Seroprotection after Hepatitis B Vaccination in Expanded Programme on Immunisation
Mohammad Afzal, Khaliq Naveed, Shabbir Hussain, Shaukat Mehmood Qureshi, Asifa Majeed, Zia Farooqi, Alizay Gohar and Abdul Wahab
Cite this article as: BJMP 2011;4(4):a445
|
|
Abstract Aim: As part of a global strategy, Pakistan included the Hepatitis B (HB) vaccine in the national Expanded Programme on Immunisation (EPI) in 2004. The aim of this study was to know the status of seroprotection amongst those receiving HB vaccination in the EPI in Pakistan. Introduction: Hepatitis B vaccination has produced very convincing results in reducing disease burden in the developed world. As per the World Health Organisation (WHO) recommendations, most countries have included HB vaccination in the national EPI schedules. Pakistan included the HB vaccination in the EPI in 2004. There are various factors affecting seroprotection after HB vaccination done in the EPI, for example dosing schedule, maintenance of the cold chain and missing the birth dose, etc. There are no published studies to date regarding seroprotection status and anti-HBs antibodies levels after receiving the HB vaccination in the EPI in Pakistan. Methods: This study was conducted at the paediatric departments of Military Hospital (MH) and Combined Military Hospital (CMH), Rawalpindi from 1st January 2010 to 31st December 2010. One hundred and ninety-four children ranging from 9 months to 2 years of age, who had received HB vaccination according to the EPI schedule, were included. Blood samples were taken and tested for anti–HBs antibody levels by enzyme-linked immunosorbent assay (ELISA) at the Department of Biochemistry of Army Medical College, Rawalpindi. Anti–HBs antibody titres >10 IU/L was taken as seroprotection level as per WHO and kit manufacturers’ standards. Results: Out of 194 children, 133 (68.6%) had anti–HBs titres > 10 IU/L (seroprotected) while 61 (31.4%) had anti–HBs titres <10 IU/L (non-protected). GMT achieved among seroprotected vaccine recipients was 85.81 IU/L. One hundred and twenty-nine were male children and of them 95 (73.6%) had a protective level and 34 (26.4%) were non- protected. Sixty-five were female children and out of them 38 (58.5%) had a protective level while 27 (41.5%) were non-protected. The difference was significant between males and females (p value= 0.032). One hundred and eighty-four children received the vaccine procured through the public sector, out of which 123 (68.5%) developed anti-HBs levels >10 IU/L (protected) and 61 (23.2%) had anti-HBs titres <10 IU/L (non-protected). However, 10 children received privately procured HB vaccines of whom all developed anti-HB titres >10 IU/L (protected). The difference was significant between the public sector procured and privately procured vaccine (p-value= 0.028). One hundred and thirty-two children received the HB vaccination at army vaccination centres (MH & CMH). Out of them 96 (72.7%) developed anti-HBs levels >10 IU/L (protected) and 36 (27.3%) had antibody titres <10 IU/L (non protected). Sixty-two children were vaccinated at civil health facilities and at home by vaccination teams. Out of them 38 (58.5%) developed anti-HBs levels >10 IU/L (protected) while 27 (41.5%) had antibody titres <10 IU/L (non protected). Conclusion: Seroprotection achieved after HB vaccination received in the EPI at 6, 10 and 14 weeks in combination vaccination form was 68.6%. This is low as compared to results reported internationally. Geometric mean titre (GMT) levels achieved in seroprotected vaccine recipients are also low (85.81 IU/L) when compared with international data. There is a need to look into relevant aspects of HB vaccination in the EPI to improve seroprotection in future. Keywords: Hepatitis B, Hepatitis B vaccine, seroprotection, EPI |
Introduction
Hepatitis B (HB) is a major disease and is a serious global public health problem. About 2 billion people (latest figures so far by WHO) are infected with the hepatitis B virus (HBV) all over the world. Interestingly, rates of new infection and acute disease are highest among adults, but chronic infection is more likely to occur in persons infected as infants or young children, which leads to cirrhosis and hepatocellular carcinoma in later life. More than 350 million persons are reported to have chronic infection globally at present1,2. These chronically infected people are at high risk of death from cirrhosis and liver cancer. This virus kills about 1 million persons each year. For a newborn infant whose mother is positive for both HB surface antigen (HBsAg) and HB e antigen (HBeAg), the risk of chronic HB Virus (HBV) infection is 70% - 90% by the age of 6 months in the absence of post-exposure immunoprophylaxis3.
HB vaccination is the only effective measure to prevent HBV infection and its consequences. Since its introduction in 1982, recommendations for HB vaccination have evolved into a comprehensive strategy to eliminate HBV transmission globally4. In the United States during 1990–2004, the overall incidence of reported acute HB declined by 75%, from 8.5 to 2.1 per 100,000 population. The most dramatic decline occurred in children and adolescents. Incidence among children aged <12 years and adolescents aged 12-19 years declined by 94% from 1.1 to 0.36 and 6.1 to 2.8 per 100,000 population, respectively2,5.
Population of countries with intermediate and high endemicity rates are at high risk of acquiring HB infection. Pakistan lies in an intermediate endemic region with a prevalence of 3-4% in the general population6. WHO has included the HB vaccine in the Expanded Programme on Immunisation (EPI) globally since 1997. Pakistan included the HB vaccination in the EPI in 2004. Primary vaccination consists of 3 intramuscular doses of the HB vaccine. Studies show seroprotection rates of 95% with standard immunisation schedule at 0, 1 and 6 months using a single antigen HB vaccine among infants and children7,8. Almost similar results have been reported with immunisation schedules giving HB injections (either single antigen or in combination vaccines) at 6, 10 and 14 weeks along with other vaccines in the EPI schedule. But various factors like age, gender, genetic and socioenvironmetal influences, are likely to affect seroprotection rates9.So there is need to know actual seroprotection rates in our population where different vaccines, EPI procured and privately procured incorporated in different schedules are used. This study has been conducted to know the real status of seroprotection against HB in our children. Results will help in future policy-making, highlighting our shortcomings, comparing our programme with international standards and moreover augment future confidence in vaccination programmes.
Materials And Methods
This study was conducted at vaccinations centres and paediatrics OPDs (Outpatient Departments) of CMH and MH, Rawalpindi, Pakistan. Children reporting for measles vaccination at vaccination centres at 9 months of age were included. Their vaccination cards were examined and ensured that they had received 3 doses of HB vaccine according to the EPI schedule, duly endorsed in their cards. They included mainly children of soldiers but some civilians also who were invited for EPI vaccination at the MH vaccination centre. Children of officers were similarly included from the CMH vaccination centre and vaccination record was ensured by examining their vaccination cards. Some civilians who received private HB vaccination were included from paediatric OPDs . Some children beyond 9 months and less than 2 years of age who reported for non-febrile minor illnesses in the paediatric OPD at CMH and MH, were also included and their vaccination status was confirmed by examining their vaccination cards.
Inclusion Criteria
1) Male and female children >9 months and <2 years of age.
2) Children who had received 3 doses of HBV according to the EPI schedule at 6,10 and 14 weeks.
3) Children who had a complete record of vaccination- duly endorsed in vaccination cards.
4) Childen who did not have history of any chronic illness.
Exclusion Criteria
1) Children who did not have proper vaccination records endorsed in their vaccination cards.
2) Interval between last dose of HBV and sampling was <1 month.
3) Children suffering from acute illness at time of sampling.
4) Children suffering from chronic illness or on immunosuppressive drugs.
Informed consent for blood sample collection was obtained from the parents or guardians. The study and the informed consent form was approved by the institutional ethical review board. Participants were informed about results of HBs antibody screening. After proper antiseptic measures, blood samples (3.5 ml) were obtained by venepuncture. Autodisabled syringes were used. Collected blood samples were taken in vaccutainers and labelled by identification number and name of child. Samples were immediately transported to the Biochemistery Department of Army Medical College. Samples were kept upright for half an hour and then centrifuged for 10 minutes. Supernatant serum was separated and stored at -20 0C in 1.5 ml eppendorf tubes till the test was performed. Samples were tested using ELISA (DiaSorin S.p.A Italy kit) for detection of anti-HBs antibodies according to manufacturers’ instructions. The diagnostic specificity of this kit is 98.21% (95% confidence interval 97.07-99.00%) and diagnostic sensitivity is 99.11% (95% confidence interval 98.18-99.64%) as claimed by the manufacturer. Anti-HBs antibody enumeration was done after all 3 doses of vaccination (at least 1 month after the last dose was received).
As per WHO standards, anti-HBs antibody titres of >10 IU/L is taken as protective and samples showing antibody titres <10 IU/L were considered as non-protected. Samples having antibody titres >10 IU/L were taken as seroprotected against HB infection. All relevant information was entered in a predesigned data sheet and used accordingly at the time of analysis. Items entered included age, gender, place of vaccination, type of vaccination (private or government procured), number of doses and entitlement status (dependent of military personnel or civilian). The study was conducted from 1st January 2010 to 31st Dec 2010.
Statistical Analysis
Data was analysed using SPSS version 15. Descriptive statistics were used to describe the data, i.e. mean and standard deviation (SD) for quantitative variables, while frequency and percentages were used for qualitative. Quantitative variables were compared through independent samples’ t-test and qualitative variables were compared through the chi-square test between both the groups. A P-value <0.05 was considered as significant.
The mean age of the children was 13.7 months. The overall frequency of children with titres <10 IU/L was 61 (31.4%) while frequency of children with titres >10 IU/L was 133 (68.6%).
Geometric mean titres (GMT) were 85.81 for the seroprotected (>10 IU/L) category.
Results
One hundred and ninety-four children, who had received HB vaccination according to EPI schedule, were tested for anti-HBs titres. Out of them 61 (31.4%) had anti-HBs titres less than 10 IU/L (non-protective level) while 133 (68.6%) had anti-HBs titres above 10 IU/L (protective level) as shown in Figure 1. The GMT of anti-HBs among the individuals having protective levels (> 10 IU/L) was found to be 85.81 IU/L.
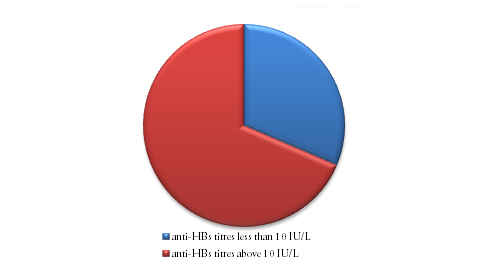
Figure 1
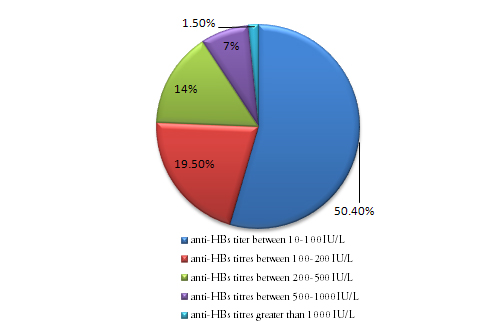
Figure 2
Figure 2 shows that anti-HBs titres between 10–100 IU/L was found in 75 (50.4%) children. Twenty-six (19.5%) individuals had titres between 100–200 IU/L. Twenty (14%) children had titres between 20–500 IU/L, 10 (7%) children had titres between 500–1000 IU/L and only 2 (1.5%) children had anti-HBs titres > 1000 IU/L.
One hundred and eighty-four children received vaccination supplied by government sources (Quinevaxem by Novartis) out of which 61 (33.1%) children had anti-HBs titres <10 IU/L (non- protective) and 123 (66.9%) had anti-HBs titres >10 IU/L (protective level). Only 10 children had received vaccination obtained from a private source (Infanrix Hexa by GSK), out of which all 10 (100%) had anti-HBs titres >10 IU/L (protective level). Comparison between the two groups revealed the difference to be significant (P value= 0.028).
One hundred and thirty-two children received vaccination from army health facilities (CMH and MH) out of which 36 (27.3%) had anti-HBs titres < 10 IU/L while 96 (72.7%) had anti-HBs titres >10 IU/L. Sixty-two children were vaccinated at civilian health facilities (health centres or vaccination teams visiting homes). Out of them 25 (40.3%) had anti-HBs titres <10 IU/L while 37 (59.7%) had anti- HBs titres >10 IU/L. The difference was insignificant (P value= 0.068). Gender analysis revealed that in the study group 129 (68.5%) were male children. Out of them 34 (26.4%) had anti-HBs titres <10 IU/L and 95 (73.6%) had anti-HBs titres >10 IU/L. Sixty-five (31.5%) were female children and out of them 27 (41.5%) had anti-HBs titres <10 IU/L while 38 (58.5%) had anti-HBs titres > 10 IU/L. Statistical analysis revealed the difference between males and females was significant (P value= 0.032).
One hundred and twenty-two (62.9%) children were less than 1 year of age. Out of them 37 (30.3%) had anti-HBs titres <10 IU/L and 85 (69.7%) had anti- HBs titres >10 IU/L. Seventy-two (37.1%) children ranged between 1 to 2 years of age. Out of them 24 (33.3%) had anti-HBs titres <10 IU/L while 48 (66.7%) had anti-HBs titres >10 IU/L. On comparison the difference between the two groups was insignificant (P value= 0.663), as shown in Table 1.
| Patient characteristics | Anti-HBs titres (< 10 IU/L) (n = 61) | Anti-HBs titres (> 10 IU/L) (n = 133) | P – values |
| Age groups | 0.63 NS | ||
| < 1year (n = 122) | 37 (30.0%) | 85 (69.7%) | |
| > 1year (n = 72) | 24 (33.3%) | 48 (66.7%) | |
| Gender | 0.032 | ||
| Male (n = 129) | 34 (26.4%) | 95 (73.6%) | |
| Female (n = 65) | 27 (41.5%) | 38 (58.5%) | |
| Hospital | 0.068 NS | ||
| Army (n = 132) | 36 (27.3%) | 96 (72.7%) | |
| Civilian (n = 62) | 25 (40.3%) | 37 (59.7%) | |
| Vaccine Type | 0.028 | ||
| Government (n = 184) | 61 (33.2%) | 123 (66.8%) | |
| Private ( n = 10) | 0 (0%) | 10 (100%) | |
Table 1 (NS = Insignificant; * = Significant )
Discussion
HB is a global health problem with variable prevalence in different parts of the world1. Various studies carried out in different parts of Pakistan in different groups of population have shown diverse figures regarding prevalence of HB. However, a figure of 3-4% is accepted as general consensus by and large, thus making Pakistan an area of intermediate endemicity for HB6. Yet when we extrapolate these figures to our population, it is estimated that Pakistan hosts about seven million carriers of HB which is about 5% of the worldwide 350 million carriers of HB10,11.
Age at the time of infection plays the most important role in acquisition of acute or chronic HBV disease. HBV infection acquired in infancy is responsible for a very high risk of chronic liver disease due to HBV in later life12. HB is a preventable disease and fortunately vaccination at birth and during infancy can eradicate the disease globally, if vaccination strategy is effectively implemented13. This can be claimed as the first anti-cancer vaccine which prevents hepatocellular carcinoma in later life.
In Pakistan, the HB vaccine was included in the EPI in 2004, given along with DPT (Diphtheria, Pertussis, Tetanus) at 6, 10 and 14 weeks of age. The vaccine is provided through government health infrastructure to health facilities. Private HB vaccines supplied as a single antigen or in combination vaccines are also available in the market. The efficacy of these recombinant vaccines is claimed to be more than 95% among children and 90% among normal healthy adults14. The immunity of the HB vaccination is directly measured by development of anti-HBs antibodies more than 10 IU/L, which is considered as a protective level15. However, it is estimated that 5–15 % of vaccine recipients may not develop this protective level and remain non-responders due to undermentioned reasons.16 Published studies regarding antibody development in relation to various factors in terms of immunogenicity and seroprotection, show highly varied results. Multiple factors like dose, dosing schedules, sex, storage, site and route of administration, obesity, genetic factors, diabetes mellitus and immunosupression, affect HB antibodies development response17.
Although the HB vaccine was included in the EPI in 2004 in Pakistan, until now no published data showing seroconversion and seroprotection among vaccine recipients of this programme is available on a national level to our knowledge. Our study has revealed that out of 194 children, only 133 (68.6%) had anti-HBs titres in the protective range (>10 IU/L) while 61 (31.4%) did not develop seroprotection. These results are low as compared to other international studies. A study from Bangladesh among EPI vaccinated children shows a seroprotection rate of 92.2%13 while studies from Brazil18 and South Africa19 have separately reported seroprotection rates of 90.0% and 86.6%, respectively. Studies from Pakistan carried out in adults also show seroprotection rates (anti-HBe titres >10 IU/L) of more than 95% in Karachi University students14 and 86% in health care workers of Agha Khan University Hospital20, respectively. However, in these studies the dosing schedule was 0, 1 and 6 months, and participants were adults. These results are consistent with international reports.
The gravity of low seroprotection after HB vaccination is further aggravated when we extrapolate these figures to our overall low vaccination coverage rates of 37.6% to 45% as shown in studies at Peshawar and Karachi respectively21,22. One can imagine a significantly high percentage of individuals vulnerable to HBV infection even after receiving HB vaccine in an extensive national EPI programme. Therefore, a large population still remains exposed to risk of HBV infection, and national and global eradication of HBV infection will remain a dream. Failure of seroprotection after receiving the HBV vaccination in the EPI will also be responsible for projecting a sense of false protection among vaccine recipients.
Dosing schedule is an important factor in the development of an antibody response and titre levels. According to the Advisory Committee on Immunization Practices (ACIP) of America, there should be a minimum gap of 8 weeks between the second and third doses and at least 16 weeks between the first and third doses of the HB vaccination23. To minimize frequent visits and improve compliance, the dosing schedule has been negotiated in the EPI to 6, 10 and 14 weeks24. Although some studies have shown this schedule to be effective, the GMT of anti-HBs antibodies achieved was lower than that achieved by the standard WHO schedule25. This may be one explanation of lower rates of seroprotection in our study. The GMT achieved in our study among the children having protective levels of antibodies is 85.81 IU/L which is lower than most other studies. This supports the observation that GMT achieved in this schedule is lower than that produced by the standard WHO schedule. This may result in breakthrough infection of HB in vaccinated individuals in later life due to waning immunity. However, the immune memory hypothesis supports protection of vaccinated individuals in later life in spite of low anti-HBs antibody titres26. Yet further studies are required to dispel this risk.
Another shortcoming of this schedule is to miss the dose at birth (‘0 dose’). It has been reported that the 0 dose of the HB vaccine alone is 70% - 95% effective as post-exposure prophylaxis in preventing perinatal HBV transmission without giving HB immunoglobulins27. This may also be a factor contributing to lower rates of seroprotection in our study as we have not done HBsAg and other relevant tests to rule out HBV infection in these children. Moreover pregnant ladies by and large are not screened for HBV infection in Pakistan routinely in the public sector except in a few big cities like Islamabad, Lahore or Krachi. Therefore, we do not know the HB status of pregnant mothers and the risk of transmission to babies remains high. Different studies have reported much varied figures of HB status in pregnant ladies. A study from Karachi reports 1.57% pregnant ladies are positive for HBsAg while a study from Rahim Yar Khan reports this figure to be up to 20%28,29. A study by Waheed et al regarding the transmission of HBV infection from mother to infants reports the risk to be up to 90%30. All of these studies support the importance of the birth dose of the HB vaccination and augment the fact that control and eradication of HB with the present EPI schedule is not possible. Jain from India has reported a study using an alternative schedule of 0, 6 weeks and 9 months. He has reported it to be comparable to the standard WHO schedule of 0, 1, 6 months in regards to seroprotection and GMT levels achieved31. This schedule can be synchronised with the EPI schedule, avoiding extra visits and incorporating the birth dose. A similar schedule can also be incorporated in our national EPI.
In our study, seroprotection rates were found to be low in the female gender and the difference was significant. This finding differs with other studies which report lower seroprotection rates in males32. Although the number of female children was less, there is no plausible explanation for this observation. The site of inoculation of the HB vaccine is also very important for an adequate immune response. Vaccines given in the buttocks or intradermally produce lower antibody titres than intramuscular injections given in the outer aspect of the thigh in children, due to poor distribution and absorption of the vaccine within the host body. The practice of giving vaccinations in the buttocks by vaccinators is a common observation which they feel convenient for intramuscular injection in children. This may also be one reason for low seroprotection rates in our study, as we picked the children at random who had received vaccination at public health facilities except a small number of private cases.
The effectiveness of the vaccine also depends on the source of procurement and proper maintenance of the cold chain. In this study 100% seroprotection was observed in children who received the HB vaccine procured from a private source. Although the number of private cases was less, this factor of source and the cold chain also needs attention. To address this issue proper training of EPI teams regarding maintenance of temperature, injection techniques, motivation and monitoring can improve outcomes substantially.
The findings of this study are different from published literature because this is a cross-sectional observational study. This reports the actual seroprotection rates after receiving the HB vaccination in the EPI schedule. While most other studies show the results after ensuring control of influencing factors such as type of vaccine, dose, schedule, route of administration, training and monitoring of local EPI teams and health status of vaccine recipients, etc. Therefore, this is an effort to look at a practical scenario and evaluate outcomes which can help in framing future guidelines to achieve the goal of control and eradication of HB infection. Further studies are required at a large scale to determine the effect of HB vaccination at a national level.
Conclusion
The HB vaccination programme has decreased the global burden of HBV infection, but evidence of decreased burden is not uniform amongst world population.Of course figures witness marked decrease in developed world while in developing world statistics show little change. Unfortunately, implementation of this programme is not uniformly effective in all countries, thus resvoirs of infection and the source of continued HBV transmission persists. HBV infection is moderately endemic in Pakistan. The HB vaccine has been included in the national EPI since 2004. The present study shows seroprotection rates of only 68.6% in vaccine recipients, which is low when compared with other studies; 31.4% of vaccine recipients remain unprotected even after vaccination. Moreover GMT achieved in seroprotected vaccine recipients is also low (85.81 IU/L). There can be multiple reasons for these results, such as type of vaccine used, maintenance of the cold chain, route and site of administration, training and monitoring of EPI teams and dosing schedule. In present practice, the very important birth dose is also missing. These observations warrant review of the situation and appropriate measures to be taken to rectify the above mentioned factors, so that desired seroprotection rates after HB vaccination in the EPI can be achieved among vaccine recipients.
|
Acknowledgements We are thankful to the administration team of National University of Sciences and Technology (NUST), Islamabad, Pakistan for financing this study project. We are also thankful to the Department of Biochemistry and Molecular Biology, Army Medical College, for conducting laboratory tests. Mr. Ghulam Husnain of Army Medical College deserves special thanks for typing the manuscript. Special thanks also to Miss Irum, statistician of Army Medical College, for carrying our statistical analysis. Author Details MOHAMMAD AFZAL, Associate Professor of Paediatrics, Army Medical College, Rawalpindi. KHALIQ NAVEED, Head of Dept of Biochemistry, Army Medical College Rawalpindi. SHABBIR HUSSAIN, Assistant Professor of Paediatrics, Armed Forces Postgraduate Medical Institute, Rawalpindi. SHAUKAT MEHMOOD QURESHI, Associate Professor of Community Medicine, Army Medical College, Rawalpindi. ASIFA MAJEED, Assistant Prof Biochemistry, Army Medical College, Rawalpindi. ZIA FAROOQI, Research Technologist, Dept of Biochemistry and Molecular Biology, Army Medical College, Rawalpindi. ALIZAY GOHAR, 4th year MBBS student, Foundation University Medical College, Rawalpindi. ABDUL WAHAB, 3rd year MBBS student, Army Medical College, Rawalpindi. CORRESPONDENCE: Dr.Mohammad Afzal, Associate Professor of Paediatrics, Army Medical College, Rawalpindi. Email: afzalchpak@yahoo.com |
References
1.World Health Organization. HB vaccines: Weekly Epidemiol Rec 2009;40:405-420. 2. A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus Infection in the United States. MMWR 2005;54/No.RR-16:1-32.3.Okada K, Kamiyama I, Inomata M, Imai M, Miyakawa Y. e antigen and anti-e in the serum of asymptomatic carrier mothers as indicators of positive and negative transmission of HB virus to their infants. N Engl J Med 1976;294:746-9.4.CDC. Recommendation of the Advisory Committee on Immunization Practices (ACIP): Inactivated HB virus vaccine. MMWR 1982;31:317-7, 327-8.5.CDC. National, State and urban area vaccination coverage among children aged 19-35 months United States, 2004. MMWR2004:54:717-21.6.Abbas Z, Jafri W, Shah SHA, Khokar N, Zuberi SJ. Members of the consensus panel. PSG consensus statement on management of HB virus infection – 2003. J Pak Med Assoc 2004, 54:150-8.7.Kane M. Global Program for control of hepatitis B infection. Vaccine 1995;13:S47-498.World Health Organization. Immunization Policy WHO/EPI/GEN/95.3.1995.9.Gomber Sunil, Sharma Rajesh, Ramachandran VG Talwar Vibha, Singh Bharat. Immunogenicity of HB Vaccine incorporatd into the Expanded Programme of immunization schedule. Indian Paediatr 2000;37:411-413.10.Waseem J, Nadeem J, Yakoob K, Mohammad I, Tirmizi SFA, et al. HB & C: prevalence and risk factors associated with seropositivity among children in Karachi, Pakistan. BMC Infectious disease. 2006;6:101.11.Zaman AS. 2003.Daily Dawn internet addition. 23rd January.12.Stevens CE, Toy PT, Tong MJ, et al. Perinatal HB virus transmission in the United States: prevention by passive – active immunization JAMA 1985;253:1740-5.13.Guho A, Ahaad A, Salam A, Aleem A, Haq AE, Islam QE. Seroconversion after recombinant HB vaccination. J MEDICINE 2010;11:143-150.14.Hakeem ST, Nadeem SG, Kazmi SU. Comparative evaluation of four HB vaccines in Pakistan. Reactogenicity & Immunogenicity. BJMP 2009;2:30-34.15.Jacj ADM, Hall AJ, Maine M, Whittle HC. What level of hepatitis B antibody is protective? J infect Dis 1999;179:489-92.16.John TJ. HB immunization. Indian Pediatr 1995;32:609-613.17.Shaw FE, Jr, Guess HA, Roets JK et al. Effect of anatomic injection site, age and smoking on the immune response to HB vaccination. Vaccine 1989;7:425-30.18.Ribero TM and Azevedo RS. Seroconversion of HB vaccine in infants related to the mothers serostatus in a community of Sao Jose dos Campos, state of Sao Paulo, Brazil. Clinics 2006;61:519.Tsebes KV, Burnett RJ, Hlungwani NP, et al. The first five years of universal HB vaccination in South Africa; evidence for elimination of HBsAg carriage in under-5-year-children. Vaccine 2001;19:3919-392620. Zeeshan M, Jabeen K, Ali ANA, Ali AW, Farooqi SZ, Mehraj V, Zafar A. Evaluation of immune response to HB vaccine in health care workers at a tertiary care hospital in Pakistan: an observational prospective study. BMC Infectious Diseases 2007,7:120.21.Rehman H, Arshad S. Immunization status of children admitted in Pediatrics department Lady Reading Hospital Peshawar. Med Channel Jan- Mar 2007;13:36-8.22.Siddiqui N, Khan A, Nisar N, Siddiqui AA. Assessment of EPI(Expanded Program on Immunization) vaccine coverage in a peri-urban area. J Pak Med Assoc 2007;57:391-5.23.CDC. General recommendations of immunization: recommendations of the Advisory Committee on immunization Practices (ACIP) and the American Academy of the Family Physicians (AAFP). MMWR 2002;51;No RR-2):1-3524.Expanded Programme on Immunization: Framework for evaluating a vaccine for the EPI, WHO Documet WHO/EPI/GEN/93.5;1993g.25.Mittal SK, Rao S, Agarwal V, Parkash C, Thirupuram S. Simultaneous administration of HB vaccine with other EPI vaccines. Indian J Pediatr 1994;61:183-8.26.Resti M, Azzari C,Mannelli F, Rossi ME, Lioneti P, Vierucci A, Ten-year follow up study of neonatal HB immunization: are booster injections indicatd? Vaccine 197; 15:1338-40.27.Pichichero ME, Blater MM, Reisinger KS, et al. Impact of a birth dose of HB vaccine on the reactogenicity and immunogenicity of diphtheria-tetanus-acellular pertussis –HB-inactivated poliovirus-Haemophilus influenzae type b combination vaccination. Pediatr Infect Dis J 2002;21:854-9.28.Ali S, Memon A. Prevalence of HB infection in pregnant women in tertiary care hospital. Infect dis J 2007;16:36-8. 29.Hakeem A, KS, Abdullah M, RA, Hashmi I. Prevalence of HB surface antigen and anti HCV in pregnant ladies attending antenatal clinic at Sheikh Zayed Medical Complex Rahim Yar Khan. Esculapio J Services Inst Med Sci 2006;2:6-830.Kazmi K, Ghafoor A, Qureshi AW. Mother infant transmission of HB in Pakistan. Pak J Med Res 2003;42:152-6.31.Jain KA, Mittal SK, Ramji S and Chakravarti A. HB vaccine in the EPI Schedule. Indian J Pediatr 2004; 72(8):661-664.32.Zuckerman JN, Sabin C, Craig FM, et al. Immune response to a new hepatitis B vaccine in healthcare workers who had not responded to standard vaccine : randomized blind dose-response study. Br Med J 1997;314: 329-33.33.CDC. Suboptimal response to HB vaccine given by injection into the buttock. MMWR 1985;34:105-9,113.34.Craven DE, Awedh ZL, Kunches LM,Yunis EJ, Diestag JL, Werner BJ, Polk BF, snydman DR, Platt R, Crumpacker CS, Grady GF, Alper CA, Non responsiveness to HB vaccine in healthcare workers. Ann Inter Med 1986; 105:356-360.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




