Tuberculosis presenting as Costochondritis: a rare case report and brief review of literature
Manzoor Ahmad Wani, Naveed Nazir Shah, Syed Quibtiya Khursheed, Khurshid Ahmad Dar, and Asma Bashir
Cite this article as: BJMP 2016;9(2):a913
|
|
Abstract Mycobacterium tuberculosis can affect almost any part of the body. Although tuberculosis of the bones is well known, tuberculosis involving the cartilages is rarely described. We report a 30 year male, who presented with insidious onset pain and swelling of the right lower parasternal area which on evaluation was diagnosed as tubercular infection of costochondral junction. The patient had no evidence of tuberculosis anywhere else in the body. Thoracic wall tuberculosis is rare and primary tubercular costochondritis has been very rarely reported in the literature. Keywords: Mycobacterium tuberculosisAbbreviations: ESR - Erythrocyte Sedimentation Rate, ECG - Electrocardiogram, AFB - =Acid Fast Bacilli CT=Computed Tomography FNAC=Fine needle aspiration Cytology |
Introduction
Tuberculosis is an important and major infectious disease worldwide, especially in developing countries with an estimated global case fatality rate of 13% in 2007. The World Health Organization estimated that there were 13.7 million prevalent cases of TB infection worldwide, with each year bringing about 9.27 million new cases, 44% of which are new smear-positive cases1. Musculoskeletal tuberculosis is rare, chest wall tuberculosis is rarer and involvement of costochondral junction is among the rarest forms of tuberculosis. Tubercular costochondritis usually presents with insidious onset non-specific pain and swelling, resulting in delay in the diagnosis. Diagnosis is usually made by typical radiological findings and microbiological and histological evidence of tuberculosis. Treatment consists of antitubercular therapy with or without surgery.
Case report
30 year male, smoker, from low socio economic status presented with history of low grade fever, malaise and anorexia which began gradually two months back. For about one month he had pain in right side of chest just adjacent to lower part of sternum. The pain had started insidiously, gradually worsened with time, and was dull and aching in character. Pain was localized to the right lower parasternal area, occasionally radiating to the back. The pain was aggravated by physical activity and deep inspiration and was relieved to some extent by ordinary anti- inflammatory medications. There was significant history of pulmonary tuberculosis in the patient’s sister 1 year ago. There was no history of cough, haemoptysis, fever with chills or history of tuberculosis in the past.
On general physical examination, the patient was weak and febrile. On local examination, there was a bulge in the right lower parasternal area, corresponding to the right 9th costochondral junction. On palpation, there was severe tenderness in the same area. There was no peripheral lymphadenopathy and abdomen was soft and non-tender with no organomegaly. Chest examination was unremarkable. The rest of the examination was normal.
In terms of investigations, the chest radiograph, ECG, haemogram, kidney function tests and liver function tests were normal. ESR was high (34), Mantoux test was positive(15mm). Sputum for AFB was negative. Axial CT chest demonstrates expansion of the left 9th costal cartilage with soft tissue thickening on both the inner and outer aspect of the cartilage (Fig.1). FNAC (Fine Needle Aspiration Cytology) of the costochondral junction revealed Mycobacterium tuberculosis and on culture and histopathology of aspirated material revealed tubercular granuloma (Fig.2). A final diagnosis of tubercular costochondritis was made and the patient was treated with anti tubercular drugs for 9 months. Patient's symptoms improved after 2 weeks of treatment and swelling and tenderness subsided. Post treatment axial CT demonstrated complete resolution of soft tissue abnormality previously seen around the costal cartilage (Fig.3).
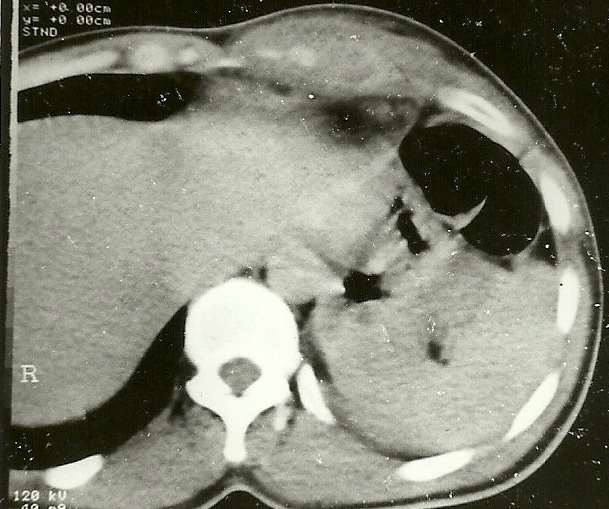
Figure 1: CT chest showing evidence of costochondritis.
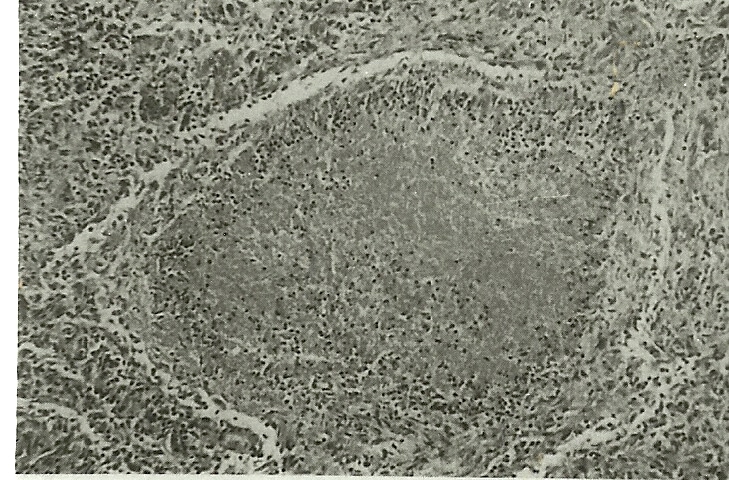
Figure 2: Typical tubercular granuloma with central caseous necrosis on histopathology.
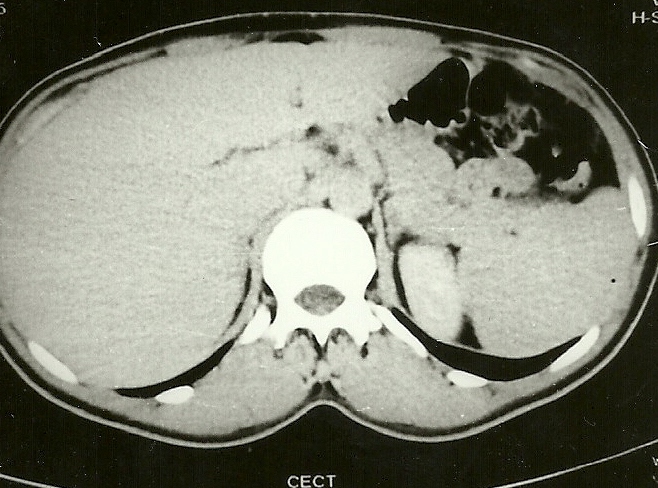
Figure 3: Post ATT CT showing complete resolution of costochondritis.
Discussion
Tuberculosis is very common infectious disease in developing countries like India, resulting in significant morbidity and mortality. Musculoskeletal tuberculosis is relatively uncommon and accounts for 1 to 2% of all the tuberculosis patients2,3 and accounts for about 10% of all extrapulmonary TB infections4. Tuberculosis of the chest wall constitutes 1 to 5% of all cases of musculoskeletal TB5,6. TB abscesses of the chest wall are usually seen at the margins of the sternum and along the rib shafts, and can also involve the costochondral junctions, costovertebral joints and the vertebrae7. In one study8, on the basis of the part of the rib involved, the roentgenographic findings for patients with rib tuberculosis was divided into four categories: Costovertebral (35%), Costochondral (13%),Shaft (61%), and Multiple cystic bone. TB of the thoracic wall is usually caused by reactivation of some latent foci of primary tuberculosis formed during hematogenous or lymphatic dissemination but direct extension from contiguous mediastinal lymph nodes can also occur9. In developing countries such as ours, tuberculosis is endemic and all the rare forms of the disease have been described, but in developed countries, resurgence of tuberculosis due to HIV may be responsible for atypical presentations .
Thoracic wall tuberculosis mostly presents insidiously with pain and swelling, but the diagnosis of chest wall TB is often delayed due to lack of specific symptoms and signs and gradual course10. Approximately less than 50% of chest wall TB patients may have active pulmonary TB11,12. Imaging techniques like X-Rays and CT scan play an important role in diagnosis and follow up of these patients. According to a study done by Vijay YB et al13, radiological signs may not be present initially at the time of presentation with symptoms, abscesses or sinuses may be present much before the imaging modalities detect them. Computed tomography (CT) scan is more valuable for localization and detection of bone destruction and soft tissue abnormalities. Atasoy et al demonstrated the role of Magnetic Resonance Imaging (MRI) for early detection of marrow and soft tissue involvement in sternal tuberculosis due to high contrast resolution of MRI14.Diagnosis is usually confirmed by finding acid fast bacilli (AFB) and positive AFB cultures of bone (positive in up to 75% of cases), and caseous necrosis and granuloma on histopathology11.
Complications of thoracic wall tuberculosis include secondary infection, fistula formation, spontaneous fractures of the sternum, compression or erosion of the large blood vessels, compression of the trachea and migration of tuberculosis abscess into the mediastinum, pleural cavity or subcutaneous tissues as discharging sinus. Chest wall TB needs to be differentiated from benign and malignant tumors [chondroma, osteochondroma, fibrous dysplasia, lipoid granuloma, chondrosarcoma, myeloma multiplex]11, metastatic carcinoma, lymphoma or other kinds of infection15,16.
The treatment of choice of chest wall TB is still not clear. Whether antitubercular therapy alone or surgical debridement (or excision based on lesion extension) combined with antitubercular therapy should be done needs further studies. But the general rule is if there are any complications, surgery is the treatment of choice followed by antitubercular therapy. We conclude that the diagnosis of thoracic wall tuberculosis is a challenge for physicians and is suspected by gradual onset clinical features and confirmed by microbiology, histopathology and radiography findings. Early diagnosis and treatment are important to prevent complications caused by bone and joint destruction.
|
Competing Interests None declared Author Details MANZOOR AHMAD WANI, DM resident, Department of Gastroenterology, SKIMS, Srinagar, India. NAVEED NAZIR SHAH, Assistant professor, Chest Diseases Hospital, Government Medical College, Srinagar, India. SYED QUIBTIYA KHURSHEED, Registrar, Department of General Surgery, Government Medical College, Srinagar, India. KHURSHID AHMAD DAR, Lecturer, Chest diseases hospital, Government Medical College, Srinagar, India. ASMA BASHIR, PhD scholar, Kashmir University, Srinagar, India. CORRESPONDENCE: MANZOOR AHMAD WANI, MBBS, MD, DM resident, Department of Gastroenterology, SKIMS, Srinagar, India. Email: drmanzoorahmadwani@gmail.com |
References
- World Health Organization Global tuberculosis control – epidemiology, strategy, financing: WHO Report 2009. http://www.who.int/tb/publications/global_report/2009/en/index.html.
- Garcia S, Combalia A, Serra A, Segur JM, Ramon R. Unusual locations of osteoarticular tuberculosis. Arch Orthop Trauma Surg 1997; 116:321-3.
- Chang DS, Rafii M, McGuinness G, Jagirdar JS. Primary multifocal tuberculous osteomyelitis with involvement of the ribs. Skeletal Radiol 1998; 27:641-5.
- Reider HL, Snider DE Jr, Cauten GM: Extrapulmonary tuberculosis in the United States. Am Rev Respir Dis 1990, 141:347-351.
- Gayler BW, Donner MW. Radiographic changes of the ribs. Am J Med Sci 1967; 253:586-619.
- Mathlouthi A, Ben M'Rad S, Merai S, Friaa T, Mestiri I, Ben Miled K et al. Tuberculosis of the thoracic wall. Presentation of 4 personal cases and review of the literature. Rev Pneumol Clin 1998; 54:182-6.
- Morris BS, Varma R, Garg A, Awasthi M, Maheshwari M. Multifocal musculoskeletal tuberculosis in children: appearances on computed tomography. Skeletal Radiol 2002; 31:1-8.
- Tatelman M, Drouillard EJP. Tuberculosis of the ribs. Am J Roentgenol 1953;70:923-35.
- Iwata Y, Ishimatsu A, Hamada M, Emori M, Ikedo Y, Wakamatsu K, et al. A case of cervical and mediastinal lymph nodes tuberculosis, tuberculous pleurisy, spinal caries and cold abscess in the anterior chest wall. Kekkaku 2004;79:453-7.
- Newton P, Sharp J, Barnes KL: Bone and joint tuberculosis in greater Manchester 1969-1979. Ann Rheum Dis 1982, 41:1-6.
- Agrawal V, Joshi MK, Jain BK, Mohanty D, Gupta A: Tuberculotic osteomyelitis of rib-a surgical entity. Interact Cardiovasc Thorac Surg 2008, 7:1028-1030
- Asnis DS, Niegowska A: Tuberculosis of the rib. Clin Infect Dis 1997, 24:1018-1019.
- Vijay YB, Vinod A, Umesh S, Anubhav G. Primary tuberculous sternal osteomyelitis: a clinical rarity. Asian Cardiovasc Thorac Ann 2009;17:310-2.
- Atasoy C, Oztekin PS, Ozdemir N, Sak SD, Erden I, Akyar S. CT and MRI in tuberculous sternal osteomyelitis: a case report. Clin Imaging 2002;26:112-5.
- Chang GH, Kim SK, Lee WY: Diagnostic issues in tuberculosis of the ribs with a review of 12 surgically proven cases. Respirology 2009, 4:249-253.
- Ormerod LP, Grundy M, Rahman MA: Multiple tuberculosis bone lesions simulating metastatic disease. Tubercle 1989, 70:305-307.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




