A Study On Clinical Features And Cost Incurred By Dengue Syndrome Patients Admitted To Tertiary Care Hospital
Manjunath M N, Chaithanya C Nair and Sharanya R
Cite this article as: BJMP 2015;8(2):a811
|
|
Abstract Background: India is one of the seven identified countries in Southeast Asia regularly reporting dengue fever (DF)/dengue haemorrhagic fever (DHF) outbreaks. India may soon transform into a major niche for dengue infection in the future with more and more new areas being struck by dengue epidemics. Objectives: 1) To study the clinical manifestations, trends and outcomes of all confirmed dengue cases admitted to a tertiary care hospital. 2) To study the cost incurred by these patients during hospital stay. Materials and Methods: This record-based study was conducted on 757 serologically (NS1 Ag/ IgM/ IgG) positive dengue cases admitted to KIMS Hospital & Research Centre, Bangalore during January 2012 to December 2012. Required data from the entire laboratory confirmed cases were collected from the Medical Records Department (MRD) and analysed. Results: The seropositive case rate for dengue was 61.5% with NS1 antigen\ IgM\ IgG. Males were commonly affected and the most vulnerable age group was found to be between 5 to15 years of age. The median age was 8 years. The percentage of cases presented as dengue fever without warning signs was 88.5%, the remaining being dengue with warning signs and severe dengue. Fever was the most common symptom seen followed by vomiting and abdominal pain. Haemorrhagic manifestations were seen in about 4.5% of cases of which majority presented with petechiae followed by haematemesis. The mortality rate was 8.6%. Conclusion: Increased awareness, better transport facilities and case management according to the WHO guidelines is needed to further reduce mortality and cost burden of dengue cases. Abbreviations: DF - Dengue Fever, DHF - Dengue Haemorrhagic Fever, DSS - Dengue Shock Syndrome, ARDS - Acute Respiratory Distress Syndrome, MODS - Multiple Organ Dysfunction Syndrome. |
Introduction:
Dengue made its debut as early as 1780, when Benjamin Rush described the condition as “break bone fever”. This hitherto unfamiliar infection has now grown to demand the attention of all public health care providers. It is a mosquito borne, fast emerging, viral infection manifesting in four serotypes (1). Approximately 2.5 billion people, living mainly in urban areas of tropical and subtropical regions, are estimated to be at risk of acquiring dengue infection (2). While dengue is endemic in more than 100 countries, most cases are reported from Southeast Asia and the western Pacific regions. Around 50 million cases and 24,000 deaths are estimated to occur in these 100 endemic countries. This includes hospitalisation of nearly half a million cases of dengue haemorrhagic fever (DHF), of which 90% are children. Treated (DHF)/dengue shock syndrome (DSS) is associated with a 1% mortality rate while mortality rate among untreated cases escalates to 20%(3,4).
India is one of the seven identified countries in the Southeast Asia region regularly reporting incidence of DF/DHF outbreaks. The first confirmed report of dengue infection in India dates back to 1940s, and since then more and more new states have been reporting the disease which mostly strikes in epidemic proportions often inflicting heavy morbidity and mortality, in both urban and rural environments.(5)
The various manifestations of dengue may not have a distinct line of demarcation: apart from the classic features, reports of rare presentations have recently become more frequent (6,7). During recent outbreaks in India, the clinical manifestations which were shown by the patients were slightly different from those in previous years(8).. There have been many reports of difficulties in the use of the previous classification, which were summarised in a systematic literature review (9). Difficulties in applying the criteria for dengue haemorrhagic fever in the clinical situation, together with the increase in clinically severe dengue cases which did not fulfil the strict criteria, led to the request for the classification to be reconsidered .Hence, WHO revised the dengue case classification into dengue (with or without warning signs), and severe dengue (10).The present study was done to analyse the clinical features, complications, cost incurred and outcome of cases admitted to a tertiary care teaching hospital in Bangalore.
Methodology:
A record based descriptive study was conducted in paediatric patients admitted with signs and symptoms suggestive of dengue fever to KIMS hospital Bangalore, during the period between January 2012 to December 2012. SD BioLine kit was used for testing with NS1 antigen\ IgM\ IgG. The medical records were perused for collecting data about these cases using a pre-designed proforma. Data was analysed for the clinical presentations, outcome and direct cost incurred in respect to hospital charges and laboratory investigations.
Results:
Out of 1230 cases admitted with clinical signs and symptoms suggestive of dengue syndrome 757 (61.5%) cases were found to be NS1 antigen\ IgM\ IgG positive for dengue. Among the 757 positive cases, males were 499 (65.9%) and females 258 (34.1%). The majority of the cases were in the school going age group and this consisted of 310 cases (41%) and adolescent children which accounted for 249 cases (33%), the median age being 8 years of age. The least number of cases were seen in infants which accounted for 45 cases (6%).
Table 1. Sex distribution
| Age group | Male | Female | Total |
| Infant | 31 | 14 | 45 |
| Toddler | 114 | 39 | 153 |
| School going | 208 | 102 | 310 |
| Adolescent | 146 | 103 | 249 |
| TOTAL | 499 (65.9%) | 258(34.1%) | 757 |
The majority, 88.5% of cases presented as dengue fever without warning signs, 6.34% with dengue fever with warning signs and 5.15% with severe dengue. Of the cases with warning signs 92.3% of cases had fever, 42.5% cases had vomiting and 38.2% cases had abdominal pain. Haemorrhagic manifestations were seen in about 4.5% of cases of which majority (87%) presented with petechiae followed by haematemesis (9%) and epistaxis (4%). Rashes were seen in 4% and arthralgia in 13% of cases. Pleural effusion was seen in 21% of cases and ascites was seen in 16% of cases. Complications in the form of acute respiratory distress syndrome (ARDS) was seen in 12.06% cases, 6% cases showed neurological manifestations in the form of encephalopathy and 1.3% cases had renal failure.
Table 2. Severity of dengue
| SEVERITY | PERCENTAGE |
| DF without warning signs | 88.5 |
| DF with warning signs | 6.3 |
| Severe dengue | 5.15 |
Table 3. Presenting complaints
| Presenting Complaints | Number (%) |
| Fever | 699(92.3) |
| Myalgia | 148(19.5) |
| Haemorrhagic manifestations | 34(4.5) |
| Vomiting | 321(42.5) |
| Abdominal pain | 289(38.1) |
| Headache | 201(26.5) |
| Arthralgia | 99(13) |
| Diarrhoea | 80(10.5) |
| Others | 121(16) |
Fig 1 presenting complaints.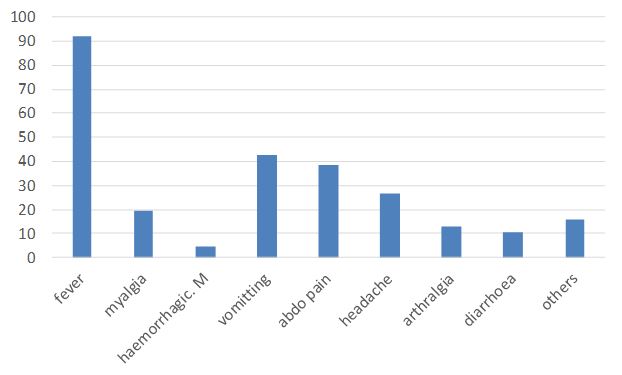
Haemoglobin level of > 12gm% was found in 73.4% cases, 9-12gm% in 23.4%, 6-9gm% in 2.1% and <6 gm% in 1.1% of cases. Platelet count of < 20,000 was found in 21.5% of cases, 20-50 thousand in 39.5% , 50,000 to 1.5 lakh in 36% of cases and >1.5 lakh was found in 3% of cases. Majority (65.5%) of cases were NS1 Ag positive alone or with IgM/ IgG/ or both positive.
Remaining were positive for either of the antibodies.13.7% cases werepositive for all the three i.e. Ag, IgM,& IgG. The mortality rate was found to be 8.6%
Figure 2: outcome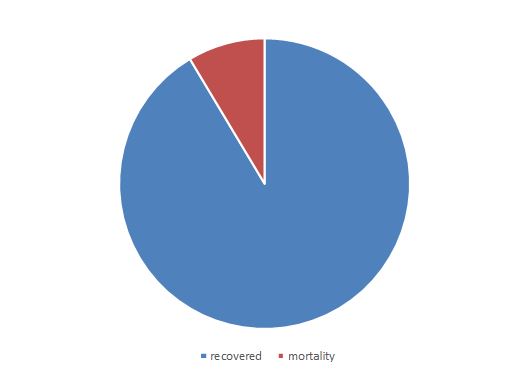
Cost incurred which includes direct cost (transporting patient to the hospital, diagnostic testing and laboratory investigations, medications, hospitalisation, food) was found to been average of Rs.12,611=00. The indirect cost loss of wages of patient &attendants) was found to be an average of Rs.3, 109=00. The hidden cost (out of pocket expenses) was found to be an average of Rs.50=00. The cost of treatment of other co-morbid conditions was found to be an average of Rs.2, 275=00. The total cost of treating dengue syndrome was 18,045=00
Discussion:
In the present study it was found that males were commonly affected and the most common age group was between 5 to 15 yrs of age. Similar results were reported in a study by Faridi et al, 76% of all cases of DHF /DSS were aged 6 years or more[11].
In the present study, the most common presenting symptoms was fever followed by vomiting and abdominal pain which is similar to study done by Kumar A et al showed fever in 99.2% followed by myalgia (64.6%), vomiting (47.6%), headache (47.6%) and abdominal pain (37.5%) (12).
In the present study, the most common bleeding manifestation was haematemesis and epistaxis. In a study by Ratageri et al, common bleeding manifestations were gastrointestinal bleeding (22%) and petechiae (18%) [13]. The gastrointestinal tract was reported as the commonest site of bleeding (61%) in a study by Ahmed et al [14].
In the present study majority of cases had platelet count between 20,000 to 50,000/mm3.In a study by Kamath et al, platelet counts less than 50,000/mm were noted in 62.3% [15]. In our study complicated cases showed ARDS and neurological manifestations in the form of encephalopathy. Almost all the cases which expired were found to have ARDS. Dengue associated ARDS is associated with a high mortality [16]. Dengue infection is found to cause neurological manifestation ranging from non-specific symptoms to encephalitis and rarely Guillain-Barre Syndrome [17]. In our study the mortality rate was found to be 8.6% , in the study by Anju et al overall mortality seen was 6% [18], compared to 3% by Ahmed et al [14].
Conclusion:
The seropositivity for dengue was 61.5% with NS1 antigen\ IgM\ IgG. Males were commonly affected and most vulnerable age group was found to be 5-15 year olds. The median age was 8 years. 88.5% of cases presented as dengue fever without warning signs, the remaining being dengue with warning signs and severe dengue. Fever was the most common symptom seen followed by vomiting and abdominal pain. Haemorrhagic manifestations were seen in about 4.5% of cases of which majority presented with petechiae followed by haematemesis. The mortality rate was 8.6%. Acute Respiratory Distress Syndrom (ARDS) and multiple organ dysfunction syndrome (MODS) was found to be the most dreadful complications with high rates of mortality .
In this study it was found that cost incurred which includes direct cost (transporting patient to the hospital, diagnostic testing and lab investigations, medications, hospitalisation, food) was found to bean average of Rs. 12,611=00. Thus dengue syndrome also causes significant economic burden on the patients.
In the recent few years, the world has seen varied clinical presentation of the dengue fever in different epidemics, even in the same regions and even with the period of time. Where some known features are still manifesting, few atypical features are noted from several parts of the world. A continuous seroepidemiological surveillance and timely interventions are needed to indentify the cases, so that its complications, outbreak and mortality can be minimised.
Moreover community awareness, early diagnosis and management and vector control measures need to be strengthened, especially during peri-monsoon period, in order to curb the increasing number of dengue cases.
|
Competing Interests None declared Author Details DR MANJUNATH M N, Fellow in Paediatric Critical Care, Narayana Hrudayalaya, Bangalore, India. DR CHAITANYA NAIR, Post Graduate, Kempegowda Institute of Medical Sciences, Bangalore, India. DR SHARANYA R, Post Graduate, Kempegowda Institute of Medical Sciences, Bangalore, India. CORRESPONDENCE: DR MANJUNATH M N, Fellow in Paediatric Critical Care, Narayana Hrudayalaya, Bangalore, India. Email: drmanju.drmanju@gmail.com |
References
- Guzmán MG, Kourí G. Dengue: An update. Lancet Infect Dis. 2002;2:33 42. [PubMed]
- Halstead SB (2007) Dengue. Lancet 370: 1644-1652
- WHO (2009) Dengue Guidelines for Diagnosis, Treatment, Prevention and Control WHO (2009) http://whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf. Last accessed 5 July 2012
- World Health Organization. Dengue and dengue haemorrhagic fever. Fact Sheet. No. 117, 2002. Available from: http//www.who.int/mediacentre/factsheets/fs117/en/ [last accessed on 2009 Dec 20]
- Dengue in Kerala: A critical review. ICMR Bulletin. 2006;36:13–22
- Gulati S and Maheshwari A (2007) Atypical manifestations of dengue. Trop Med Int Health 12: 1087-1095
- Misra UK, Kalita J, Syam UK, Dhole TN (2006) Neurological manifestations of dengue virus infection. J NeurolSci 244: 117-122
- SeemaA, SinghV, KumarS, KumarA, DuttaS. The Changing Clinical Spectrum of Dengue Fever in the 2009 Epidemic in North India: A Tertiary Teaching Hospital Based Study. Journal of Clinical and Diagnostic Research 2012 August; Vol-6(6): 999-1002
- Bandyopadhyay S, Lum LC, Kroeger A. Classifying dengue: a review of the difficulties in using the WHO case classification for dengue haemorrhagic fever. Tropical Medicine and International Health, 2006,11(8):1238–1255
- WHO Library Cataloguing-in-Publication Data Handbook for clinical management of dengue.1. Dengue – therapy. 2. Dengue – diagnosis. 3. Clinical medicine. 4. Handbooks. I. World Health Organisation. ISBN 978 92 4 150471 3 (NLM classification: WC 528)
- Faridi MMA, Aggarwal A, Kumar M, et al. Clinical and biochemical profile of Dengue haemorrhagic fever in children in Delhi. Trop Doct. 2008;38(1): 28-30
- Shah I, Deshpande GC, Tardeja PN. Outbreak of dengue in Mumbai and Predictive markers of dengue Shock Sydrome. J Trop Pediatr 2004; 50:301-305
- Ratageri VH, Shepur TA, Wari PK, et al. Clinical profile and outcome of dengue fever cases. Indian J Pediatr. 2005;72(8):705-6
- Ahmed S, Arif F, Yahya Y, et al. Dengue fever outbreak in Karachi 2006 - a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008;58(1): 4-8
- Kamath SR, Ranjit S. Clinical features, complications and atypical manifestations of children with severe forms of dengue hemorrhagic fever in South India. Indian J Pediatr. 2006;73(10):889-95
- Lum LC, Thong MK, Cheah YK et al. Dengue-associated adult respiratory distress syndrome. Ann Trop Pediatr.1995;15(4):335-9
- Garacia-Rivera EJ, Rigan-Perez JG. Encephalitis and dengue. Lancet 2002;360(9328):261
- Aggarwal A, Chandra J, Aneja S, et al. An epidemic of dengue hemorrhagic fever and dengue shock syndrome in children in Delhi. Indian Pediatr. 1998;35(8):727-32

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




