Sustainability and sleep management in psychiatric wards
Maria Donnelly, Nieves Mercadillo & Stuart Davidson
Cite this article as: BJMP 2020;13(2):a009
|
|
Abstract Insomnia is a disturbance of normal sleep patterns. It is characterised by sleep onset latency and/or sleep maintenance. Short term insomnia is defined as having symptoms for less than 4 weeks, whilst long term insomnia is symptoms lasting more than 4 weeks. Hypnotics including the benzodiazepine and non-benzodiazepine (Z-drugs) can provide relief from the symptoms of insomnia; they do not treat any underlying cause. NICE guidance states “After consideration of the use of non-pharmacological measures, hypnotic drug therapy is considered appropriate for the management of severe insomnia interfering with normal daily life, it is recommended that hypnotics should be prescribed for short periods of time only, in strict accordance with their licensed indications”. They also advise to use the lowest effective dose for the shortest period possible. Side effects are common with hypnotic usage. This includes most importantly developing tolerance and rebound insomnia. The aim of our project is to reduce hypnotic prescribing for patients on an Acute inpatient psychiatric ward. The ward is a Male ward containing 17 inpatient beds in the Northwest of England. The patients are 18 years onward with varying diagnosis. The reason for doing this project was most importantly for improving patient safety via reduction of unnecessary prescriptions and administration of medications, but also for cost and carbon footprint reduction of the NHS. Patients included in this project were inpatients on the selected ward between the 09/12/2020-20/01/2020 and 28/01/2020-10/03/2020. The interventions used to fulfil our aims included development of an educational presentation about Insomnia and sleep management, development of an Insomnia management flow chart to be used at admission point and at weekly reviews (Appendix 1), training session for ward staff, patient sleep hygiene and management educational sessions, face to face and email correspondence to inform medical trainees about this project and gathering feedback from patients and staff before and after this project. The data we collected included the specific Hypnotic medication, dose and quantity prescribed on the ward during these dates. With our interventions we have demonstrated a 44.5% reduction in hypnotic administration. This highlights the positive change the interventions have resulted in. This will improve patient safety by reducing the risk of side effects, and by reducing the number of patients being discharged on a regular prescription which will further reduce long term costs of hypnotic medications for the NHS. The small changes that we have applied have resulted in a massive improvement in our clinical care and patient safety, with the added benefit of a reduction in the pharmaceutical environmental impact that over prescribing can result in. Keywords: Insomnia; Sleep Hygiene; Hypnotics; Benzodiazepines; Rebound insomnia; Tolerance; Flow chart; Pharmaceutical impact; Carbon footprintAbbreviations: NICE: The National Institute for Health and Care Excellence |
Introduction
Insomnia is a disturbance of normal sleep patterns. It is characterised by sleep onset latency and/or sleep maintenance. Short term insomnia is defined as having symptoms for less than four weeks, whilst long term insomnia is symptoms lasting more than four weeks1. Hypnotics can provide relief from the symptoms of insomnia; they do not treat any underlying cause.
Several hypnotic agents are licensed for the treatment of insomnia, including the benzodiazepines and Non-benzodiazepine hypnotics (Z-drugs)2.
NICE guidance for Insomnia management states “After consideration of the use of non-pharmacological measures, hypnotic drug therapy is considered appropriate for the management of severe insomnia interfering with normal daily life; it is recommended that hypnotics should be prescribed for short periods of time only, in strict accordance with their licensed indications” 1.
NICE guidance also advises to use the lowest effective dose of the hypnotic agent for the shortest time frame possible. The exact duration will depend on the underlying cause, but treatment should not continue for longer than two weeks. We should also inform the patient that further prescriptions for hypnotics will not usually be given, ensure that the reasons for this are understood, and document this information in the patient’s notes.
Side effects are common with hypnotic usage including, most importantly, the development of tolerance and rebound insomnia. Other side effects can occur such as daytime sedation, poor motor coordination, cognitive impairment, hallucinations, anxiety, delusions and sleep disorders2.
Aims
To reduce the amount of hypnotic medication being prescribed to patients on an Acute Inpatient psychiatric ward in the Northwest of UK. The ward is in a semirural psychiatric hospital and is a Male ward containing 17 inpatient beds. The patients are 18 years old onwards with varying diagnosis including Generalised Anxiety Disorder, Bipolar Affective Disorder, Schizophrenia, Depression, and patients with mental and behavioural disorders due to psychoactive substance use.
The reason for doing this project was most importantly for improving patient safety by reducing unnecessary prescriptions and therefore administration of hypnotic medications, but also to reduce NHS expenditure and carbon footprint.
Inclusion criteria
Patients who have been an inpatient on the selected ward between the 09/12/2020-20/01/202 and 28/01/2020-10/03/2020.
Intervention
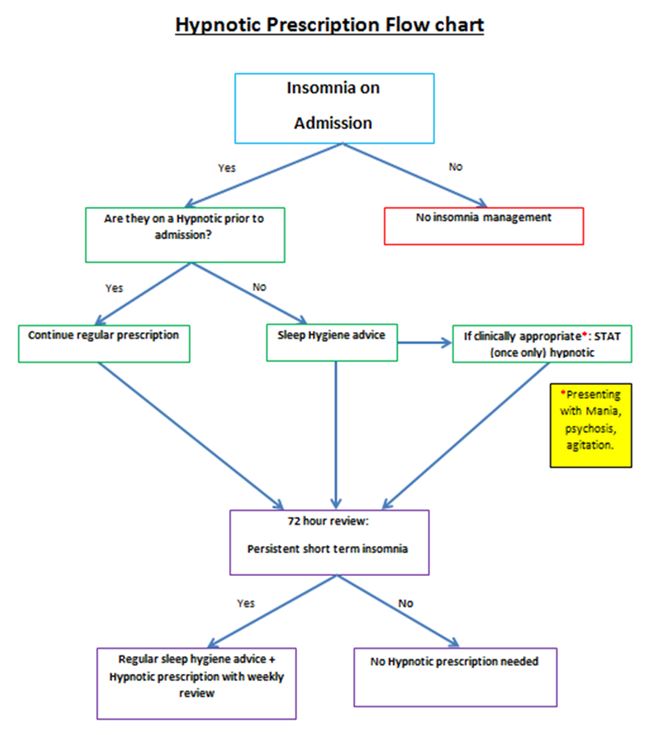
We developed a prescription aid flow chart (Appendix 1) for all newly admitted patients to the ward. This will guide doctors when making the decision if a hypnotic prescription is warranted.
All patients on the ward during this intervention period, who are currently on a hypnotic agent and are not newly admitted, will have their hypnotic prescription reviewed using the flow chart (Appendix 1) at their weekly consultant ward round.
We then decided on some interventions to fulfil our aims. The interventions were as follows:
1) Development of an educational presentation about Insomnia and sleep management.
2) Development of an Insomnia management Flow chart (Appendix 1) to be used at admission point.
3) Training sessions for ward staff.
4) Shared teaching programme with patients at their sleep management sessions.
5) Face to face and E-mail correspondence to inform medical trainees about this project.
6) Gather feedback from ward patients and staff before and after this project.
The Hypnotic prescription flow chart aid (Appendix 1), has been put on the ward office notice board, the clinic room and the On Call Doctors Room. It was also e-mailed out to the regular ward doctors, as well as all on-call doctors working during the intervention period.
As discussed above, we created an educational PowerPoint presentation entitled “Insomnia and hypnotic agents”. This included insomnia definitions and types, NICE guidance on insomnia, sleep hygiene advice, the medications used for insomnia, their mode of actions, side effects, cautions and cost of these medications. We also included our new hypnotic prescription flow chart aid (Appendix 1).
From the 21/01/2020-27/01/2020 we had two of these educational training sessions. This was to ensure that all staff working on this ward attended at least one of these sessions. Staff in attendance included the ward managers, nursing staff, health care assistants, the pharmacist, a junior doctor, and the ward consultant. This was very important as all these health care professionals are involved with the management of patients on the ward, and those suffering from insomnia. We felt that this session was vital as we wanted to ensure that all the staff knew the importance of this project and could raise their own concerns and issues that they have with regards to managing patients with insomnia. This proved to be very useful as we all brainstormed and voiced some realistic ward changes that could happen on an inpatient psychiatric ward. We also acknowledged that sleeping on the ward as an inpatient can often be disturbed, due to regular nursing checks and noise from the staff and other patients. We did however discuss some feasible interventions which included:
1) The time at which all the automatic ward lights are turned on in the morning could be delayed.
2) Caffeine –free coffee/tea available only after a particular time in the evening.
3) Discourage daytime napping.
4) Have regular sleep-hygiene sessions on the ward.
Between 28/01/2020 to the 10/03/2020 we started these interventions, and this is the time period for collection of our next six weeks of data. We had multiple patient group sessions on sleep hygiene during this time led by the occupational therapist. Other health professionals assisted with this, including the ward pharmacist and the junior doctor. During these sessions we asked for patients to give their feedback on the current management of insomnia on the ward. Some responses included:
· One patient with Severe Generalised Anxiety Disorder stated that he feels that the sleep hygiene advice is helpful, as he doesn’t like to “jump straight into taking tablets” and likes to “fix the root” of his sleeping problem.
· A second patient with a diagnosis of Mental and Behavioural Disorder due to use of cannabinoids, stated that he needs both sleeping medications and sleep hygiene advice, as sometimes he still cannot get to sleep on the ward by solely using relaxation methods.
· A third patient with Generalised Anxiety Disorder stated that he found the sleep hygiene sessions useful. He is now using relaxation methods and is trying to avoid daytime naps which are both helping with his sleep. However, he still on occasions struggles with sleep. He said it is important to have a tidy, clean and relaxing sleeping environment, which is sometimes difficult to implement on the ward.
Appendix 1
Results:
Data was collected prior to any intervention on the ward between the dates 09/12/2020 and 20/01/2020.
The table below (Table No.1) includes the type and number of sleeping tablets prescribed on the ward between the dates 09/12/2020 and 20/01/2020. The total number of patients treated from 9 December 2019 to 20 January 2020 were 28 and the total number of patients were prescribed hypnotic medication during this time were 14.
Table No.1 - Hypnotic medication prescribed:
| Name | dose | Number of tablets |
| Zopiclone | 7.5mg | 191 |
| Zopiclone | 3.75mg | 12 |
| Zolpidem | 10mg | 4 |
| Nitrazepam | 5mg | 7 |
| Temazepam | 10mg | 10 |
The table below (Table No.2) includes the number of hypnotics prescribed and administered after the interventions mentioned above. The total number of patients treated from 28 January 2020 to 10 March 2020 were 25 and the total number of patients who had prescribed hypnotic medication were 11.
Table No. 2- Hypnotic medication prescribed:
| Name | dose | Number of tablets |
| Zopiclone | 7.5mg | 96 |
| Zopiclone | 3.75mg | 6 |
| Zolpidem | 10mg | 0 |
| Nitrazepam | 5mg | 0 |
| Temazepam | 10mg | 0 |
With our ward interventions we have significantly reduced the amount of hypnotic tablets being administered. The total number of tablets administered during this 6 week period was 102. The total number of patients who were prescribed hypnotics was 11. Prior to our interventions the total number of tablets administered between 9th December 2019 and 20th January 2020 was 224 and 14 patients in total were treated. This demonstrates a 44.5% reduction in tablets which is significant.
Discussion
The total reduction in tablet administration was very significant with a 44.5% reduction post-intervention. This demonstrates the positive change in our clinical practice that has resulted from using the flow chart aid (Appendix 1) as well as patient and staff educational and feedback sessions. This will improve patient safety by reducing the risk of side effects. The risk of patients developing tolerance to hypnotic medications has been reduced, as well as reducing those being discharged on a regular prescription which will further improve long term expenditure of hypnotic medications for the NHS. With the changes that have occurred in our clinical practice, we have reduced the number of hypnotics being unnecessarily prescribed and administered.
Over prescribing/unnecessary prescribing is an issue within the NHS and is impacting negatively on the environment. The NHS constitution states that the NHS is ‘committed to providing the most effective, fair and sustainable use of finite resources’3. By reducing the number of inpatients being unnecessarily started on hypnotic medications, another positive from this project will be the reduction in the negative pharmaceutical impact on the environment. The number patients being discharged with hypnotic medications, who may no longer need them, due to their insomnia improving when they are discharged from the inpatient setting will also improve. Furthermore, if they are unnecessarily started on a hypnotic prescription as an inpatient, they may continue this prescription regularly and become tolerant, which will inevitably have an undesirable effect on the environment.
The feedback that we received from the educational insomnia teaching sessions also proved to be very useful. As stated above the staff sessions allowed us to brainstorm simple ward-based interventions, as well as discussing possible drawbacks which may result. This allowed us to modify the flow chart so that it worked for all staff effectively.
The feedback given from patients was also very encouraging. As health professionals we sometimes overlook how some patients want and need more involvement in making decisions on aspects of their care. Ensuring patients are informed about medications prior to prescribing, especially about side effects is something that is very important and allows patients to make informed decisions which is a more holistic approach to clinical practice. This is vitally important prior to prescribing any medications but especially medications with more severe side effects which some hypnotics have.
The patient educational sessions were a key part of this project. We gathered feedback and established that the patients involved found these sessions informative. Some, but not all, of the sleep hygiene advice was feasible to implement into their daily routine on the ward. The ward can be disruptive at night, due to other patients, or due to regular staff checks in patient rooms, as well as rooms not being familiar surroundings, were two of the difficulties raised from the patients. This is something that we appreciate can’t be changed, however with the interventions that can be feasibly made on the inpatient psychiatric ward, we continue to strive to implement and improve for patients. For these reasons both the staff and the patient educational sessions should be continued and proved a vital part of this project
Following on from this initial intervention, we feel that we can continue to make further changes and expand the changes we made on this ward, to other similar wards in our hospital and to other inpatient psychiatric wards in the Trust.
|
Competing Interests None declared Author Details MARIA DONNELLY, FY1 Doctor, Warrington General Hospital WA5 1QG UK. NIEVES MERCADILLO, Consultant Psychiatrist, Hollins Park Hospital WA28WA UK. STUART DAVIDSON, Senior Pharmacist, Hollins Park Hospital WA28WA UK. CORRESPONDENCE: NIEVES MERCADILLO, Consultant Psychiatrist, Hollins Park Hospital WA28WA UK. Email: maria.donnelly3@nhs.net |
References
- Insomnia - NICE CKS [Internet]. Cks.nice.org.uk. 2020 [cited 13 May 2020]. Available from: https://cks.nice.org.uk/insomnia
- Excellence N. Hypnotics and anxiolytics | Treatment summary | BNF content published by NICE [Internet]. Bnf.nice.org.uk. 2020 [cited 13 May 2020]. Available from: https://bnf.nice.org.uk/treatment-summary/hypnotics-and-anxiolytics.html
- Sustainability Development Unit for Public Health UK. Reducing the Use of Natural Resources in Health and Social Care [Internet]. Sustainable Development Unit for NHS UK and Public Health UK; 2020. Available from: https://www.sduhealth.org.uk/documents/Policy%20and%20strategy/20180912_Health_and_Social_Care_NRF_web.pdf

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




