Solitary Basal Ganglia Tuberculous Abscess in an Immunocompetent Individual
Raja Shariff REF & Sapuan S
Cite this article as: BJMP 2019;12(3):a021
|
|
Abstract Background: Tuberculosis (TB) involving the central nervous system (CNS) account for 2 to 5% of all TB cases. Treatment should be guided by histological evidence, which unfortunately can be difficult to obtain in those with CNS dissemination. We present a rare case of solitary basal ganglia tuberculous abscess, with no evidence of pulmonary TB. Abbreviations: Anti-Tuberculous Therapy (ATT), Cerebrospinal Fluid (CSF), Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Central Nervous System (CNS), Mycobacterium Tuberculosis (MTB), Tuberculous Abscess (TBA), Ziehl-Neelsen (ZN), Nucleic Acid Amplification Test (NAAT) |
Background
Tuberculosis (TB) involving the central nervous system (CNS) account for 2 to 5% of all TB cases1. Commonly it manifests in three ways – meningo-encephalitis, tuberculomas or abscesses2. Treatment should be guided by histological evidence, which unfortunately can be difficult to obtained in those with CNS dissemination. We present a rare case of solitary basal ganglia tuberculous abscess, which provided a diagnostic dilemma and led to complex management planning.
Case Report
A 53-year old man, with no known medical illness, presented with a 5-day history of fever, vomiting and altered mental behaviour. His vital signs were stable, on arrival aside from being pyrexial at 38°C. There was, however, neck stiffness noted on clinical examination as well as evidence of increased tone on the right upper and lower limbs, with an upgoing right-sided plantar response. Power was preserved in all limbs.
An initial contrast-enhanced computed tomography (CT) imaging of the brain revealed a hypodense lesion measuring 1.6 cm x 2.1 cm x 1.8 cm in the left basal ganglia region, with rim enhancement, complicated by cerebral oedema causing mass effect and mild hydrocephalus (Figure 1). A lumbar puncture was performed, and cerebrospinal fluid (CSF) analysis suggested the possibility of bacterial infiltration (Table 1). Initial, Ziehl-Neelsen (ZN) staining, mycobacterium tuberculosis (MTB) cultures and Gene Xpert nucleic acid amplification test (NAAT) from CSF were negative and a HIV antibody serology was negative as well. A transthoracic echocardiogram and CT imaging of the thorax and neck were both performed, failing to identify a possible source of spread. Furthermore, there was no evidence of focal lung infection or collection, and no evidence of lymphadenopathy of note.
The patient was initially treated for 2 weeks with intravenous antibiotics, using intravenous Ceftriaxone 2g BD and Metronidazole 500mg TDS. Intravenous Dexamethasone was also commenced in view of the cerebral oedema. Unfortunately, the patient showed no clinical improvement, prompting repeat CT and Magnetic Resonance Imaging (MRI) which revealed an unchanged left basal ganglia enhancing lesion, with worsening obstructive hydrocephalus, perilesional oedema causing midline shift. The lesion was in contact with the lateral wall of the left lateral ventricle, with evidence of acute ventriculitis and involvement of the basal cisterns (Figure 2). A right-sided ventriculo-peritoneal shunt was inserted in view of the worsening hydrocephalus and persistent symptoms of headache and vomiting. Subsequently, stereotactic drainage and biopsy of the lesion was discussed but could not be performed in view of its deep location. A decision was thus made to initiate anti-tuberculosis therapy (ATT) empirically and to cease antibiotics. Subsequently, the patient’s clinical state improved with ongoing ATT and active inpatient rehabilitation, alongside improvement in the lesion, via radiological evidence (Figure 3).
Table 1: Cerebrospinal Fluid (CSF) test and other investigations performed during admission.
| Test for Cerebrospinal Fluid (CSF) | Results | Other Test | Results |
| Micro-Total Protein | 3.8 g/dL | Lumbar Puncture Opening Pressure | 19 cm H20 |
| Glucose | 1.65 mmol/L | Lumbar Puncture Closing Pressure | 16 cm H20 |
| Culture & Sensitivity | Negative | Random Capillary Glucose | 7.3 mmol/l |
| India Ink | Negative | ||
| Ziehl-Neelsen Stain | Negative | HIV Antibody | Negative |
| MTB Culture | Negative | Echocardiogram | No vegetation or mass |
| MTB NAAT (GeneXpert) | Negative | ||
| Cell Count & Cytology | No atypical cells. Mixed of pleomorphs and lymphocytes seen |
Figure 1: CT imaging of the brain on (a) axial and (b) saggital view, illustrating a well-circumscribed, rim-enhanced lesion in the left basal ganglia region, suspicious of an abscess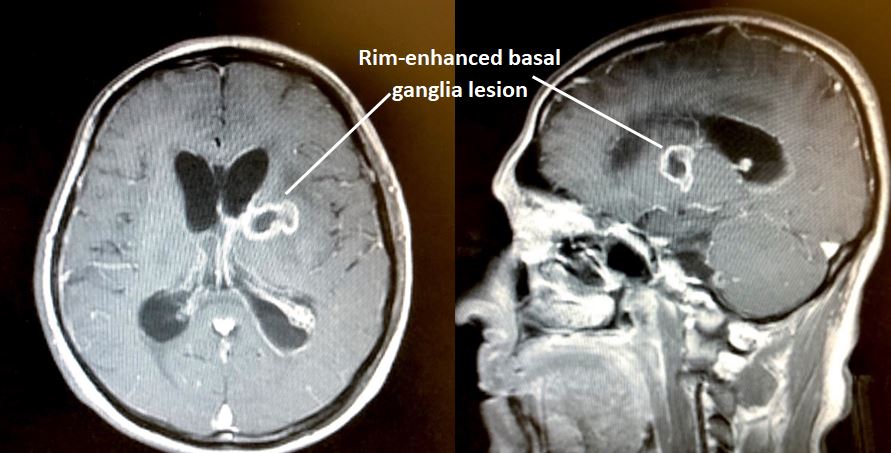
Figure 2: T2-sequence of MRI brain on axial view (a) pre- and (b) post-procedure involving ventriculo-peritoneal shunting, illustrating a well-circumscribed hyperdense basal ganglia lesion, with peri-lesional oedema, as well as evidence of hydrocephalus.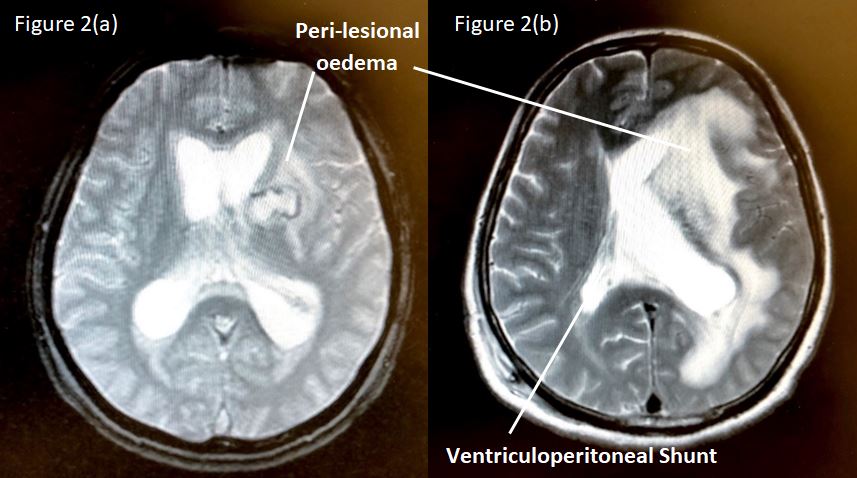
Figure 3: Non-contrasted CT brain on axial view, illustrating less apparent left basal ganglia lesion, with hypodensities in areas of previous oedema, as well as an in-situ ventriculo-peritoneal shunt.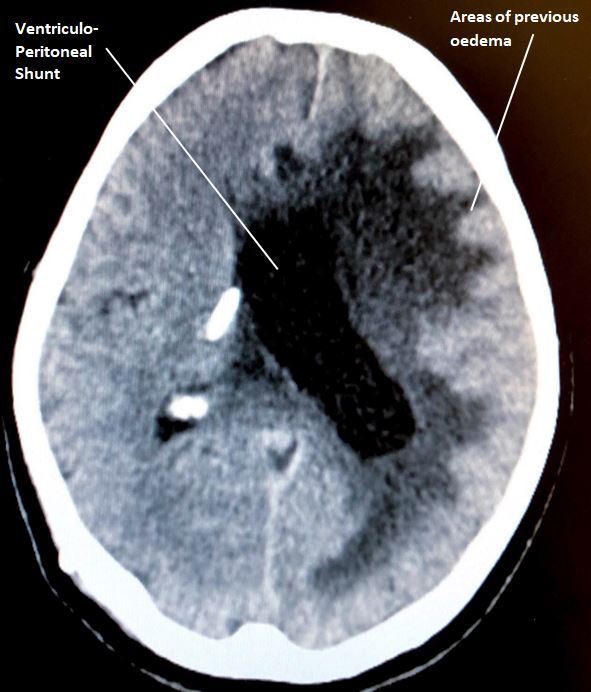
Discussion
Basal ganglia abscesses are very rare, incidence varying between 0.9 to 4% of total brain abscesses3. These are often disseminated lesions from sources such as congenital heart disease infections, intrathoracic and abdominal sepsis, dental caries, otitis media or sinusitis3-4. Solitary tuberculosis lesions, which includes tuberculous abscesses (TBA), in the basal ganglia are additionally more uncommon, even in endemic countries, as they normally have a predilection for the cerebellum and brainstem5. TBA has been seen in both the immunocompromised, or otherwise, where clinical presentation differs only slightly6-9.
Similar to other brain abscesses, stereotactic aspiration remains the gold standard diagnostic tool but there is a risk of rupture into ventricles or the subarachnoid space (leading to ependymitis or meningitis), worsening neurological deficits and more importantly the possible need for repeated procedures in as many as 70% of patients9.
Although experts advocate the combination of both surgical and chemotherapeutic therapy in managing TBA, the former was limited by the location of the lesion, whereas the latter was due to lack of histological evidence. Furthermore, the lack of risk factors, negative yield from cultures, NAAT and ZN stain, and inability to biopsy made the decision-making complex in our patient. Fortunately, there are evidence to support presumptive ATT for diagnostic and therapeutic purposes, which was adopted in our case5. This, however, requires cerebrospinal fluid examination, lung CT imaging and brain MRI that can provide circumferential evidence for diagnosis and to monitor treatment progress, all of which were performed in our gentleman5. In fact, CT imaging of the thorax is considered mandatory in cases suspicious of asymptomatic and subclinical extra-neurological tuberculosis, although yield remains poor (detecting abnormalities in only 38 to 56%)10.
Conclusion
Although CNS involvement in extra-pulmonary tuberculosis is not uncommon, TBA in the basal ganglia region remains a unique entity which poses a challenge in terms of diagnosis, as histological evidence is often difficult to obtain. As adopted in the case highlight, empirical therapy using ATT remains a valid option, especially in areas limited by resources and appropriate skills to perform intracranial biopsies, which is a common occurrence in endemic areas globally.
|
Acknowledgements The authors would like to acknowledge Universiti Teknologi MARA and the Clinical Research Centre (Hospital Sungai Buloh) for supporting the submission of the following case report. Competing Interests None declared Author Details RAJA SHARIFF REF (MRCP), Universiti Teknologi MARA (UITM) Sungai Buloh, Malaysia. SAPUAN S (MMED), Hospital Sungai Buloh, Malaysia. CORRESPONDENCE: RAJA SHARIFF REF, Universiti Teknologi Mara Sungai Buloh, Jalan Hospital, 47000, Sungai Buloh, Selangor, Malaysia. Email: rajaezman@gmail.com |
References
- Goldstein W, Maimon N & Avendan˜o M. Central nervous system tuberculous abscess. Eur J Intern Med 2007; 18(6): 504-506.
- Corti M, Palmero D & Trione N, et al. Cerebral abscess associated with multi drug resistant tuberculosis and immune reconstitution. Int J Tuberc Lung Dis 2006; 10(12): 1417.
- Bhatia R, Tandon P & Mishra AK. Inflammatory lesion of the basal ganglia and thalamus: Review of twenty-one cases. Neurosurgery 1986; 19: 983-988.
- Lutz TW, Landott H, Wasner M, et al. Diagnosis and management of abscess in the basal ganglia and thalamus: a survey. J Neurosurg 1984; 44: 226-232.
- Psimaras D, Bonnet C, Heinzmann A, Cardenas G, et al. Solitary tuberculous brain lesions: 24 new cases and a review of the literature. Revue neurologique 2014; 1-10.
- Farrar DJ, Flanigan TP, Gordon NM, Gold RL & Rich JD. Tuberculous brain abscess in a patient with HIV infection: case report and review. Am J Med 1997; 102(3): 297-301.
- Schoeman JF, Morkel A, Seifart HI, et al. Massive posterior fossa tuberculous abscess developing in a young child treated for military tuberculosis. Possible role of very rapid acetylation of isoniazid. Pediatr Neurosurg 1998; 29(2): 64-68.
- Whiteman M, Espinoza L, Post MJ, Bell MD & Falcone S. Central nervous system tuberculosis in HIV-infected patients: clinical and radiographic findings. Am J Neuroradiol 1995; 16(4): 1319-1327.
- Cardenas G, Soto-Hernandez JL, Orozco RV, et al. Tuberculous Brain Abscesses in Immunocompetent Patients: Management and Outcome. Neurosurgery 2010; 67: 1081–1087
- Yaramis A, Bukte Y, Katar S & Ozbek MN. Chest computerized tomography scan findings in 74 children with tuberculous meningitis in southeastern Turkey. Turk J Pediatr 2007; 49(4): 365–9

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




