Solitary metastasis to the pancreas from colorectal cancer– A case report and literature review
Suvadip Chatterjee, John Scott, Viney Wadehra, Steve White and Manu Nayar
Cite this article as: BJMP 2012;5(2):a516
|
Introduction
Majority of pancreatic tumours are of primary pancreatic origin. Nevertheless a multitude of extra pancreatic cancers can metastasize to the pancreas and may present a diagnostic and management dilemma. Our case demonstrates such a problem in a patient with a pancreatic lesion.
Case report
A 82 year old man was referred to our hospital with computed tomogram (CT) scan showing a hypodense lesion in the pancreas. He had an anterior resection done 5 years prior for a Duke’s B (pT3N0M0) colon cancer. He did not receive any post-operative chemotherapy or radiotherapy. Carcinoembryonic antigen (CEA) levels was normal. He underwent an MRI scan (Figure 1) of his abdomen which reported a 2.8cm ring enhancing lesion in the tail of pancreas. At endoscopic ultrasound (EUS) a 2 x 2 cm well circumscribed mass was demonstrated in the tail of the pancreas close to the splenic artery but, not involving the vessel. Fine needle aspiration (FNA) of the lesion demonstrated a poorly differentiated mucin secreting adenocarcinoma. Immuno-histochemical staining was strongly positive for CK 20 but, CK 7 was only weak focally positive (Figure 2) thus, suggesting metastasis to the pancreas from a colonic primary as opposed to a primary pancreatic malignancy.
The patient was given an option to undergo subtotal pancreatectomy or consider palliative chemotherapy. The patient chose neither and was discharged home with input from the Macmillan team.
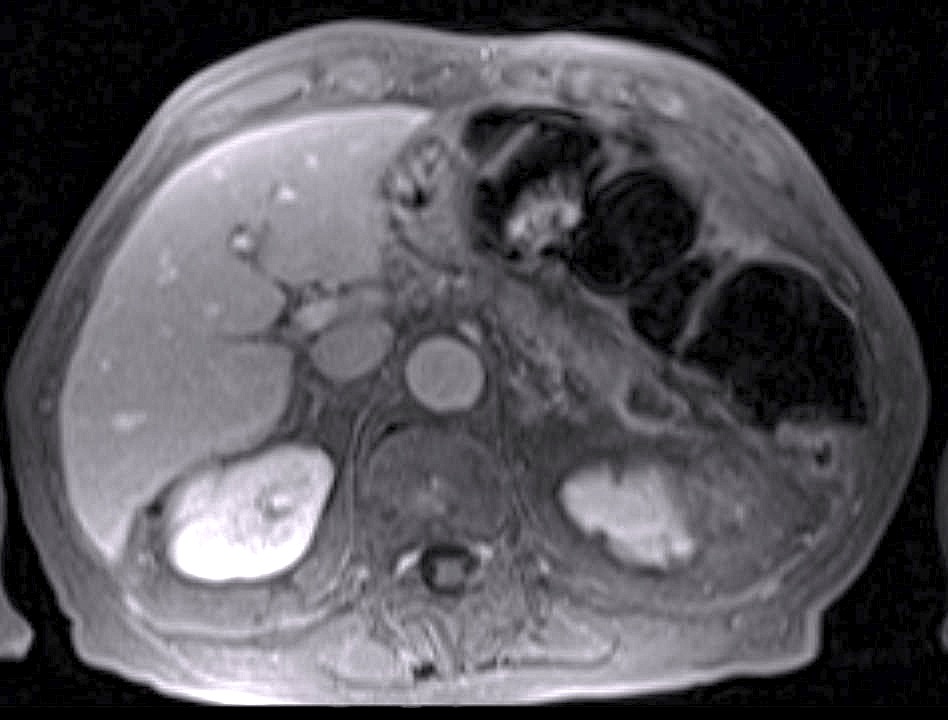
Figure 1: MRI after gadolinium showing a ring-enhancing lesion in the tail of pancreas.
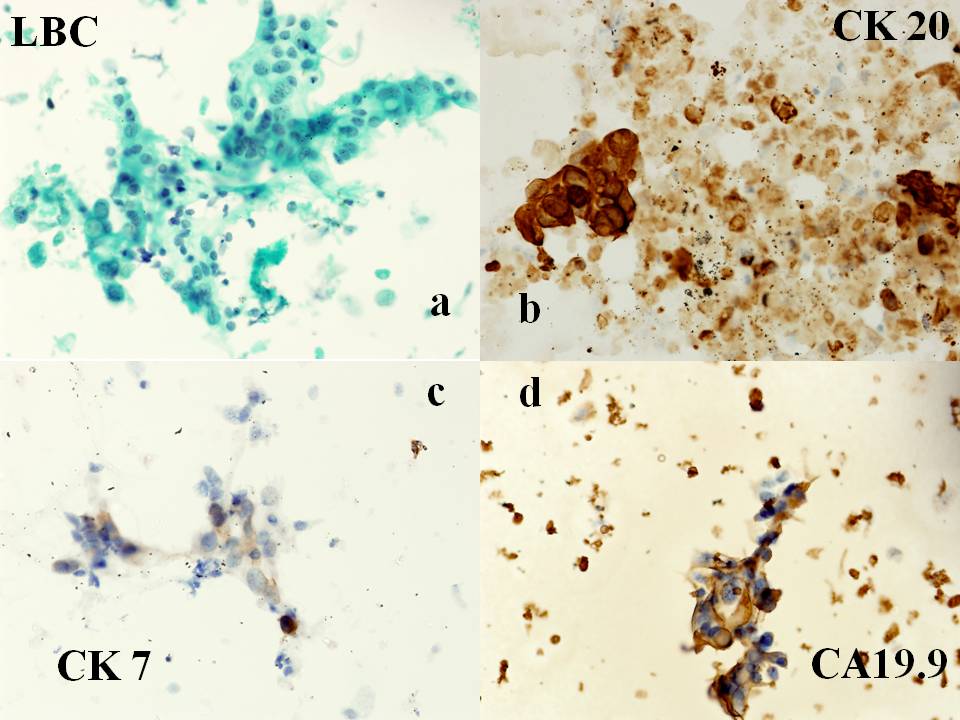
Figure 2: (a) Fine needle aspirate on liquid based cytology (x 400) shows irregular distribution of cells with nuclear palisading and pleomorphism. Immunocytochemistry performed on cytology smear shows (b) strong positivity for CK 20 (c) negative for CK7 and (d) focal positivity for CA19.9.
Discussion:
The pancreas is an uncommon site of metastasis from other primary cancers.1 Most of the space occupying lesions seen in the pancreas on imaging are of primary pancreatic origin.1, 2 Adsay, et al 2 performed analyses on surgical and autopsy database in 2004 and found that amongst a total of 4955 adult autopsies and 973 pancreatic specimens at surgery; the prevalence of different metastatic tumours to the pancreas was only 1.6% of all examined autopsy cases and 3.9% of pancreatic resections.
A study from Japan found that the commonest primary malignancies to metastasize to the pancreas were from the stomach, lung and bile duct in that order.3 Other primary tumours that have been reported to metastasize to the pancreas include renal cell carcinoma, lung, breast, small bowel, colon, rectum and melanoma.4, 5 Several mechanisms for development of pancreatic metastases (particularly from colorectal cancer) have been described: transfer via the lymphatic system, metastases from peritoneal carcinomatosis, and/or transfer via the haematogenous system. 6 Direct invasion of the pancreas by the primary tumour was also noted to be a method of spread from bile duct and gastric malignancies.3
CT scan is often unhelpful in differentiating primary from secondary pancreatic lesions. Pancreatic metastasis can present as solid or cystic structures, hypodense or hyper dense lesions.7, 8 A series by Klein, et al in which the CT features of pancreatic tumours are described suggested that multiplicity of tumours and/or hypervascularity were characteristic of secondary pancreatic tumours.9 A recent study has suggested that Positron Emission Tomogram (PET) is a more sensitive investigative tool than CT in detecting metastatic colorectal cancer.10 Most patients (as in our unit) usually have EUS guided FNA or biopsy to arrive at a diagnosis.
The differential diagnosis of primary pancreatic cancer versus metastasis from other carcinomas may be difficult using common histopathological techniques.11 Immuno-histochemical staining is often helpful in differentiating primary from secondary pancreatic tumours. Sometimes staining by a combination of different antibodies helps to reach a diagnosis. In a survey of 435 cases, the expression of CK 7 was positive in 92% of pancreatic cancers but in only 5% of colon cancers. On the other hand CK 20 was positive in 100% of colon cancers and in only 62% of pancreatic cancers.12 Furthermore, CD X2 is frequently expressed in colorectal carcinoma but, rarely in pancreatic ductal adenocarcinoma.13
The choice between conservative chemotherapy and resection for solitary pancreatic metastasis from colorectal cancer is still undecided. The natural history of untreated patients with pancreatic metastasis from cancer of the colon or rectum is unknown and thus it is impossible to compare the survival rate of resected and unresected patients treated with chemotherapy.14 Researchers from John Hopkins have reported only 4 colon metastasis to the pancreas (0.6%) among 650 pancreatico-duodenectomy procedures performed in their institution from 1990 to 1996.15 Experience from an Italian centre14 published that metastasis to the pancreas was the indication for surgery in a total of 18 out of 546 pancreatic resections (3.2%) performed over 27 years and colorectal cancer was the primary tumour in 50% of those cases. The median survival time was 16.5 months (range 8 – 105 months) with no peri-operative mortality being reported. In another study, all symptomatic (pain or jaundice) patients experienced complete relief of symptoms after surgery and no one experienced obstructive jaundice or abdominal pain until tumour recurrence.16
Oncologists may argue that chemotherapy can offer the same results as pancreatic resection but with less morbidity. Unfortunately, there is paucity of data in medical literature on comparisons of outcomes associated with surgical and chemotherapeutic treatment. We agree with Sperti et al 14 that resection of pancreatic metastasis from colorectal cancer is a palliative procedure with long-term survival being an exceptional event.
Conclusion:
Our case demonstrates that differential diagnoses for pancreatic masses should always include metastasis to the pancreas from other tumours particularly, when there is a history of previous or concurrent non-pancreatic malignancy. When disseminated malignancy is not present an aggressive surgical approach may offer successful palliation of symptoms and have a role in the multidisciplinary management of metastatic malignancy.
|
Competing Interests None declared Author Details SUVADIP CHATTERJEE, MD MRCP(UK), Advanced Endoscopy Fellow, HPB Unit, Freeman Hospital, Newcastle-upon-Tyne, UK. JOHN SCOTT, FRCR, Consultant Radiologist, Department of Radiology, Freeman Hospital, Newcastle-upon-Tyne, UK. VINEY WADEHRA, FRCPath, Consultant Cytopathologist, Department of Pathology, Freeman Hospital, Newcastle-upon-Tyne, UK. STEVE WHITE, FRCS PhD, Consultant HPB and Transplant Surgeon, HPB Unit, Freeman Hospital, Newcastle-upon-Tyne, UK. MANU NAYAR, MRCP, Consultant Gastroenterologist, HPB Unit, Freeman Hospital, Newcastle-upon-Tyne, UK. CORRESPONDENCE: SUVADIP CHATTERJEE, MD MRCP(UK), Advanced Endoscopy Fellow, HPB Unit, Freeman Hospital, Newcastle-upon-Tyne, UK. NE7 7DN Email: suvadip_chatterjee@yahoo.com |
References
- Hiotis SP, Klimstra DS, Conlon KC, Brennan MF: Results after pancreatic resection for metastatic lesions. Ann Surg Oncol 2002,9:675 – 679.
- Adsay NV, Andea A, Basturk O, Kilinc N, Nassar H, Cheng JD. Secondary tumours of the pancreas : an analysis of a surgical and autopsy database and review of the literature. Virchows Arch 2004;444:527 – 535.
- Nakamura E,Shimizu M,Itoh T,Manabe T. Secondary tumours of the pancreas :clinicopathological study of 103 autopsy cases of Japanese patients. Pathol Int 2001;51:686 – 90.
- Roland CF, Van Heerden JA. Non pancreatic tumours with metastasis to the pancreas.Surg Gynaecol Obstet 1989;168:345 – 347.
- Minni F,Casadei R,Perenze D,Greco VM,Marrano M,Margiotta A, Marrano D. Pancreatic metastasis : observations of three cases and review of the literature.Pancreatology 2004;4:509 – 20.)
- Shimoda M, Kuboata K, Kita J,et al. Is a patient with metastatic rectal cancer a candidate for resection ? A case report. Hepatogastroenterology 2007;54:1262 – 5.
- Chou YH, Chiou HJ,Hong TM,Tiu CM,Chiou SY, Su CH,Tsay SH. Solitary metastasis from renal cell carcinoma presenting as diffuse pancreatic enlargement. J of Clin Ultrasound 2002; 30:499 – 502.
- Kleef J,Freiss H,Buchler MW.What is the most accurate test to differentiate pancreatic cystic neoplasms ? Nat Clin Pract Gastroenterol Hepatol 2004;1:18 -9.
- Klein KA, Stephens DH,Welch TJ. CT characteristics of metastatic disease of pancreas. Radiographics 1998;18:369 – 78.
- Chou YH, Chiou HJ,Hong TM,Tiu CM,Chiou SY, Su CH,Tsay SH. Solitary metastasis from renal cell carcinoma presenting as diffuse pancreatic enlargement. J of Clin Ultrasound 2002; 30:499 – 502.
- Wente MN, Bergman F, Frohlich BE: Pancreatic metastasis from gastric carcinoma : a case report. World J of Surg Oncology 2004,2:43:1-4.
- Chu P, Wu E,weiss LM.Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasm : a survey of 435 cases. Mod Pathol 2000;13:962 – 72.
- De Lott LB, Morrison C,Suster S, Cohn DE,Frankel WL. CDX2 is a useful marker of intestinal-type differentiation : a tissue microarray-based study of 629 tumours from various sites.Arch Pathol Lab Med 2005;129:1100 -5.
- Sperti C, Pasquali C, Berselli M,Frison L, Vicario G, Pedrazzoli S. Metastasis to the pancreas from colorectal cancer : Is there a place for pancreatic resection ? Dis Colon rectum 2009;52:1154 – 1159.
- Yeo CJ, Cameron JL,Sohn TA,et al.Six hundred and fifty consecutive pancreaticoduodenectomies in the 1990s : a single centre experience and overview of literature.Pancreas 2005.;30:218 – 22.
- Crippa S, Angelini C, Mussi C,et al. Surgical treatment of metastatic tumours to the pancreas: A single centre experience and review of literature.World J of Surg 2006;30:1536 – 42.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




