A Rapid Need Assessment Survey of Anaesthesia and Surgical Services in District Public Hospitals in Cross River State, Nigeria
Queeneth N. Kalu, Atim I. Eshiet, Essien I. Ukpabio, Anietimfon U. Etiuma and Emmanuel Monjok.
Cite this article as: BJMP 2014;7(4):a733
|
|
Abstract Background: The district hospitals in Cross River State of Nigeria serve majority of the population residing in the rural areas and little is known about their capacity to provide anaesthetic and surgical care. The present study is an initial needs assessment of anaesthesia and surgical services in public hospitals in Cross River State as a stepping stone for strengthening anaesthesia and surgical services. |
INTRODUCTION
Surgery and anaesthesia have traditionally been viewed as expensive, resource-intensive and requiring highly specialized training.1 This misconception has led to surgery and anaesthesia taking a back seat to public health, maternal and child health, and infectious diseases in global health.2 Surgery has also been termed the “neglected stepchild of global health.3These concepts have changed rapidly since it has been found that surgical diseases contribute about 11% to Disability Adjusted Life Years4 and therefore would benefit from preventive and public health strategies necessary to achieve the Millennium Development Goals. The realization of the huge public health burden of surgical diseases in low and medium income countries (LMICs), and the fact that surgical services and treatment could be made cost effective, led World Health Organization (WHO) to launch the Global Initiative for Emergency and Essential Surgical Care (GIEESC) in 2005.5
The GIEESC is a global forum whose goal is to promote collaboration among diverse groups of stakeholders to strengthen the delivery of surgical services at the primary referral level in LMICs.5 Improvements in surgical services at the primary referral level in LMICs will equally require the provision of safe and effective anaesthesia. The provision of safe and effective anaesthesia will need adequately trained human resources and essential health technologies. The surgical and anaesthesia service capacity have generally been very low in sub-Saharan Africa (SSA) as evidenced through surveys conducted in Ethiopia,6 Gambia,7,8 Ghana,9,10 Liberia,8,11 Malawi,12 Nigeria,13 Sierra Leone,8,14 Rwanda,15,16 Tanzania,8,17 and Uganda.18 The survey from Nigeria was conducted among rural private hospitals and was administered to attending members in a conference of the Association of Rural Surgical Practitioners of Nigeria.13 This was done using the Personnel, Procedures, Equipment and Supplies (PIPES) survey tool developed by the non-governmental organization Surgeons Overseas (SOS).13 This is a tool developed to assess surgical capacity through the workforce, infrastructure, skill, equipment, and supplies of health facilities in LMICs.13 The other indicated surveys done in SSA used a comprehensive survey tool designed by the Harvard Humanitarian Initiative. This tool was adapted from the WHO Tool for Situational Analysis to Assess Emergency and Essential Surgical Care as part of an international initiative to assess surgical and anaesthesia capacity in LMICs.
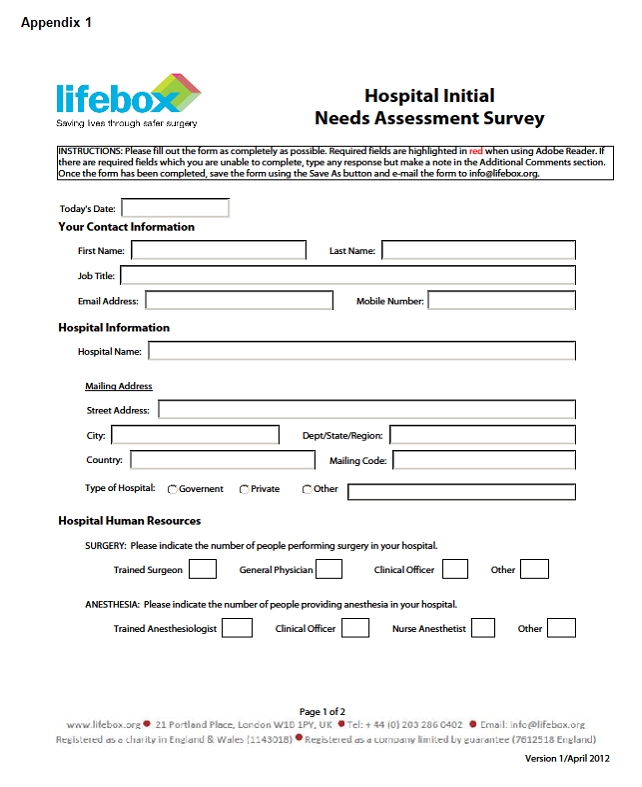
The present survey used a rapid assessment tool known as the Lifebox Hospital Initial Needs Assessment questionnaire with another structured questionnaire to assess anaesthesia services in public hospitals in the Cross River State (CRS) of Nigeria. Lifebox (www.lifebox.org) is a non-profit organization saving lives by improving the safety and quality of surgical care in low-resource countries.19 Since 2001, Lifebox has trained more than 2000 anaesthesia providers, and more than 4200 pulse oximeters have been supplied to more than 70 low-resource countries thereby closing the operating room pulse oximetry gap in about 15 countries.19 This organization is supported by the World Federation of Societies of Anaesthesiologists (WFSA), Association of Anaesthetists of Great Britain and Ireland, Harvard School of Public Health and the Brigham and Women’s Hospital in Boston, United States of America.19 This survey was primarily aimed at the secondary health care facilities which are owned and managed by the CRS Ministry of Health (MOH). This survey audit will identify the anaesthesia providers in CRS, their level of training and retraining as well as equipment available for providing safe anaesthesia and monitoring patients in the peri-operative period. The data will also identify baseline information and gaps in anaesthesia and surgical capacity as a first step for the CRS MOH initiative to improve surgical and anaesthesia services. This information is a stepping-stone for national and international assistance since CRS is a relatively poor state in the Nigerian Federation.
Country and State overview
Nigeria is the most populous African country, located in the West African sub-region with a population of more than 160 million people.20 It is a Federal Republic with 36 states and a Federal Capital Territory. It is politically sub-divided into six geo-political zones: North-Central, North-Eastern, North-Western, South-Eastern, South-South and South-Western. There are 774 Local Government Areas (LGAs) where more than 60% of the population reside. The health care system is divided into three levels: primary, secondary and tertiary. There are public and private health facilities operating at all levels. The primary healthcare facilities (health centres) are managed by the Local Government, the secondary healthcare facilities (general hospitals) are managed by the State Government, while the tertiary facilities (University Teaching Hospitals and Federal Medical Centres) are managed by the Federal Government. Health indicators for Nigeria are among the worst in the world despite the fact that Nigeria is the sixth largest exporter of crude oil. The United Nations Human Development Index ranked Nigeria 156 out of 187 countries.21 In particular, Nigeria is one of the five countries contributing more than 50% to the global maternal mortality ratio22 and one of the countries with the highest physician’s and nurse’s emigration to developed countries.23 Physicians and nurses who remain in Nigeria predominantly practice in urban cities leaving the LGAs, most of them rural with severe shortages in health manpower.
CRS, with approximately 3.2 million population and 20156 square kilometres, is located in the South-South geo-political zone.24 The state has boundaries with the Republic of Cameroon in the East, Benue State in the North, Ebonyi State in the North West and Akwa-Ibom State in the South.24 It is divided into 18 LGAs with 18 general hospitals and 613 primary health centres. There is only one tertiary health facility, the University of Calabar Teaching Hospital (UCTH) located in Calabar, the capital city, which provides specialist care to the entire population. Being a tourism state, the importance of safe anaesthesia as a component of safe surgery cannot be overemphasized.
Physician-anaesthetist, nurse-anaesthetist and surgery training programs in Nigeria
Physicians are trained to be specialist anaesthetists or surgeons in a four-year training program leading to the Fellowship in Anaesthesia (FMCA) or Surgery (FMCS) of the National Postgraduate Medical College of Nigeria (NPMCN) or the Fellowship in Anaesthesia or Surgery (FWACS) of the West African College of Surgeons (WACS). This is after a six-year medical education program in the university leading to the Bachelor of Medicine and Bachelor of Surgery degree, one-year rotatory internship, and one-year of compulsory National Youth Service. Most Fellows, after completion (average time of completion is 7-8 years), work in University Teaching Hospitals and Federal Medical Centres, all located in urban cities. Another training program for doctors designed for primary and secondary healthcare is the Diploma in Anaesthesia (D.A) of the Universities or WACS, which is a 12-month training program. There is no short training program in Surgery.
Nurses are trained as nurse-anaesthetists after 18 months of training in a post-basic nursing program. The basic nursing training program is three-years of training in general nursing, after completing six years of secondary school education. There are now few university degree programs leading to the Bachelor’s degree in Nursing Science (BSN) from the universities. All these nursing training programs lead to certification by the Nursing and Midwifery Council of Nigeria.
Rural-urban practice
Physician-anaesthetists (Fellows and Diplomates), nurse-anaesthetists and consultant surgeons are all concentrated in urban hospitals leaving the rural areas and urban slums with a critical shortage of anaesthetic and surgical workforce. Therefore the majority of the surgical and anaesthetic procedures in rural areas in Nigeria are carried out by government-employed medical officers with almost all anaesthesia being provided by nurse-anaesthetists. In some very remote districts, Community Health Extension Workers (CHEWs) and Community Health Aids with little or no formal training in providing surgical care, are the only health workers available to provide some form of surgical care. The Association of Rural Surgical Practitioners of Nigeria (ARSPON) has been making some effort to address this workforce gap in rural areas by providing short on-the job training for medical officers to enable them to provide safe and affordable surgery to the rural population.13 The concept of surgical task-shifting to “non-physician clinicians” to address this rural-urban surgical workforce disparity, as is being officially done in other LMICs of SSA25 is not acceptable in Nigeria.
METHODOLOGY
A standardized questionnaire, the Lifebox Hospital Initial Needs Assessment Survey (Appendix 1) and another structured questionnaire (Appendix 2) was distributed to all 18 general hospitals (secondary health facilities) in CRS. All the general hospitals, which are the first referral hospitals in the districts, perform surgery. The site visit was conducted in April/May 2014. Permission to conduct the site visit was given by the CRS Honorable Commissioner for Health. The hospital surveys did not involve face-to-face interviews with the medical superintendents, hospital matrons or anaesthesia providers. The questionnaires were to be completed by the anaesthesia providers and medical superintendents in each of the hospitals visited. Each completed questionnaire was to be sent to the office of the Honorable Commissioner for Health at the MOH headquarters in Calabar, the capital city. The results are presented in frequency tables and charts.
RESULTS
A total of 16 well-completed questionnaires were received from 18 general hospitals/secondary healthcare facilities visited (88.9 % response rate). Averages of 3 - 53 surgeries are performed monthly in each of the hospitals (Table 1). The common procedures performed include: herniorrhaphy, appendicectomy, caesarean section, myomectomy, prostatectomy and exploratory laparotomy (Table 1). There are no practicing physician anaesthesiologists or surgeons employed by the State MOH except for one visiting consultant anaesthesiologist and five visiting consultant surgeons from the University of Calabar Teaching Hospital (UCTH), at the General Hospital, Calabar, which is located in the capital city of the State (Table 1). There are 13 nurse-anaesthetists distributed unevenly in the 16 hospitals (Table 1). There are no clinical officers cadres in the Nigerian healthcare system. Apart from the nurse-anaesthetists at the General Hospital in Calabar and Dr Lawrence Henshaw Memorial Hospital, also in Calabar, the other nurse-anaesthetists have had no refresher course or in-service training in the past two years. In the 16 general hospitals, the commonest anaesthetic technique used is Total Intravenous Anaesthesia (TIVA) with Ketamine (Table 1).
Table 1 : Summary of audit of anaesthesia services in the 16 district hospitals in Cross River State, April/May2014
| Hospital |
Number of anaesthetists |
Type of anaesthesia administered | Scope of surgery | Average number of surgeries | Refresher course within last two years | |
| Nurse-anaesthetist | Physician-anaesthetist | |||||
| General Hospital, Obubra | 0 | 0 | Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, | 10 | No |
| General Hospital, Ogoja | 4 | 0 | GA(ETT), Spinal, Local, Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy & Others | 15 | No |
| General Hospital, Sankwala | 1 | 0 | Local | Others | 11 | No |
| General Hospital, Okpoma | 0 | 0 | Local, Ketamine | Herniorrhaphy, Appendicectomy & Others | 3 | No |
| General Hospital, Calabar | 1 | 1 (Visiting) | GA (ETT), Face Mask, Spinal, Epidural, CSE, Local, GA(Ketamine) | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy & Others | 53 | Yes |
| General Hospital, Ugep | 1 | 0 | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy & Others | 18 | No | |
| Cottage Hospital, Oban | 0 | 0 | Ketamine | Herniorrhaphy, C/S, Appendicectomy, Myomectomy | 4 | No |
| Cottage Hospital, Akpet | 0 | 0 | Local, Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy. | 10 | No |
| Lutheran Hospital, Yahe | 1 | 0 | Local, Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy & Others | 5 | |
| Eja Memorial Joint Hospital, Itigidi | 1 | 0 | Local, Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy | 15 | No |
| St. Joseph Hospital, Akpabuyo | 1 | 0 | Local, Spinal, Ketamine | Herniorrhaphy, C/S, Appendicectomy, Myomectomy | 5 | No |
| Dr. Lawrence Henshaw Memorial Hospital, Calabar South | 1 | 0 | GA (ETT), Face Mask, Local, Ketamine | Herniorrhaphy, Laparotomy, Appendicectomy, Myomectomy & Others | 10 | Yes |
| General Hospital, Ukem, Odukpani | 0 | 0 | Ketamine | Herniorrhaphy, Appendicectomy | 3 | No |
| Ranch Medical Center, Obudu | 1 | 0 | Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy | 5 | No |
| General Hospital, Akamkpa | 1 | 0 | Local, Ketamine | Herniorrhaphy, Laparotomy, C/S, Appendicectomy, Myomectomy | 20 | No |
| Government House Clinic, Calabar | 0 | 0 | Local, Ketamine | Herniorrhaphy, Laparotomy, Appendicectomy | 3 | No |
| TOTAL | 13 | 1 (Visiting) | 190 | |||
GA: General Anaesthesia. ETT: Endotracheal Intubation. C/S: Caesarean Section. CSE: Combined Spinal and Epidural anaesthesia.
Basic anaesthetic equipment such as anaesthetic machines, oxygen cylinders, suction machines, and pulse oximeters were lacking in most of the hospitals visited (Box 1).
| Box 1. Summary of Equipment in the 16 General Hospitals, Cross River State, Nigeria: April-May 2014 · 10% of the hospitals had pulse oximeter · 20% of the hospitals had oxygen cylinders · 20% of the hospitals had suction machines · 30% of the hospitals had anaesthetic machines · 80% of the hospitals had recovery beds · 100% of the hospitals perform surgery |
The WHO Surgical Safety Checklist Information was administered to the hospitals management team at the Districts Hospital (Box 2). This shows that all the surgical teams had never used the WHO checklist, never received training, and the checklist was not available in the operating rooms, although all surgical personnel would like to receive training on the WHO checklist and pulse oximetry
| Box 2. World Health Organization (WHO) Surgical Safety Checklist Information · How often do the surgical teams at your hospital use the WHO Surgical Safety Checklist? NEVER · Has your hospital received training in the WHO Surgical Safety Checklist? NO · Is the WHO Surgical Safety Checklist available in your operating rooms? NO · Would you like to receive training in pulse oximetry and the WHO checklist? YES |
DISCUSSION
This survey aimed to provide a quick assessment of anaesthesia and surgical services in public hospitals in CRS of Nigeria. The data shows gross and significant shortages in anaesthesia and surgical providers in all 16 general hospitals. There were no consultant anaesthetists, diplomate anaesthetists or consultant surgeons employed in the CRS MOH. There were only 13 nurse-anaesthetists working in the 16 general hospitals, and one visiting consultant anaesthetist and five visiting consultant surgeons at the General Hospital, Calabar, the capital city. In six of the hospitals, there were no nurse-anaesthetists providing care for the surgical procedures being conducted. As it has been reported from the many surveys in SSA.6, 18, 26 most of the procedures in all the hospitals are being done by generalist medical doctors and general nurses, many without any postgraduate training in surgery and anaesthesia.
The gross inadequacy of the anaesthetic workforce in this survey represents what is found in many of the 778 LGAs (Districts) in the Federal Republic of Nigeria. This is because many of the LGAs are rural and studies have indicated the general difficulties of most health workers seeking jobs in rural hospitals. The lack of specialist anaesthetists in peripheral hospitals in most of Nigerian Districts therefore requires a re-direction of the training programs for doctors in Nigeria with greater emphasis on the shorter training program design for primary and secondary healthcare levels. Inaddition, annual refresher courses should be made mandatory for nurse-anaesthetists especially for those practicing in rural areas.
A recent review of the met and unmet needs of surgical disease in rural SSA, where district and rural hospitals are the main providers of care, shows a very huge burden.27 An important finding is the discrepancy between surgical care needs and provision.27 Since the majority of the population in SSA reside in rural areas, there is the need to strengthen the surgical services at this level. This is the first of the four recommendations of the Bellagio Essential Surgery Group.28 Many of the surveys using the WHO Situational Analysis Tool have described the lack of capacity in many district hospitals to meet the local surgical and anaesthesia needs.6-18 One study, using pulse oximeter availability as a measure of operating room resources, showed that between 58.4% and 78.4% of operating rooms in West Africa, East Africa and Central SSA do not have pulse oximeters.29 This finding was also clearly shown by our own rapid survey and assessment. Three important factors have been responsible for these findings. These are lack of resources, lack of manpower and the need for training.27 The need for training to improve the quality of the surgical and anaesthesia providers at the district hospitals is the third recommendation of the Bellagio Essential Surgery Group.28
Training programs and improvement of the facilities at the District Hospital has been shown to increase the number of operations performed.27Also, the presence of a visiting consultant anaesthetist in the District Hospital has been shown to increase the scope of anaesthesia services during the visiting period.30 The visit left more knowledgeable local staff in the care of their patients especially in peri-operative care.30 The need for developing countries in SSA, particularly in Nigeria, to concentrate more on shorter training programs in surgery and anaesthesia at their current level of development has been advocated.31,32 This has been shown by Sani et al where a 12-month training program for General Practitioners in district hospitals in Niger significantly reduced the number of referrals to the regional and specialist hospital.33 In many other SSA countries, where gross shortages of medical manpower exist, surgical task shifting has been championed and research has shown that these are cost effective interventions.25, 34 This is, however, not acceptable in Nigeria which is Africa’s most populous country with very poor health indicators.
There are some limitations to this study. Firstly, it was a snapshot of anaesthesia and surgical services which did not highlight in detail the eight key areas of surgical and anaesthesia care, as in other surveys. These key areas include: access and availability of hospital services, human resources, physical infrastructures (including availability of water and electricity), surgical and anaesthetic procedures, surgical and anaesthesia outcome, essential equipment availability, NGO and international organizations providing care, and access to essential pharmaceuticals. Secondly, this assessment did not include the only public tertiary hospital in the State and private hospitals. Lastly, this was an initial assessment in preparation for a more detailed survey based on the WHO guidelines when research funds are received.
CONCLUSION AND RECOMMENDATIONS
Therehas been a paradigm shift in global public health and the concept of primary healthcare which has resulted in increased awareness of the importance and contributions of surgical disease to the overall burden of disease especially in LMICs. This rapid survey of anaesthesia services in CRS, one of the 36 states in Nigeria, will serve as a window to inform other Nigerian State governments of the need to increase surgical and anaesthesia capacity and funding in their development agenda. It is therefore recommended that visiting consultant’s services to all the general hospitals in an organized and planned fashion should be highly encouraged. All the anaesthesia caregivers should attend refresher courses at least once every two years. These courses can be arranged locally, or sponsorship provided for attendance of relevant courses by Anaesthesia Trainers within and outside the State. Basic anaesthesia equipment and guidelines as recommended by the Nigerian Society of Anaesthetists (Box 3) must be available and followed to enhance patient safety. It is also recommended that the government should give incentives to medical and nursing staff working in rural areas so that there will be a reversal of the rural- urban shift. The Lifebox global oximetry project is interested in making high quality, low-cost pulse oximeters available in every operating room. Therefore, every secondary care facility in the country should take advantage of this laudable program.
| Box 3. Nigerian Society of Anaesthetists Standard Guidelines for the Practice of Anaesthesia Anaesthetic Personnel · Certified physician anaesthetist · Trained nurse-anaesthetist under supervision by physician-anaesthetists · Maximum number of nurses to physicians should be 4:1 · Where there is no physician-anaesthetist, nurses should adhere strictly to the guidelines and conditions of their certification · The surgeon should provide coverage especially in the area of patient resuscitation and fitness for surgery and take full responsibility for any decisions made against the guidelines. Anaesthetic equipment for each theatre |

|
Acknowledgements The authors are grateful to the CRS Honorable Commissioner for Health for giving us the permission to carry out this survey. We are also thankful to the medical and nursing staff of all the sixteen secondary health care facilities for making this survey a reality. Special acknowledgement goes to LIFEBOX for the donation of thirty (30) free pulse oximeters to improve anaesthetic practice as a result of this survey. This study was carried out in collaboration between all authors. QNK and AIE conceived and designed the study, and QNK visited the hospitals and distributed the questionnaires. EIU, AUE and EM managed the literature searches and reviews, and wrote the first draft. All authors read and approved the final manuscript. Competing Interests None declared Author Details QUEENETH NDUKWE KALU, MB, BCH, DA, FWACS, DA (WFSA), Consultant Anaesthesiologist, UCTH, Calabar, Cross River State, Nigeria. ATIM IMEH ESHIET, MB, BCH, DA, FMCA, FICS, FWACS. Consultant Anaesthesiologist/Professor - UCTH, Calabar, Cross River State, Nigeria. ESSIEN ITA UKPABIO, MB, BCH, DA. Senior Registrar in Anaesthesiology - UCTH, Calabar, Cross River State, Nigeria. ANIETIMFON UMOH ETIUMA, MB, BCH, FMCS, FWACS. Consultant Surgeon/Professor - UCTH, Calabar, Cross River State, Nigeria. EMMANUEL MONJOK, MD, MPH. Visiting Consultant, Family Medicine/Public Health - UCTH, Calabar, Cross River State, Nigeria. CORRESPONDENCE: Dr Queeneth N. Kalu. Department of Anaesthesiology, University of Calabar Teaching Hospital, Calabar, Nigeria. Email: queen_kalu@yahoo.com |
References
- Spiegel, DA, Abdulla F, Price RR, Gosselin RA, Bickler SW. World Health Organization Global Initiative for Emergency and Essential Surgical Care: 2011 and Beyond. World J Surg 2013; 37: 1462-1469.
- Lavy, C, Suaven K, Mkandawire N, Charian M, Gosselin R, Ndihokubwayo JR, Parry E. State of Surgery in Tropical Africa: A Review. World J Surg 2011; 35: 262-271.
- Farmers PE, Kim JY. Surgery and Global Health: a view from beyond the OR. World J Surg 2008; 32: 533-536.
- Debas H, Gosselin R, Mc Cord C et al. Surgery. In: Jamison DT, Breman JG, Measham AR et al (Eds) Disease Control Priorities in Developing Countries, 2ed. Oxford University Press. New York, 2006; pp1245-1259.
- WHO. www.who.int/surgery, accessed August 30, 2013.
- Reshamwalla S, Gobeze AA, Ghosh S, Grimes C, Lavy C. Snapshot of surgical activity in rural Ethiopia: Is enough being done? World J. Surg.2012; 36(5): 1049.
- Iddriss A, Shivute N, Bickler S, Coley-Sessay R, Jargo B, Abdulla F, Cherian M. Emergency anesthetic and essential surgical capacity in The Gambia. Bull World Health Organ 2011; 89(8): 565-572.
- Kushner AL, Cherian MN, Noel L, Spiegel DA, Groth S, Etienne C. Addressing the Millennium Development Goals from a surgical perspective: essential surgery and anesthesia in 8 low-and-middle income-countries. Arch. Surg.2010; 145 (2): 154-159.
- Abdulla F, Choo S, Hesse AA, Abantanga F, Sory E, Osen H, Ng J, McCord CW, Cherian M, Fleischer-Djoleto C, Perry H. Assessment of surgical and obstetrical care in 10 district hospitals in Ghana using on-site interviews. J. Surg Res 2011; 171(2): 461-466.
- Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H, Fleischer-Djoleto C, Moresky R, McCord CW, Cherian M, Abdullah F. Assessment of capacity for surgery, obstetrics and anesthesia in 17 Ghanaian hospitals using the WHO assessment tool. Trop Med Int Health 2010; 15: 1109-1115.
- Sherman L, Clement PT, Cherian MN, Ndayimirije N, Noel L, Dahn B, Gwenigale WT, Kushner AL. Implementing Liberia’s poverty reduction strategy: an assessment of emergency and essential surgical care. Arch Surg 2011; 146(1): 35-39.
- Lavy C, Tindall A, Steinlechner C, Mkandawire N, Chimangeni S. Surgery in Malawi- a national survey of activity in rural and urban hospitals. Ann R Coll Surg Engl 2007; 89(7): 722-724.
- Henry JA, Windapo O, Kushner AL, Groen RS, Nwomeh BC. A Survey of Surgical Capacity in Rural Southern Nigeria: Opportunities for Change. World J Surg 2012; 36: 2811-2818.
- Kingham TP, KamaraTB, Cherian MN, Gosselin RA, Simkins M, Meissner C, Foray-Rahall L, Daoh KS, Kabia SA, Kushner AL. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg 2009; 144(2): 122-128.
- Notrica MR, Evans FM, Knowlton LM, Kelly-McQueen KA. Rwanda surgical and anesthetic infrastructure: a survey of district hospitals. World J Surg 2011; 35: 1770-1780.
- Petroze RT, Nzayisenga A, Rusanganwa V, Ntakiyiruta G, Caland JF. Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. Br. J. Surg 2012; 99(3): 436-443.
- Penoyar T, Cohen H, Kibatala P, Magoda A, Saguti G, Noel L, Groth S, Mwakyusa DH, Cherian M. Emergency and surgical services of primary hospitals in the United Republic of Tanzania. BMJ 2012; Open 2(1): e000369.
- Linden AF, Sekidde PS, Galakande M, Knowlton LM, Chackungal S, McQueen KA. Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J. Surg 2012; 36: 1056.
- Lifebox www.lifebox.org, accessed August 30, 2013.
- The World Factbook (2009). Washington DC (updated 2012 July). Available at: https://www.cia.gov/library/publications/the-world-factbook/index/html accessed August 31, 2013.
- Human Development Index (HDI) value (2012). Available at: http://hdrstats.undp.org/en/ingicators/103106.html, accessed August 31, 2013.
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela M et al. Maternal Mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010; 8; 275(9726): 1609-1623.
- Kasper J, Bajunirvve F. Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centers. Arch. Dis. Child 2012; 97: 973-979.
- National Population Census; Cross River State, Federal Republic of Nigeria Official Gazette, 2009; 2; B25-B26.
- Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet 2007; 370: 2158-2163.
- Hodges SC, Mijumbi C, Okello M, McCormick BA, Walker IA, Wilson IH. Anaesthesia services in developing countries: defining the problems. Anaesthesia 2007; 62: 4-11.
- Grimes CE, Law RSL, Borgstein ES, Mkandawire NC, Lavy CBD. Systemic review of met and unmet need of surgical diseases in rural sub-Saharan Africa. World J Surg 2012; 36: 8-23.
- Lubuga S, Macfarlane SB, Von Schreeb, T et al. Increasing Access to Surgical Services in sub-Saharan Africa: Priorities for National and International Agencies recommended by the Bellagio Essential Surgery Group. PloS Med 2009; 6(2): 1-5.
- Funk LM, Weiser TG, Berry WR et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet 2010; 376(9746): 1055-1061.
- Kalu QN. The Influence of a consultant anesthetist in a nurse-led anesthetic service. African J. Anesth. Intensive Care 2008; 8(1): http//dx.doi.org/10.4314/ajaic.v8i1.47975
- Monjok E, Essien EJ, Smesny A, Okpokam SN. A training need for rural primary care in Nigeria. J. Obst.Gynae 2010; 35(8): 833-835.
- Monjok E, Essien EJ. Mobile surgical services in primary care in a rural and remote setting: Experience and evidence from Yala, Cross River State, Nigeria. Afr J. Primary Health Care. Family Med 2009; 1(1): Art # 31, 4 pages. Dot: 40. 4102/phcfm.v1i1.31.
- Sani R, Numeroua B, Yahaya A. The impact of launching surgery at the district level in Niger. World J. Surg 2009; 33: 2063-2068.
- Chu K, Rosseel P, Gielis P et al. Surgical task-shifting in sub-Saharan Africa. PloS Med 2009; 6(5): e1000078.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




