Sedation by Surgeons: Is patient safety being compromised by non-anaesthetists?
Priyan R Landham, Umer Butt, Aabid Sanaullah, Hester C Taekema and Ahmed Shawky Eid
Cite this article as: BJMP 2011;4(2):a421
|
|
Abstract Introduction: Sedation is frequently administered by non-anaesthetic doctors in the emergency department whilst minor procedures are carried out. Guidelines and protocols exist but are non-anaesthetic doctors familiar with them? |
Introduction
Sedation is frequently administered outside of the operating theatre by non-anaesthetic doctors to facilitate minor procedures. This can be in both primary care including dental surgeries as well as in hospital departments such as radiology, endoscopy and the emergency department. Clinical practice including medication and monitoring equipment available and the personnel involved, varies not only between hospitals and regions but also between departments.
In the emergency department sedation is often performed in a busy clinical setting by junior doctors. This enables minor procedures to be carried out with subsequent discharge home reducing admission rates and the requirement for general anaesthesia. Other advantages include less workload pressure on the anaesthetic team and a significant improvement in the patient experience. Sedation is not without risk and significant morbidity and mortality is still associated with its use, particularly in the elderly and in combination with other medication1,2. Guidelines and protocols do exist to ensure safe practice but often it is only anaesthetic doctors who are aware of them3-7. A recent study by Fanning highlighted discrepancies in practice, skills and knowledge of doctors of various specialities and grades who administered sedation8. Anecdotal reports from orthopaedic colleagues suggested the variability in competence of doctors with clear implications for patient safety. We therefore sought to ascertain the current clinical practice, knowledge and prior training in sedation techniques of specialist registrars in orthopaedic and trauma surgery in our region.
Materials and Methods
A questionnaire based survey of 53 specialist registrars in orthopaedic and trauma surgery in the neighbouring Severn and South Wales regions was carried out. The questionnaire was modified from that developed by Fanning8 and circulated for completion at regional teaching sessions in Swansea and Bristol (Appendix 1). Each respondent had 15 minutes to complete the questionnaire based on their own experience, practice and knowledge. Respondents were not allowed to confer and full confidentiality was assured. The questionnaire was split into several sections that ascertained the respondents’ clinical practice including the procedures that sedation was used for, prior training, awareness of protocols and safety issues. Knowledge of the basic pharmacology of commonly used sedative agents was also tested. The final section asked respondents whether they had ever encountered any adverse events, the nature of the adverse event and whether assistance was required from the anaesthetic department.
Results
Orthopaedic specialist registrars (post basic surgical training) who were in higher surgical training completed 53 questionnaires. Sedation was performed in the emergency department by all respondents for manipulating fractures, reducing dislocated joints and for applying traction. Twenty-four respondents (45%) had read the sedation protocol for their hospital/emergency department. Thirteen respondents (25%) completed pre-sedation assessment forms, whilst only eleven (21%) completed the during-procedure monitoring data forms and twelve (23%) filled the after-procedure forms (Figure 1). Twenty-eight (53%) respondents ensured that either they or an assistant provided the patient with discharge advice.

Figure 1The percentage of respondents who had read the departmental protocol, completed monitoring forms and given advice prior to discharge.
Table 1: Sedative agents used.
|
Medication/Sedative Agent |
No of Respondents |
|
Diazepam |
31 |
|
Pethidine |
1 |
|
Midazolam |
35 |
|
Propofol |
15 |
|
Fentanyl |
3 |
|
Morphine |
44 |
|
Opiates with BDZs |
12 |
|
Local anaesthesia with sedation |
17 |
Almost all (98%) respondents administered sedation in the presence of an assistant. Forty-seven (89%) checked their medication with another healthcare professional. All fifty-three respondents supplied patients with concurrent oxygen whilst fifty-two ensured that resuscitation equipment was available nearby. In terms of specific training, forty-seven (89%) registrars had undergone Advanced Life Support training (ALS) but this qualification was only valid (within three years) for thirty-six (68%). Sixteen registrars (30%) stated they had undergone formal training or teaching regarding sedation (Figure 2). With regards to monitoring of patients, thirty-six (68%) respondents used pulse oximetry, fourteen (26%) used electrocardiogram (ECG) monitoring and twenty-eight (53%) measured blood pressure.

Figure 2The proportion of respondents who had received training in administering sedation
Morphine and other opioids were the most commonly used sedative medication (44 responses), followed by midazolam (35 responses), diazepam (31 responses) and propofol (15 responses). Twelve respondents combined opiates and benzodiazepines, whilst seventeen combined local anaesthesia with sedation (Table 1). Two-thirds of respondents (35 out of 53, 66%) administered sedation in boluses rather than calculating the correct dose per kilogram. The pharmacology questions devised by Fanning8 tested knowledge of metabolic pathways, duration of action and side effects. Overall, each question was answered correctly by over 50% of respondents (Figure 3). The mean score was 4.29 out of 7.
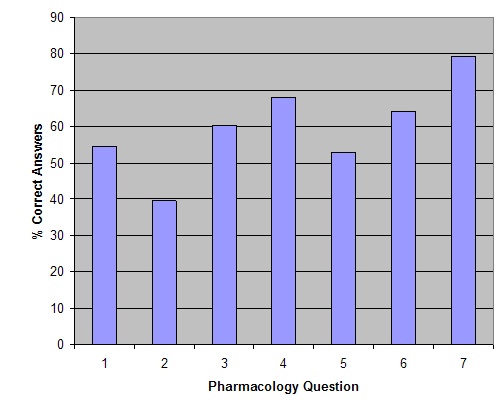
Figure 3The percentage of correct answers for each of the seven pharmacology questions.
Eighty percent of surveyed orthopaedic doctors (43 respondents) reported an adverse event after administering sedation. Twenty-nine respondents had at some stage contacted the anaesthetic department for assistance in managing a patient following sedation (Table 2).
Table 2: Adverse Events reported.
|
Adverse Effects |
No of Respondents |
|
Hypoxia |
20 |
|
Respiratory Depression |
13 |
|
Loss of consciousness |
7 |
|
Hypotension |
14 |
|
Prolonged Sedation |
13 |
|
Nausea and Vomiting |
14 |
Discussion
Non-anaesthetic doctors are permitted and often required to administer sedation to perform procedures in settings outside of the operating theatre. There are various published guidelines that detail the level of care and monitoring that should be provided when sedation is given3-7. It has been recommended that the same standards of monitoring apply to procedures under sedation or local anaesthesia as to procedures under general anaesthesia, and are irrespective of the location of the procedure3.
The report by an intercollegiate working party led by the Royal College of Anaesthetists summarised the key aspects of administering sedation based on existing guidelines6. Patients should be first assessed before the procedure by attendant staff, risk factors noted and further examination or investigations performed as necessary. Drug administration technique should be “one defined by a relevant specialty organisation”6 and doses adjusted to individual patient requirements. Combinations of drugs should be “employed with particular caution” especially sedatives and opioids. The opioids should be administered first and given time to be maximally effective before any sedative is given. The patient should be monitored during the procedure by a suitably trained individual recording pulse oximetry, blood pressure and electrocardiography. High flow oxygen should also be available. Doctors administering sedation should be able to control an airway using basic manoeuvres or airway adjuncts.
There is significant morbidity and mortality associated with sedation1,2. It is difficult to know the true incidence of cardio-respiratory complications after sedation, as this is often related to the procedure and patient factors. An audit of 14,000 endoscopic procedures reported a 30-day mortality of 1 in 20009 and there are several anecdotal reports of death following sedation10,11.
It is apparent that not all doctors are aware of or follow sedation guidelines. In the study by Fanning8, 42% of respondents completed a pre-procedure assessment form and 70% completed monitoring data sheets. In this study, whilst 45% of respondents had read departmental protocols, only 25% completed a dedicated pre-assessment of the patient and an equally low number recorded monitoring data forms during (21%) and after the procedure (25%). These low numbers are of potential concern. Time and resource constraints may play a part, particularly in a busy emergency department. Also, as junior doctors frequently rotate between hospitals, they may not be aware of departmental policies in each unit. It is understandably impractical to perform a procedure and concurrently complete a data monitoring form. This role should be delegated to an assistant.
Knowledge of basic pharmacology amongst respondents seemed reasonable and indeed better scores were achieved than in Fanning’s original paper. It would appear that a large number of respondents (n=29) have contacted anaesthetic colleagues for help following adverse events. This may simply reflect an acknowledgement of limited anaesthetic capabilities amongst respondents and a pre-emptive call for assistance rather than an anaesthetic “bail out” after cardio-respiratory compromise.
Whilst the questionnaire used is neither a formal assessment tool of clinical competence nor an accurate log of experience, it serves to highlight the potential limitations of current training. A clear issue is the low number of respondents who claim to have received formal teaching or training with regards to sedation. This may be due to the fact that little or no postgraduate training is provided in hospital specialities that require sedation. This is an area that needs to be addressed. The issues raised by this study are not new. In fact, a similar survey by Hewitt and Hartley in 1994 had similar findings and suggested that “sedation techniques should be included in induction teaching for A&E and orthopaedic juniors” and that all doctors administering sedation should have the “opportunity of resuscitation refresher courses”12.
Conclusion
Sedation is widely administered by non-anaesthetic doctors including orthopaedic surgeons in order to perform basic procedures outside of the operating theatres, mainly in the Accident and Emergency department. Whilst this study only involves 53 doctors in one speciality across two regions, it does give an insight into the self-reported clinical practice, knowledge and experience of a group of surgical doctors who are often required to administer sedation. Significantly, the majority of doctors surveyed reported they had not received any formal training. It is also apparent that departmental guidelines are not always known or followed. Due to the inherent risks of sedation, it is important that doctors are aware of and follow available guidelines. It is crucial that adequate training should be given to non-anaesthetic doctors to ensure they have the knowledge and skills to safely administer sedation. Otherwise a medical doctor, perhaps a registrar level from the Accident and Emergency department, should be present for patient assessment and management of airway compromise or any arising complication.
|
Competing Interests None declared Author Details PRIYAN R LANDHAM MBBS, MRCS Registrar Trauma & Orthopaedics, Royal United Hospital, Bath, UK UMER BUTT MBBS, MRCS Registrar Trauma & Orthopaedics, Yeovil General Hospital, Yeovil, UK AABID SANAULLAH MBBS, MRCS Registrar Trauma & Orthopaedics, Frenchay Hospital, Bristol, UK HESTER C TAEKEMA MBBS Registrar Anaesthesiaedics, Royal United Hospital, Bath, UK AHMED SHAWKY EID MBBCH, MRCS Trust fellow Trauma & Orthopaedics, Yeovil General Hospital, Yeovil, UK CORRESPONDENCE: PRIYAN R LANDHAM MBBS, MRCS Registrar Trauma & Orthopaedics, Royal United Hospital, Bath, UK Email: priyanlandham@doctors.org.uk |
References
1. Cravero JP, Blike GT, Beach M, Gallagher SM, Hertzog JH, Havidich JE, Gelman B. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the Pediatric Sedation Research Consortium. Pediatrics2006 Sep;118(3):1087-96.
2. Cote CJ, Notterman DA, Karl HW, Weinburg JA, McCloskey C. Adverse sedation events in pediatrics: a critical incident analysis of contributing factors. Pediatrics 2000;105:805-14.
3. Association of Anaesthetists of Great Britain and Ireland. Recommendations for Standards of Monitoring during Anaesthesia and Recovery. Guidelines of the Association of Anaesthetists of Great Britain and Ireland, December. London:AAGBI, 2000.
4. Pitetti RD, Singh S, Pierce MC. Safe and efficacious use of procedural sedation and analgesia by non-anaesthesiologists in a pediatric emergency department. Archives of Pediatric and Adolescent Medicine 2003;157:1090-6.
5. Holzman RS, Cullen DJ, Eichhorn JH, Philip JH. Guidelines for sedation by non-anaesthesiologists during diagnositic and therapeutic procedures. The Risk Management committee of the Department of Anesthesia of Harvard Medical School. Journal of Clinical Anestheisa 1994;6:265-76.
6. http://www.rcoa.ac.uk/docs/safesedationpractice.pdf [accessed December 2009]
7. Commission on the Provision of Surgical Services. The Royal College of Surgeons of England. Guidelines for Sedation by Non-anaesthetists. 1993
8. Fanning RM. Monitoring during sedation given by non-anaesthetic doctors. Anaesthesia, 2008; 63: 370-374.
9. Quine MA, Bell GD, McCloy RF, Charlton JE, Devlin HB, Hopkins A. A prospective audit of upper gastrointestinal endoscopy in two regions of England : safety, staffing and sedation methods. Gut 1995;36:462-7. (12 from working party)
10. Kovac C. Airline passenger dies after being sedated by doctor. BMJ 1999;318:12.
11. http://www.topix.com/forum/county/cook-il/THDSMC6MO19B32TMC [accessed December 2009]
12. Hewitt SM, Hartley RH. Manipulation under sedation in the accident and emergency department. Journal of Accident and Emergency Medicine 1994;11(3):186-8.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




