Prevalence and Pattern of Self Medication use in coastal regions of South India
Balamurugan E and Ganesh K
Cite this article as: BJMP 2011;4(3):a428
|
|
Abstract Aim:Self medication (SM) is proportionately increasing in both urban and rural communities. The prevalence and pattern of SM use is not well established, hence a cross sectional survey was undertaken which recruited a sample size of 200 participants randomly from the coastal regions of south India. |
Introduction
William Osler has said that "A desire to take medicine is perhaps the great feature which distinguishes man from animals" This desire, however may play havoc when a person starts taking medicines on their own (i.e. self-medicating), forgetting that all drugs are toxic and their justifiable use in therapy is based on a calculable risk 1.
Self-medication (SM) can be defined as obtaining and consuming drugs without the advice of a physician2. There is a lot of public and professional concern about the irrational use of drugs in SM. In developing countries like India, easy availability of a wide range of drugs coupled with inadequate health services result in increased proportions of drugs used as SM compared to prescribed drugs2. Although, over-the-counter (OTC) drugs are meant for SM and are of proved efficacy and safety, their improper use due to lack of knowledge of their side effects and interactions could have serious implications, especially in extremes of ages (children and old age) and special physiological conditions like pregnancy and lactation 3, 4. There is always a risk of interaction between active ingredients of hidden preparations of OTC drugs and prescription medicines, as well as increased risk of worsening of existing disease pathology 5 . As very few studies have been published in our community regarding usage of self medication we conducted this cross-sectional study in the coastal region of Pudhucherry, South India, t assess the prevalence and pattern of SM use.
Materials and methods:
The present study was a cross-sectional survey conducted in coastal region of pudhucherry, south India. For this study we recruited 200 patients randomly from both urban and rural communities (100 each) for a period of six months during 2009. Patients who were = 18 years of age and who were able to read and write the local language (Tamil) or English were included in the study after informed consent explaining the purpose of the study. Participants with intellectual, psychiatric and emotional disturbances that could affect the reliability of their responses were excluded from the study. To collect data regarding SM usage a structured questionnaire was prepared, after an extensive literature review.. The structured questionnaire contained 25 items in the form of closed and open ended questions. Initially the tool was validated by a panel of experts in the field of public health for the appropriateness of each item and assessment of content validity (0.91) and re-test reliability coefficient (0.89). Approval to conduct the study was granted by the Institute ethics committee prior to data collection. Each participant underwent a face to face interview to collect data followed by an informal educational counseling about potential adverse effects of consuming common SM. Data collected was analyzed using SPSS for windows statistical software version 14 (SPSS Inc., Chicago, Il, USA). Data was presented using descriptive statistics (i.e. numbers, percentage) and inferential statistics (i.e. Chi-square). A probability value of < 0.05 was considered to be significant.
Results
Basic demographic details:
The majority of the participants were female (56%). Most of the participants (60%) were between 26-45 years of age. There were an equal number of participants from the rural and urban community. Among the total 200 participants 70% were literate.
Findings related to usage of SM:
Overall, out of 200 participants, 71 % of them reported that they have used SM in the past. The frequency of SM use varied among the subjects with a minimum of at least one time to maximum of 5 times and above See Figure 1. When the participants were asked about the reasons for SM use, the majority of them - 41.5% - stated lack of time to visit a doctor as the main reason followed by minor illness and quick relief. See Table 1. The major source through which the participants learned to use SM were as follows, directly from pharmacist (57.3%), prescription of previous illness (21.5%), friends (12.5%), television (5.5%) and books (3%).See Table 2. The main indications for SM use were fever (36%), headache (35%), then cough/cold/sore throat (20%). See Table 3 for detailed data.
Figure 1: Frequency of self medication Use
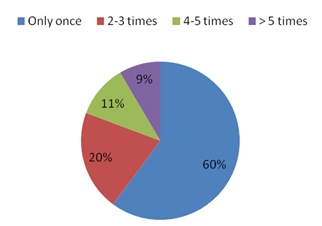
Table 1: Reasons for Self Medication Use
| Reasons | Number (%) |
| Lack of time | 41.5 |
| Minor illness | 10.5 |
| Economical | 14 |
| Quick relief | 10 |
| Learning opportunity | 2 |
| Ease and convenience | 10.5 |
| Avoiding crowd in visiting doctor | 6 |
| Unavailability of doctor | 5.5 |
Table 2: Sources of Self Medication Use
| Sources for self medication use | Number (%) |
| Directly from pharmacy without prescription | 57.3 |
| Prescription of previous illness | 21.5 |
| Friends prescription | 12.5 |
| Television media | 5.5 |
| Book | 3 |
Table 3: Indications for Self Medication Use
| Indications for self medication use | Number (%) |
| Headache | 35 |
| Stomach ache | 3 |
| Vomiting | 1 |
| Eye symptoms | 0.73 |
| Diarrhoea | 2 |
| Cough, cold, sore throat | 20 |
| Fever | 36 |
| Skin symptoms | 0.27 |
| Ear symptoms | 2 |
While calculating chi-square to find out the association between usage of SM and selected demographic variables we found an association between residence (i.e. rural or urban) and gender; urban people were more likely to use SM than rural people (urban, 60/100 vs. rural 82/100, p value = .006). In relation to gender females were more likely to use SM in comparison to males (female, 78/112 vs. 43/88, p value= .002). Other variables were not significantly associated with SM use. Finally, when the subjects were asked about the side effects of their used self medications 93.5% of them said that they are not aware of the side effects and only the remaining 6.5% of them said they are aware of the side effects.
Discussion
The current study examined the prevalence and pattern of SM use in a coastal region of South India. The study findings revealed 71% of the people reporting SM use in the past, this prevalence rate in our study is consistent with previous finding3,6,7,8,9,10,11 The figure of participants who use SM is very high, which requires immediate attention. The frequency of self medication use in our study ranged from a minimum of one time to a maximum of 5 times and above, this finding was in line with the findings of a study by Nalini (2010)12.
Participants cited multiple reasons for use of SM like lack of time , quick relief from illness and ease and convenience, a similar reasons were cited in an another Indian study13. In the current study participants reported SM use in a variety of conditions like headache, stomach ache, cough and fever, this these finding are comparable with those of Sontakke et al (2011) 14. The reason for SM use may be mufti-factorial, in our study an association was found between gender and residence, i.e. female and rural people reporting more SM use, this finding was similar to two previous studies15,16 To establish the reasons why requires further research. One potential limitation of this study is the limited sample size, which we tried to overcome by adopting a random sampling method so as to generalize findings.
Conclusion
Factors influencing SM include patient satisfaction with the healthcare provider, cost of the drugs, educational level, socioeconomic factors, age and gender 17. Interactions between prescribed drugs and the drugs taken for SM is an important risk factor of which healthcare providers must be aware of.17,2
Easy availability of wide range of drugs without a prescription is the major factor responsible for irrational use of drugs in SM as, thus resulting in impending health problems (antimicrobial resistance, increased load of mortality and morbidity) and economic loss. The need for promoting appropriate use of drugs in the health care system is not only for financial reasons, with which policy makers and manager are usually most concerned, but also for health and medical care of patients and the community. There is need for authorities to strengthen existing laws regarding OTC drugs to ensure their rational sale and use. Also, specific pharmacovigilance is needed and the patient, pharmacist and physician must be encouraged to report any adverse events. Periodic studies on the knowledge, attitude about and practice of SM may give insight into the changing pattern of drug use in societies.
|
Acknowledgements The author is grateful to all study participants who willingly participated in the study. Competing Interests None declared Author Details BALAMURUGAN E. (R.N, R.M, M.Sc.), Research Scholar, College of Nursing, All India Institute of Medical Science, New Delhi, India. GANESH K. (R.N, R.M, M.Sc), Research Scholar, College of Nursing, All India Institute of Medical Science, New Delhi, India CORRESPONDENCE: Balamurugan E., Research Scholar, College of Nursing, All India Institute of Medical Science, Ansari Nagar, New Delhi -110029, India Email: bmbalanursing@gmail.com |
References
- Phalke VD, Phalke DB, Durgawale PM. Self-medication practices in rural Maharashtra. Indian J Community Med .2006; 31:34-5.
- Montastruc JL, Bagheri H, Geraud T, Lapeyre MM. Pharmacovigilance of self-medication. Therapie 1997;52:105-10
- Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal; a questionnaire based study. BMC Fam Pract. 2002;3:17
- Murray MD, Callahan CM. Improving medication use for older Adults: An integrated research agenda. Ann Intern Med 2003;139:2425-9
- Choonara I, Gill A, Nunn A. Drug toxicity and surveillance in children. Br J Clin Pharmacol. 1996;42:407-10
- Sharma R, Verma U, Sharma CL, Kapoor B. Self-medication among urban population of Jammu city. Indian J Pharmacol. 2005;37:40-3
- Kasilo OJ, Nhachi CF, Mutangadura EF. Epidemiology of household medications in urban Gweru and Harare. Cent Afr J Med. 1991;37:167-71
- Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005 Aug 12;8(2):326-31.
- Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MA. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20(4):373-80.
- Richman PB, Garra G, Eskin B, Nashed AH, Cody R. Oral antibiotic use without consulting a physician: a survey of ED patients. Am J Emerg Med. 2001 Jan;19(1):57-60.
- Cagri Buke A, Ermertcan S, Hosgor-Limoncu M, Ciceklioglu M, Eren S. Rational antibiotic use and academic staff. Int J Antimicrob Agents. 2003 Jan;21(1):63-6.
- Berzanskyte A, Valinteliene R, Haaijer-Ruskamp FM, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19(4):246-53.
- Nalini GK. Self Medication Use Among allopathic Medical Doctors in Karnataka, India. British Journal of Medical Practioner. 2010; 3(2):325.
- Kayalvizhi S, Senapathi R. International Journal of Enterprise and Innovation Management Studies.2010; 1(3): 40-44.
- Sontakke SD , Bajait CS , Pimpalkhute SA, Jaiswal KM, Jaiswal SR. International Journal of Biological & Medical Research. Int J Biol Med Res. 2011; 2(2): 561-564
- Figueiras A, Caamano F, Gestal OJJ. Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26
- Hebeeb GE, Gearhart JG. Common patient symptoms: patterns of self-treatment and prevention. J Miss State Med Assoc. 1993; 34:179–181.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




