An Unusual Cause of Chronic Dyspnoea
Fadi Seif and Lamia H. Ibrahim
Cite this article as: BJMP 2011;4(1):a408
|
A 73 year old lady presented for assessment of her recurrent right sided pleural effusion. She had a history of gallstones and underwent open cholecystectomy. One month after surgery the patient had recurrent pleural effusion requiring thoracocentesis on a monthly basis. On the chest x-ray, the pleural effusion was seen exclusively on the right side occupying the whole right hemithorax.
The pleural fluid was transudative on multiple occasions and there was no evidence of malignant cells. Her echocardiography revealed preserved cardiac function. An abdominal ultrasound showed findings of cirrhosis and splenomegaly consistent with portal hypertension.
.jpg)
Image 1
Computerised tomography (CT) of the chest and abdomen revealed a large right-sided pleural effusion and minimal ascites (Image 1). An ultrasound guided paracentesis was performed with difficulty and only 17cc of fluid.was obtained. The abdominal fluid showed similar consistency as the pleural fluid. The blood workup at the same time was unremarkable.
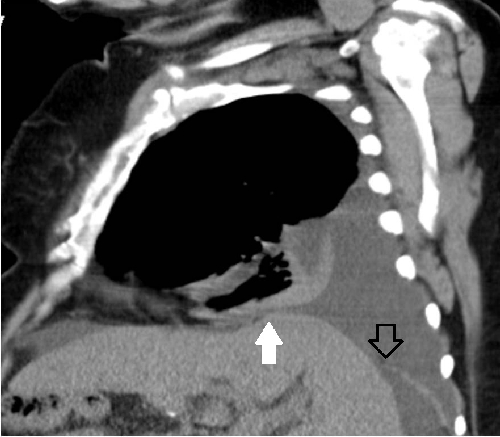
Image 2
Intra-peritoneal administration of 99mTc-sulphur colloid was attempted but failed in the absence of ascites. Computed tomography with three dimensional reconstruction at the diaphragmatic level revealed a defect in the posterior aspect of the right hemidiaphragm (Image 2 black arrow) and also revealed irregular contours of the liver, an indirect sign of diaphragmatic defect (Image 2 white arrow).
The patient declined any surgical intervention at that point including the option of pleurodesis. She was started on diuretics and a low salt diet with significant improvement.
Discussion:
Pleural effusion due to hepatic cirrhosis and ascites is well known, but hepatic hydrothorax in the absence of ascites is a rare complication. We report a case of liver cirrhosis with a large and recurring right sided pleural effusion that had an apparent abdominal source in the absence of ascites. We review the characteristics and treatment for hepatic hydrothorax in the absence of ascites.
Hepatic hydrothorax is defined as the presence of significant pleural effusion in a cirrhotic patient without primary pulmonary or cardiac disease1. Postulated mechanisms for the development of pleural effusions in patients with hepatic cirrhosis include: hypoalbuminemia and decreased oncotic pressure leakage of the plasma from the hypertensive azygos vein, lymphatic leak from the thoracic duct, passage of ascitic fluid to the pleural space by way of lymphatic channels in the diaphragm, and transfer of peritoneal fluid directly via diaphragmatic defects2.
The usual unilaterality of hepatic hydrothorax could be attributed to a congenital factor, but not to physiologic mechanisms3. The most likely explanation appears to be that ascitic fluid passes through congenital or acquired fenestrations in the diaphragm directly into the pleural space2. The description of hepatic hydrothorax in the absence of ascites is very rare1. The flow of the ascitic fluid into the pleural space equaled the rate of ascites production in patients with this entity3.
The composition of pleural fluid from hepatic hydrothorax is similar to that of ascitic fluid. Pleural effusions associated with portal hypertension are always transudative1. Nuclear scans can be performed to establish the diagnosis of hepatic hydrothorax with fairly high accuracy. Intra-peritoneal administration of 99mTc-human serum albumin or 99mTc-sulphur colloid can be used to demonstrate the communication between the peritoneal and pleural space. Recent advances in radiological imaging have enabled investigators to examine in detail the diaphragmatic defects responsible for the development of hepatic hydrothorax1.
The management is challenging and frequently associated with poor outcomes in most cases. Dietary restriction of sodium intake and the addition of diuretics is the initial approach. Thoracocentesis can be performed in patients with dyspnoea due to hepatic hydrothorax for immediate relief of symptoms. When thoracocentesis is required too frequently in patients on maximal sodium restriction and optimal diuretics, alternative treatment options must be considered1, 3.
Over the last few years, new insights into the pathogenesis of this entity have lead to improved treatment modalities such as portosystemic shunts (TIPS) and video-assisted thoracoscopy (VATS) for closure of diaphragmatic defects. Both, though temporary measures, are perhaps the best available bridging to liver transplantation in selected patients with refractory hepatic hydrothorax2, 3.
|
Competing Interests None declared Author Details Fadi Seif, M.D. Fellow, Pulmonary Critical Care and Sleep Medicine, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine Lamia H. Ibrahim, M.D., FCCP, Director of Asthma Center, Director of Medical Student and Resident Pulmonary Education, Division of Pulmonary, Critical Care and Sleep, University Hospitals Case Medical Center. Assistant Professor of Medicine, Case Western Reserve University School of Medicine, Louis Stokes Cleveland VAMC CORRESPONDENCE: Fadi Seif, M.D. Fellow, Pulmonary Critical Care and Sleep Medicine, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine Email: Fadi.Seif@UHhospitals.org |
References
- Kiafar C, Gilani N. Hepatic hydrothorax: Current concepts of pathophysiology and treatment options. Annals of Hepatology 2008; 7(4): 313-320
- Mentese BB, Kayhan B, Görgül A, et al. Hepatic Hydrothorax in the Absence of Ascites. Report of Two Cases and Review of the Mechanism. Digestive Diseases and Sciences 1997; 42(4): 781-788
- Gur C, Ilan Y, Shibolet O. Hepatic hydrothorax – pathophysiology, diagnosis and treatment – review of the literature. Liver International 2004; 24(4): 281-284

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




