Upgrading of Hospital Discharge Summary Software to Optimise COVID-19 Documentation and Safeguard Infection Prevention in the Community
Jack Donati-Bourne, Ning Lo, Wail Mohamed, Zain Kasmani, Masilamani Selvan & Jonathan O'Dair
Cite this article as: BJMP 2021;14(1):a002
|
|
Abstract Aims: Early review of 50 discharge summaries at Royal Shrewsbury Hospital (SATH) in April 2020 revealed only 27% documented the patient’s in-hospital COVID-19 test result and 2% outlined any recommended self-isolation advice following hospital discharge. This had potential adverse implications for community infection control as well as medico-legal sequalae for the Trust were the discharged patient to spread COVID-19 to other cohabitants. The urology team worked with SATH IT to amend the existing discharge summary software, to add two tabs to make COVID-19 test result and self-isolation documentation mandatory for successful sign-off. The aim of this quality improvement project was to evaluate the impact of updating the discharge summary software on documentation accuracy related to COVID-19 on discharge paperwork. Method: Following the implementation of the modified software, 50 consecutive discharge summaries for patients admitted under the urology team starting 1st October 2020 were retrospectively reviewed for documentation of COVID-19 result and self-isolation advice. Results: 90% of discharge summaries included COVID-19 test result and 100% included self-isolation advice for the patient, or alternatively confirmed that no self-isolation was required. Conclusions: This simple modification of an existing IT system greatly improved compliance with COVID-19 discharge summary documentation. We propose all hospitals consider adopting similar measures in the interest of infection prevention, public safety and potential medico-legal sequalae. Keywords: discharge summary, COVID-19, ITAbbreviations: COVID-19 - Coronavirus disease 19; IT - Information technology; GMC - General Medical Council. |
Introduction
The first documented case of COVID-19 in the UK was reported on 29 January 2020 followed by a rapid surge of infections leading to a UK national lockdown announced on 23 March 20201.
The COVID-19 pandemic has since required NHS hospitals to constantly adapt their protocols, workforce and logistics to keep pace with the evolving spread of the virus.
The variable clinical presentation of COVID-19 may result in those requiring admission being redirected under the care of different specialties within the hospital2. Furthermore the presence of asymptomatic carriers admitted with unrelated pathologies or cases of nosocomial cross-infections implies that COVID-19 related clinical noting and discharge summary documentation is likely to affect doctors across all hospital departments.
An initial review of 50 consecutive urology discharge summaries in Royal Shrewsbury Hospital in April 2020, revealed that only 27% included the patient’s in-hospital COVID-19 swab result (positive or negative) and only 2% documented any recommended patient self-isolation advice to be adhered to after discharge into the community.
Accurate COVID-19 related documentation is paramount to ensure the patient, their family and their GP / care setting where applicable are all aware of their COVID-19 status and any recommended self-isolation, to safeguard infection prevention in the community. Furthermore, there could be potential medicolegal sequalae for the Trust were a patient recently discharged from hospital to spread COVID-19 to their family and / or vulnerable adult cohabitants due to lack of clear self-isolation guidance.
An urgent collaboration between the urology team and the Trust IT department was undertaken to upgrade the Trust’s existing eScript discharge summary software.
Two new tabs were integrated:
1. COVID-19 test result [Figure 1] and date [Figure 2]: Positive / Negative / Not tested
2. Self-isolation advice [Figure 3]: No / Yes (please specify as free text)
Completion was made mandatory prior to being able to sign-off the document for printing and successful upload on the electronic records.
Figure 1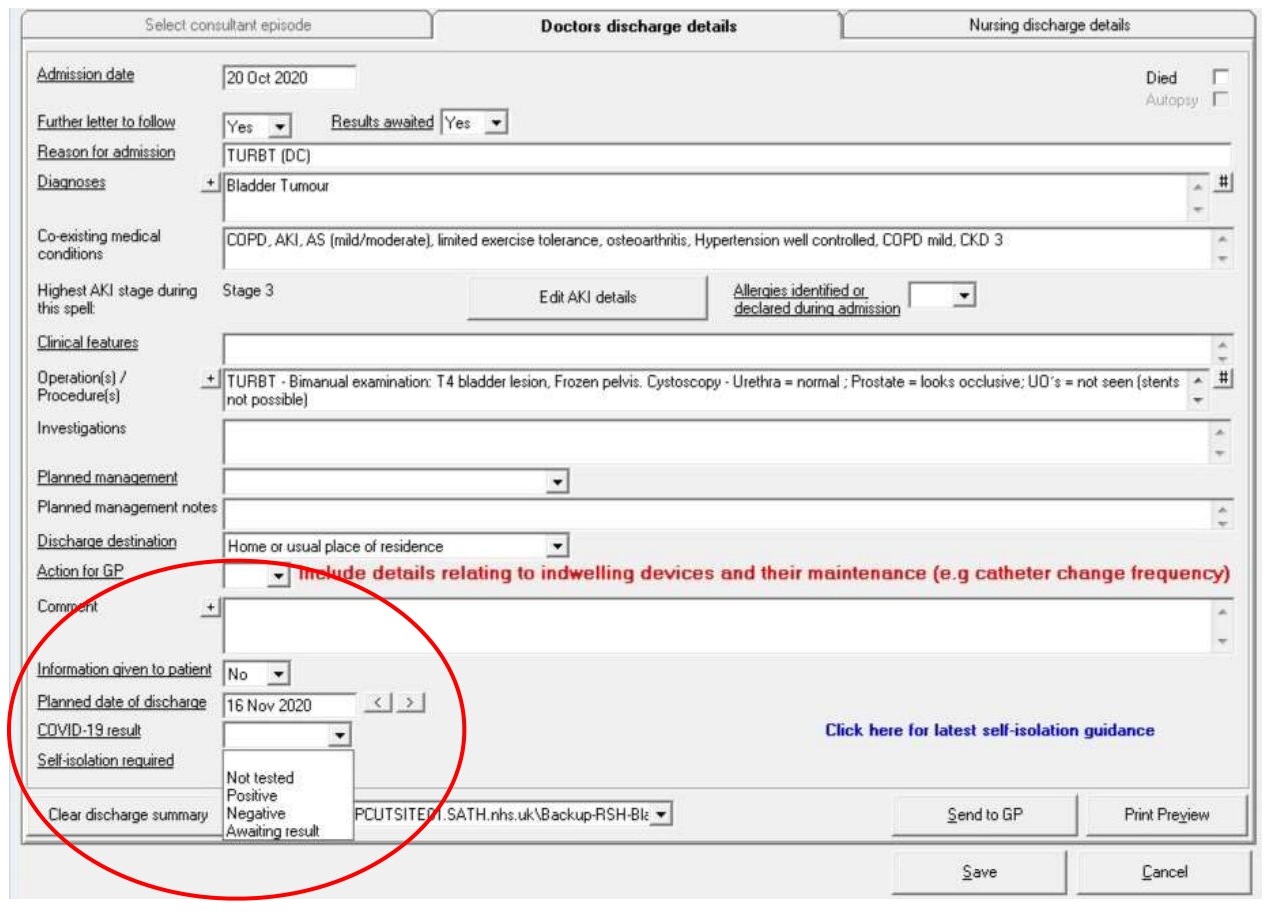
Figure 2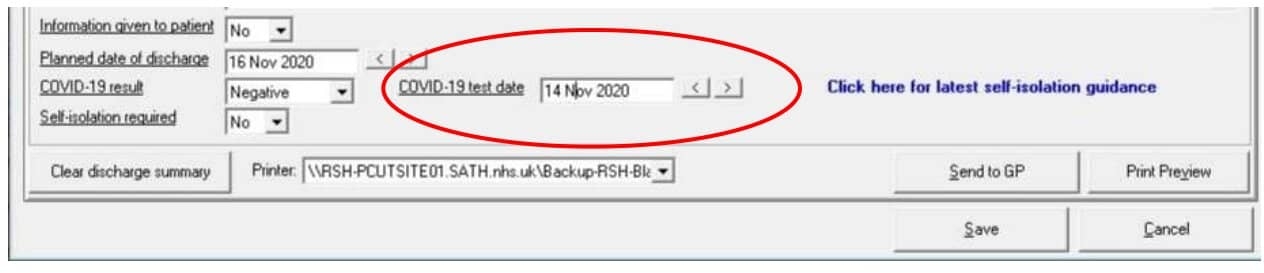
Collaboration with the infection prevention team (IPT) was undertaken to create a flow-chart style document accessible by hyperlink [Figure 3] to help discharging clinicians correctly determine and document patient self-isolation instructions following discharge from hospital, depending on individual circumstances. [Appendix 1]
Figure 3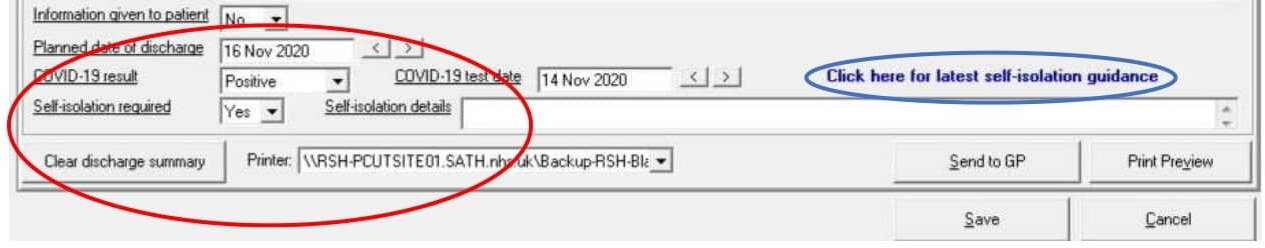
The aim of this quality improvement project was to evaluate the impact of the dynamic upgrade made to the eScript discharge summary software in clinician compliance with COVID-19 related documentation.
Materials and Methods
The upgraded eScript discharge summary software was rolled out across the Shrewsbury and Telford NHS Trust (SATH) in the week beginning 28th September 2020.
All clinicians were informed regarding the upcoming software change by means of a Trust-wide email from the SATH Medical Director, with instructions provided on how to complete the new tabs.
The first 50 consecutive completed discharge summaries of patients admitted electively or as emergency under the urology team starting from 1st October 2020 were retrospectively reviewed by NL, EF, ZK by means of electronic records.
Note was taken of correct documentation of:
· any COVID-19 test outcome (positive or negative result)
· any recommended patient self-isolation advice after discharge from hospital
The findings were compared and contrasted with the results of the initial study in April 2020.
Results
49 / 50 (98%) patients had a COVID-19 test at any time during their admission – 1 patient did not have a COVID-19 test at any time in their admission.
3 patients were discharged prior to their COVID-19 result becoming available, 1 patient was discharged without a written discharge summary and 1 patient was incorrectly labelled as having been “not tested.”
46 patients’ results therefore became available in time before discharge and 44 (90% of all those tested) were documented on their discharge summary. All COVID-19 tests were negative. [Table 1]
All patients had either documented self-isolation advice or “none required” specified on their discharge summary following discharge from hospital. [Table 1]
The most common primary reasons for admission were urinary tract infection / sepsis (18%), catheter-related complications (14%) and urinary retention (12%).
Incidental note was made of two patient deaths within 28 days of admission.
Table 1
| Initial Review | Review after software update | |
| Number of patients | 50 | 50 |
| Patients tested for COVID-19 | 33 (66%) | 49 (98%) |
| Patients testing positive | 1 (3.3%) | 0 (0%) |
| COVID-19 result on discharge summary | 9 (27%) | 44 (90%) |
| Self-isolation advice on discharge summary | 1 (2.0%) | 50 (100%) |
Discussion
The results revealed that the upgraded eScript software resulted in a notable improvement in COVID-19 related documentation on discharge summaries.
In the initial study 33 / 50 (66%) had a COVID-19 test at any time during their admission – only 27% of these however had the result included on their discharge summary, compared to 90% compliance following the eScript software upgrade.
Following the finding of 3 patients’ (6%) COVID-19 result not becoming available prior to discharge, SATH IT was consulted and an extra option on the eScript COVID-19 result dropdown menu was added to include “awaiting result” to mitigate for this particular circumstance. [Figure 1]
Only 1 patient (2%) in the initial study had any self-isolation advice documented on their discharge summary – this figure soared to 100% following the eScript software upgrade. [Table 2]
The figures have to be interpreted in light of the change in COVID-19 testing availability, which only became widespread in mid-May 2020 and thus after the completion of the initial study3. This is likely to account for the lower proportion of in-patient COVID-19 tests being performed in the initial study (66%) vs. second study (98%).
Arguably a negative COVID-19 result such as those commonly encountered on the urology ward are less likely to be documented on a discharge summary compared to a positive test, particularly if admitted with unrelated pathologies (e.g. urinary retention) or asymptomatic carriers. By nonetheless documenting this pertinent negative, one ensures the patient is aware of their reassuring result and any community-based clinician such as district nurse or GP can be cognisant of this information if called to assess the patient soon after hospital discharge.
The findings of the study are directly relevant to all doctors working in acute NHS Trusts, as clear and accurate documentation is a key principle in the GMC’s “Good Medical Practice” document to which all registered practising doctors must abide to4. A discharge letter is a key component of the documentation of a patient’s journey and therefore must be completed accurately in line with GMC guidance. The updated software system safeguards the accuracy and clarity of the Trust’s discharge summaries in relation to COVID-19 results and self-isolation advice.
Self-isolation is a key principle of outbreak control for any infectious disease, and is a particularly important strategy in managing widespread vast numbers of cases such as in the COVID-19 pandemic in a libertarian society where strict quarantine is not routinely enforced5. The adherence with self-isolation has been notoriously poor in the UK – it is estimated that only 25% of symptomatic patients with proven COVID-19 complied fully with the government advice of not leaving the home during their isolation period6. It is therefore of paramount importance that patients being discharged from hospital in the COVID-19 pandemic era are given clear instructions on how to self-isolate and the recommended duration of this is documented.
Doctors preparing discharge summaries and their patients must be aware that COVID-19 may still be relevant to them even if the primary reason for admission was unrelated and their test on admission was negative – for example they may have been exposed to another in-patient or staff member later found to be positive for the virus. The discharging clinician should check for any such event and disclose this on the discharge summary where applicable.
From a medicolegal perspective, hospitals trusts may find themselves in a vulnerable position if COVID-19 positive or potentially exposed patients are discharged without any documented self-isolation advice. This in particular follows the controversy highlighted in the earlier months of the pandemic of thousands of elderly patients being discharged from hospital to care homes in the UK without a COVID-19 test7. Indeed, since then a judge has allowed legal action from a bereaved daughter to be brought against the Department for Health and Social Care, NHS England and Public Health England for failure to adequately protect vulnerable residents in an Oxfordshire care home8. Safeguarding the clear documentation of recommended patient self-isolation instructions on discharge summaries is likely to confer additional protection to a Trust facing any such legal challenge.
Writing a high-quality discharge summary is a difficult skill to teach and indeed they are often completed by the most junior members of the medical team9. The Trust’s IT software can therefore play a vital role in helping doctors ensure that COVID-19 result and self-isolation instructions are documented for all hospital discharges, by means of mandatory tabs for completion prior to sign off.
To our knowledge, although other Trusts have since similarly amended their discharge summary software in light of the COVID-19 pandemic, this is the only study in the literature which directly attests the degree of improvement in documentation as a result of such a software change. We urge that all Trusts in the UK consider amending their discharge summary software in line with the changes characterised in this study.
Conclusions
The updated eScript discharge summary software has greatly improved compliance within the Trust with COVID-19 test result and self-isolation advice documentation on discharge summaries.
This is a simple and highly effective modification whose benefits can have ramifications across the healthcare system.
By accurately documenting COVID-19 test results and any advised self-isolation for the patient after hospital discharge, one safeguards IPC in the community and protects the Trust from potential relevant medico-legal sequalae.
Appendix 1
Scenario 1: COVID-19 positive patient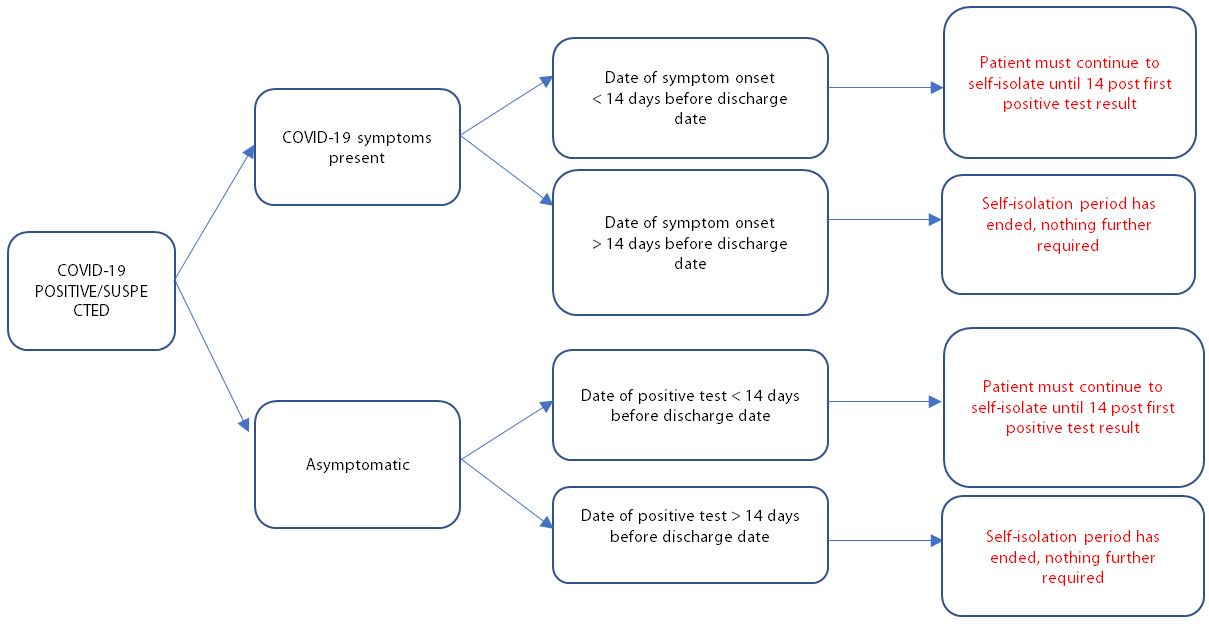
Scenario 2: COVID-19 negative patient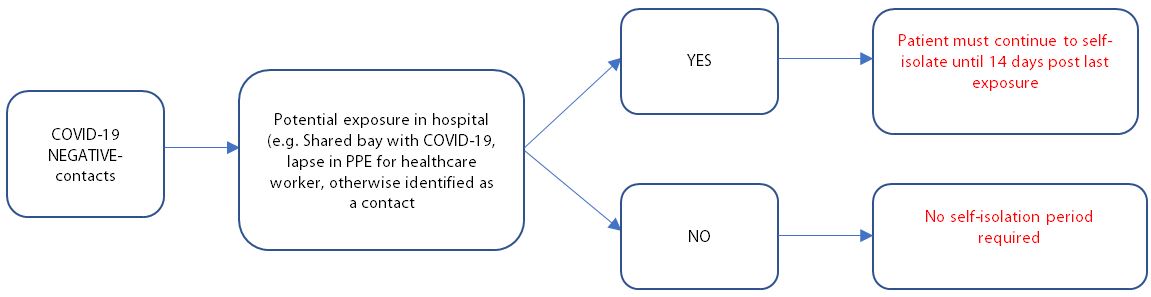
Scenario 3: No COVID-19 test performed as rubbish and make someone else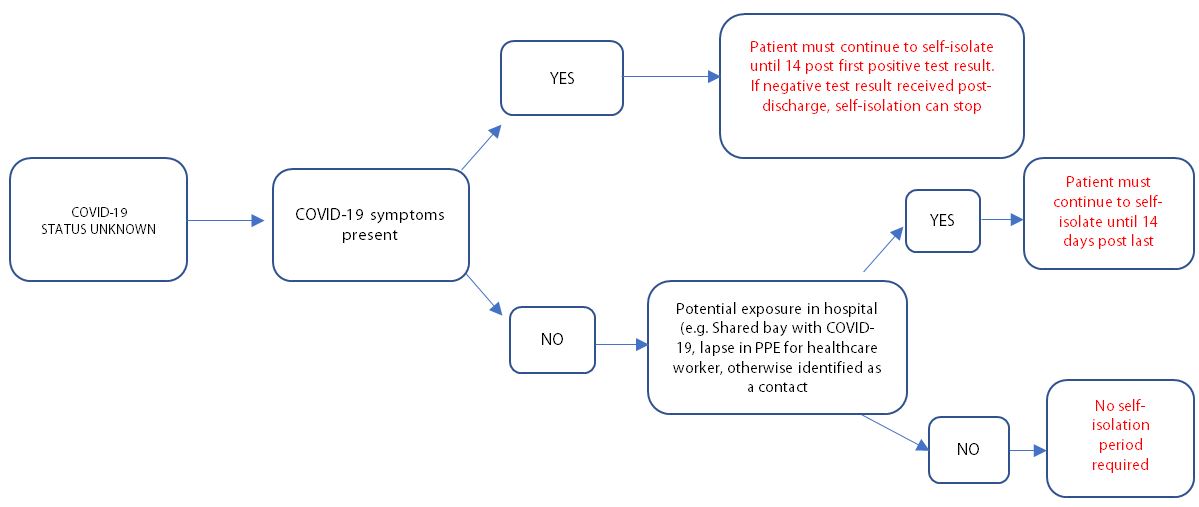
|
Acknowledgements The authors wish to thank Dr Arne Rose, Mr Mark Cheetham, Pete McGinness, Ashley May, Joe Thelwell, Angela Lewis and Kelly Pardy for the completion of this project. Competing Interests None declared Author Details JACK DONATI-BOURNE, FRCS(Urol), Royal Shrewsbury Hospital, Mytton Oak Rd, Shrewsbury SY3 8XQ, UK. NING LO, MBChB, Royal Shrewsbury Hospital, Mytton Oak Rd, Shrewsbury SY3 8XQ, UK EAMONN FOLEY, MBChB, Royal Wolverhampton Hospital, Wolverhampton Road, Wolverhampton, WV10 0QP, UK. ZAIN KASMANI, MBChB, Worcestershire Acute Hospitals NHS Trust, Woodrow Drive, B98 7UB, Redditch, UK. MASILAMANI SELVAN, FRCS(Urol), Royal Shrewsbury Hospital, Mytton Oak Rd, Shrewsbury SY3 8XQ, UK. JONATHAN O'DAIR, FRCS(Urol), Royal Shrewsbury Hospital, Mytton Oak Rd, Shrewsbury SY3 8XQ, UK. CORRESPONDENCE: JACK DONATI-BOURNE, Urology Department, Royal Shrewsbury Hospital, Mytton Oak Rd, Shrewsbury SY3 8XQ, UK. Email: jack.donati-bourne@nhs.net |
References
- Lillie PJ, Samson A, Li A, et al. Novel coronavirus disease (Covid-19): the first two patients in the UK with person to person transmission. J Infection 2020, 80(5), 578-606.
- Martín-Sánchez FJ, Del Toro E, Cardassay E, et al. (2020) Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department. Eur geriatr med 2020, 11(5), pp.829-841.
- Surkova E, Nikolayevskyy V, Drobniewski F. False-positive COVID-19 results: hidden problems and costs. Lancet Resp Med 2020, 8(12), pp.1167-1168.
- General Medical Council, “Good Medical Practice” [2013]. Available at: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice
- Salathé M, Althaus CL, Neher R, et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss med weekly 2020, 150(11-12), 1-3
- Rubin GJ, Smith LE, Melendez-Torres GJ, et al. Improving adherence to ‘test, trace and isolate’. J Royal Soc Med 2020, 113(9), pp.335-338.
- BBC (British Broadcasting Corporation) (2020) Coronavirus: sending untested patients to care homes “reckless” – MPs. [Cited 30 December 2020] Available at: https://www.bbc.co.uk/news/uk-politics-53574265
- BBC (British Broadcasting Corporation) (2020) Covid: Judge allows legal challenge into care home deaths. [Cited 30 December 2020] Available at: https://www.bbc.co.uk/news/uk-england-devon-55007355
- Myers JS, Jaipaul CK, Kogan JR, et al. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med 2006, 81(10), pp.S5-S8

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




