- Do you believe that you have received adequate training in the use of a dermoscopy for your training grade?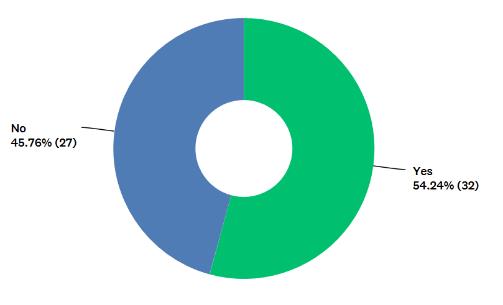
These results of this survey highlight the need for dermoscopy training to be reviewed within the UK national training curriculum for dermatology. Despite daily use by the vast majority, dermoscopy training is largely self-directed and highly variable amongst individual trainees. Of concern, a significant proportion of those who responded feel their dermoscopy skills are inadequate for their training stage. Of note, the 25% response rate means that the results of this survey may not be representative of dermatology trainees in the United Kingdom as a whole.
This is the first time that dermoscopy use has been explored through a national survey of dermatology trainees in the UK, to the best of our knowledge. A survey on dermoscopy use was carried out by The British Association of Dermatologists (BAD) in 20126 but the majority of responses were from dermatology consultants. This confirmed that 98.5% of respondents regularly used dermoscopy, while 81% had received any training. The most frequent source of training was UK based courses, which 62% of respondents reported attending. Of note, 39% of all respondents lacked confidence when making a diagnosis based on their interpretation of dermoscopy findings. It is not clear how many of those lacking in confidence were consultants, trainees or specialty doctors. Although the situation may have improved since 2012, these results do suggest that dermoscopy training needs have not been met for a proportion of doctors across the dermatology community.
Dermoscopy training is an important issue to address for several reasons. The volume of cutaneous lesions being referred to dermatology is increasing, and skin cancer referrals and treatment now account for 50% of a UK dermatologists’ workload7. For every melanoma diagnosed, a dermatologist may expect to see 20–40 benign lesions referred from general practitioners (GPs)7. These facts highlight the importance of maximising diagnostic skills which frequently include using dermoscopy as part of clinial assessment. Lack of adequate training is a common self-reported reason for dermatologists not using dermoscopy8. Both trainees and their supervising bodies have a responsibility to maximize training opportunities and embed the use of dermoscopy in routine practice.
In conclusion, we feel UK dermatology trainees and indeed any clinician who utilizes this tool, would benefit from a more standardized and integrated approach to dermoscopy teaching to ensure safe practice of this skill and deliver high quality evidence-based patient care.
|
Competing Interests Dr Catriona Henderson teaches at a dermoscopy course which is ran by the British Association of Dermatology Author Details CLAIRE REID, Medical Doctor, Dermatology Department, University Hospital Southampton NHS Foundation Trust, SO140YG England. KIMBERLEE LIM, Medical Doctor, Dermatology Department, University Hospital Southampton NHS Foundation Trust, SO140YG England. CATRIONA HENDERSON, Medical Doctor, Dermatology Department, University Hospital Southampton NHS Foundation Trust SO140YG England. CORRESPONDENCE: CLAIRE REID, Medical Doctor, Dermatology Department, University Hospital Southampton NHS Foundation Trust, SO140YG England Email: clairereid85@gmail.com |
References
- European Dermatology Forum; update of the guideline on the diagnosis and treatment of melanoma, developed by the guideline sub-committee ‘Melanoma’ of the European Dermatology Forum, 2012. Accessed at http://www.euroderm.org/edf/index.php/edf-guidelines/category/5-guidelines-miscellaneous
- Melanoma; assessment and management. National Institute for Health and Care Excellence. NICE guideline [NG-14], July 2015. Accessed at https://www.nice.org.uk/guidance/ng14/chapter/1-recommendations#assessing-melanoma-2
- Watts C.G., Dieng M., Morton R.L., Mann G.J., Menzies S.W., Cust A.E. Clinical practice guidelines for the identification, screening and follow-up of individuals at high risk of primary cutaneous melanoma: a systematic review. British Journal of Dermatology 2015;172;1:33-47
- Vestergaard M.E., Macaskill P., Holt P.E., Menzies S.W. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: a meta-analysis of studies performed in a clinical setting. British Journal of Dermatology 2008:159:3;669-676
- Specialty Training Curriculum for Dermatology August 2010 (amended August 2012) Joint Royal Colleges of Physicians Training Board. Accessed at https://www.jrcptb.org.uk/sites/default/files/2010%20Dermatology%20%28amendment%202012%29.pdf
- Butler T, Martin R, Affleck A, Fleming C, Bowling J. Trends in dermoscopy use in the UK: results from surveys in 2003 and 2013. Dermatology Practical and Conceptual 2015;5;(2);4:29-38
- Eedy D. Dermatology: a specialty in crisis. Clinical Medicine 2015;15;6 509–10
- Engasser H.C., Warshaw E.M. Dermatoscopy use by US dermatologists: A cross-sectional survey. Journal of the American Academy of Dermatology. 2010 Sep 1;63(3). Available from, DOI: 10.1016/j.jaad.2009.09.050

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




