A survey of aseptic technique when performing lumbar puncture: a comparison of medical and anaesthetic trainees
Rajiv Malhotra and Sara Kelly
Cite this article as: BJMP 2012;5(1):a503
|
|
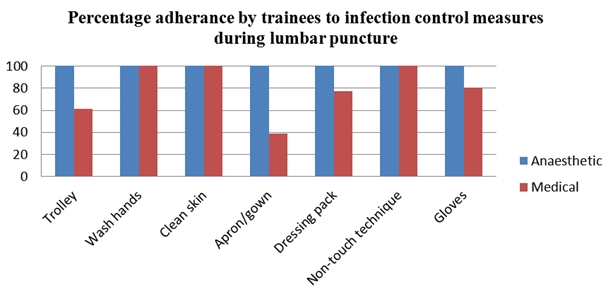
Abstract Aim:To compare infection control measures taken by anaesthetic and acute medical trainees when performing lumbar puncture. Methods:An online anonymous survey was sent to 50 anaesthetic and 50 acute medical trainees currently in training posts. Information on compliance with infection control measures was gathered. Results:The response rate was 71% (40/50 anaesthetic trainees, 31/50 medical trainees). All anaesthetic trainees complied with the components of aseptic technique. In comparison to this, only 80.6% of medical trainees used sterile gloves, 38.7% used an apron and 77.4% used a dressing pack. Conclusions:Levels of infection control during lumbar puncture differ between anaesthetic and medical trainees, particularly with the use of equipment as part of an aseptic technique. The difference is likely to be due to a combination of factors including training and the clinical environment. |
Introduction
Lumbar punctures are commonly performed by both medical and anaesthetic trainees but in different contexts. Medically performed lumbar punctures are often used to confirm a diagnosis (meningitis, subarachnoid haemorrhage) whilst lumbar puncture performed by anaesthetists are usually a precedent to the injection of local anaesthetics into cerebrospinal fluid for spinal anaesthesia. The similarity relies on the fact that both involve the potential for iatrogenic infection into the subarachnoid space. The incidence of iatrogenic infection is very low in both fields; a recent survey by the Royal College of Anaesthetists1 reported an incidence of 8/707 000 whilst there were only approximately 75 cases in the literature after ‘medical’ lumbar puncture.2 However, the consequences of iatrogenic infection can be devastating. It is likely that appropriate infection control measures taken during lumbar puncture would reduce the risk of bacterial contamination. The purpose of the present study is to compare infection control measures taken by anaesthetic and medical staff when performing lumbar puncture.
Method
A survey was constructed online (www.surveymonkey.com) and sent by email to 50 anaesthetic and 50 acute medical trainees in January 2011. All participants were on an anaesthetic or medical training programme and all responses were anonymous. The survey asked whether trainees routinely used the following components of an aseptic technique3 when performing lumbar puncture:
- Sterile trolley
- Decontaminate hands
- Clean patient skin
- Apron/gown
- Dressing pack
- Non-touch technique
- Sterile gloves
No ethical approval was sought as the study was voluntary and anonymous.
Results
The overall response rate was 71% (40/50 anaesthetic trainees and 31/50 medical). All anaesthetic trainees routinely used the components of an aseptic technique when performing lumbar puncture. All medical trainees routinely cleaned the skin, decontaminated their hands and used a non-touch technique but only 80.6% used sterile gloves. 61.3% of medical trainees used a sterile trolley, 38.7% used an apron/gown and 77.4% used a dressing pack.
Discussion
This survey shows that adherence to infection control measures differ between anaesthetic and medical trainees when performing lumbar puncture. The anaesthetic trainees have a 100% compliance rate compared to 80% for the medical trainees for all components of the aseptic technique. Both groups routinely cleaned the patient’s skin, decontaminated their hands and used a non-touch technique. However, there were significant differences in the use of other equipment, with fewer medical trainees using sterile gloves, trolleys, aprons and dressing packs.
Although the incidence of iatrogenic infection after lumbar puncture is low, it is important to contribute to this low incidence by adopting an aseptic technique. There may be differences with regards to the risks of iatrogenic infection between anaesthetic and medical trainees. Anaesthetic lumbar punctures involve the injection of a foreign substance (local anaesthesia) into the cerebrospinal fluid and may therefore carry a higher risk. Crucially however, both anaesthetic and medical lumbar punctures involve accessing the subarachnoid space with medical equipment and so the risk is present.
There are many reasons for the differing compliance rates between the two specialties. Firstly, anaesthetic trainees perform lumbar punctures in a dedicated anaesthetic room whilst the presence of ‘procedure/treatment rooms’ is not universal on medical wards. Secondly, anaesthetic trainees will always have a trained assistant present (usually an operating department practitioner, ODP) who can assist with preparing equipment such as dressing trolleys.
The mechanism of iatrogenic infection during lumbar puncture is not completely clear.4 The source of microbial contamination could be external (incomplete aseptic technique, infected equipment) or internal (bacteraemia in the patient); the fact that a common cause of iatrogenic meningitis are viridans streptococcus strains5 (mouth commensals) supports the notion that external factors are relevant and an aseptic technique is important.
It is very likely that improved compliance amongst acute medical trainees would result from a dedicated treatment room on medical wards, but this is likely to involve financial and logistical barriers. The introduction of specific ‘lumbar puncture packs’, which include all necessary equipment (e.g. cleaning solution, aprons, sterile gloves) may reduce the risk of infection; the introduction of a specific pack containing equipment for central venous line insertion reduced colonisation rates from 31 to 12%.6 The presence of trained staff members to assist medical trainees when performing lumbar puncture may assist in improved compliance, similar to the role of an ODP for anaesthetic trainees.
The main limitation of this study is that the sample size is small. However, we feel that this study raises important questions as to why there is a difference in infection control measures taken by anaesthetic and medical trainees; it may be that the environment in which the procedure takes place is crucial and further work on the impact of ‘procedure rooms’ on medical wards is warranted.
|
Competing Interests None declared Author Details RAJIV MALHOTRA ST4 Anaesthetics, MB ChB, FRCA, Department of Anaesthetics, Royal Liverpool University Hospital, Prescot Street, Liverpool, L7 8XP. SARA KELLY CT1 Anaesthetics, MB ChB, Department of Anaesthetics, Warrington Hospital, Lovely Lane, Liverpool, WA5 1QG. CORRESPONDENCE: RAJIV MALHOTRA ST4 Anaesthetics, Department of Anaesthetics, Royal Liverpool University Hospital, Prescot Street, Liverpool, L7 8XP. Email: rajivmalhotra1@hotmail.com |
References
1. Cook T, Counsell D, Wildsmith JAW et al. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth. 2009;102 (2):179-190.
2. Baer ET. Iatrogenic meningitis: the case for face masks. Clin Infect
Dis 2000; 31: 519-521.
3. Rowley S, Clare S. ANTT: a standard approach to aseptic technique. Nurs Times. 2011; 107: 12-14.
4. Baer ET. Post-dural puncture bacterial meningitis. Anesthesiology.
2006;105 (2): 381-393.
5. Yaniv LG, Potasman I. Iatrogenic meningitis: an increasing role for resistant viridans streptococci? Case report and review of the last 20 years. Scand J Infect Dis. 2000; 32 (6): 693-696.
6. Mukerji S, Daniels R, Maung K, Mattin A. Central venous catheter related infection: a cohort study evaluating dedicated central venous catheter packs. Critical Care.2009; 13 (4): 22.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




