Predicting falls risk in patients – the value of cardiovascular variability assessment
Simon Freilich and Robert Barker
Cite this article as: BJMP 2009:2(4) 44-48
|
|
Abstract Objective: To test the hypothesis that an individual’s falls risk is a continuum and that physiological variation in the routine nursing observations in the lead up to the fall can be used to predict its occurrence when compared to the general hospital population. Methods: This study was a retrospective case-control study.13 Fallers were randomly selected and compared to 47 Controls matched for age, sex and equivalent length of stay. Routine nursing observations such as heart rate, systolic blood pressure, respiratory rate, temperature and patient at risk (PAR) scores were recorded and compared over the 12 hours preceding the fall. Data was compared using a Student Unpaired T-Test with Power calculated as > 80%. Variability was quantified by the range and standard deviation of the values for each parameter.Results: The average (±SD) age of fallers in years (79 ± 16) was higher than of general medical admissions (67 ± 20) p<0.003. There was a predisposition to men falling (63%, p<0.001) compared to women. 70% were taking over 4 medications and most of the injuries were minor. The overall PAR score, temperature and respiratory rates were not predictive of falls and neither was their variability. There were no significant differences between the recorded heart rates or blood pressures between fallers and controls; however, there was much greater variation in both. The range of heart rate variation was 15 ± 10 bpm in fallers, and 7 ± 7 bpm in controls p<0.001. The range of systolic blood pressure variation was 26 ± 12 mmHg in fallers and 11 ± 7 mmHg in controls p<0.001. Orthostatic hypotension was recorded in 2 patients prior to their falls.Conclusions: Cardiovascular variation as measured by increasing range is an acute predictor of falls risk despite relatively normal absolute values. This implies that falls risk should be regarded as a continuum, above and beyond recognised basal risk factors. We therefore recommend that falls risk should become an integral part of patients’ daily assessments and incorporate the patients’ physiology together with pre-existent pathology Keywords: Falls, Heart Rate, Blood Pressure, Cardiovascular, Variability |
IntroductionHospital inpatient falls have remained the subject of extensive research and intervention over the past 55 years1. Despite risk factor identification, multiple prediction system developments and harm reducing technologies, the issue of falls remains. The incidence of falls varies between 2.2 and 14 per 1000 patient days 2,3 and increases with age 4. In the UK’s National Health Service, 32% of adverse incident reports are due to falls 2 . In 2007 it reported 200,000 inpatient falls to the National Patient Safety Association 5. Whilst most patients (96%) came to no harm or minor harm, they estimated that over 500 hip fractures and 26 deaths resulted from these falls.Inpatient falls lead to greater morbidity and mortality than equivalent fractures in the community, 6 and they significantly increase the length of stay in hospital7. Apart from physical harm, there are also psychological consequences for patients such as anxiety, loss of confidence, and fear of falling 4. The risk of falls leads to a conundrum in rehabilitative care. Ideally, patients’ mobility, autonomy and dignity must be encouraged and respected - yet slips, trips and falls must be pre-empted often with varying degrees of intrusion and even restraint. In order to selectively target individual patients who would benefit from closer attention, many risk stratification tools have been developed to predict potential fallers. They were developed on a background of over 400 independent risk factors identified with falls 8. The most prominent in the UK are STRATIFY (St Thomas's risk assessment tool in falling elderlyinpatients) and Downton with the recent addition of the Wandering Behaviour Assessment 8. STRATIFY 4 was designed to be used once per week and assesses 5 factors –falls history, patient agitation, visual impairment that limits daily function, frequent toileting, and a transfer or mobility score of 3 or 4 . Each factor scores 1 point and a score greater than 2 was found to have a 92% sensitivity and 68% specificity for a fall in the following week. In the Wandering Behaviour study the STRATIFY criteria results were not reproduced and were found to have only an 82% sensitivity and 34% specificity in their study population 8. Downton 9 also has 5 categories of assessment; falls history, medication subtypes, audio-visual-sensory deficits, mental state (using the Mini Mental State Score <24) and stability of gait. Each category scores 1 point and a score of greater than 3 is considered significant. In the Wandering Behaviour study, when applying the Downton criteria they only found an 82% sensitivity and 36% specificity 8. The Wandering Behaviour assessment looks for the presence of the following :checking, pottering, aimless walking, walking with inappropriate purpose, walking with appropriate purpose but inappropriate frequency, excessive activity, night-time walking, attempts to leave the hospital and being brought back to hospital. The presence of any one of these was found to have a sensitivity of 43% but specificity of 91% 8. Thus, both STRATIFY and Downton are limited by the multi-disciplinary assessments required, so that even when implemented, it is difficult to repeat them on a daily or weekly basis. The Wandering Score is easily repeatable on a daily basis, but lacks the sensitivity of STRATIFY and Downton 8. The aim of this study is to investigate whether changes in a patient’s physiology can be predictive of falls risk, and if so, can they become a useful tool for calculating risk? The reason why we have chosen to investigate this is that many of the commonly encountered risk factors can potentially be reflected in the patient’s routine observations 10. For example, fever could indicate infection and delirium. Hypotension could result from anti-hypertensives, sedatives, or dehydration. Hypertensive states could result from stroke, stress response to infection, or even be a surrogate marker of cardiovascular disease predisposing to arrhythmias. Blood pressure variation could also be predictive since dynamic orthostatic challenges such as lying and standing blood pressure measurements are known to predict falls 10. Thus, by measuring fluctuations in the observations we hypothesised that it may be possible to make an accurate short term prediction of falls risk MethodsSubjectsWe obtained consent for this retrospective study from the hospital’s ethics committee. We based this study in the Acute Medical Unit of our hospital, as it has the largest case mix of patients recently admitted and is therefore most likely to have the largest physiological instability. We aimed to detect a mean difference of 10% in the physiological variability prior to falling with 80% power, p-value < 0.05, and a common standard deviation of 5 %. Our power calculation indicated that we needed to study 12 patients. We identified all the falls in the calendar year of 2008 by examining the records of all the incident report forms submitted by the ward. A total of 33 incident reports related to falls were logged. Two reports related to staff slips and trips and were excluded, and a third incident report failed to adequately identify either the patient’s name, date of birth or hospital number and so had to be excluded. One of the 30 patients fell twice, and this was treated as its own incident as with the STRATIFY paper. The incident report forms were also used to identify the time, nature, and outcome of the fall. Of all the case notes related to the 30 falls requested from medical records, only 13 were available for detailed review. MeasurementsHeart rate (HR), Blood Pressure (BP), Temperature and Respiratory Rates were all recorded and analysed. The PAR (Patient at Risk) Score as calculated by the nursing staff was included too. PAR Scores are validated mechanisms of identifying sick patients who may go on to develop deterioration to the point of requiring Intensive Care. Scores of >3 are associated with a high risk of deteriorating health and are calculated using the routine nursing observations set. Oxygen saturations were not included in this study, as even small deviations tend to be rapidly corrected by staff with oxygen and therefore were not thought to be a useful marker. Recordings of blood pressure and heart rate were all done with ward based equipment. It is impossible to know which machines were used on individual patients as the equipment has varied, both over the course of time, and between multiple wards. However, because the subjects were their own controls, we are confident that the same machine and cuff were used for taking all the 12 hour recordings as each individual machine is allocated to a given bay. Blood pressures were obtained using semi-automatic Dynamap equipment, therefore the readings are in effect calculated from the Mean Arterial Pressure (MAP). We elected to study the systolic readings only, as this represents the maximum perfusion pressure to the brain and carotid sinus. Two of the thirteen patients were known to have undergone orthostatic challenges as part of their admission work up and these were included. Other parameters recorded included the time of the fall, number of medications on the drug chart, whether the fall was observed and any injuries sustained. ControlsWe had two sets of controls. The first set was used to compare the age and gender profile of the fallers to those of the general adult admissions. We had to do this because the official hospital statistics included obstetric and paediatric admissions and comparison would have been inaccurate. We therefore took 4 random days’ of acute adult medical admissions (i.e. over the age of 18) in order to compile an age and gender profile of patients admitted with a ratio of 4:1 (n=110). In order to compare the variability in physiological parameters between fallers and non fallers we generated a second set of controls matched for age (± 5 years) and gender in a ratio of 4 to 1 from a random week’s cohort of patients in February 2009 (for practical purposes). For each matched control, recordings were made at the equivalent length of stay and the controls were not known to have previously fallen. The patients were taken from across the hospital’s medical wards (not Intensive Care or Surgical) with their diagnosis blinded from the investigators. We were able to match 47 of the 52 controls that we were aiming for. Only BP and HR data were recorded in the controls, as we already established that temperature and respiratory rate were not sensitive markers from our faller data. StatisticsOur 13 patients allowed us to reach sufficient statistical power of 80%. Physiological parameters were tested within groups using the Students t-test (paired, two tailed) and when comparing to controls using the Students t-test (unpaired, two tailed). The null hypothesis were rejected when p<0.05. Variability in heart rate, temperature, respiratory rate and PAR (Patient At Risk Score) were calculated using the mean, range and standard deviation between maximum and minimum values. Blood pressure variability was measured by using the maximum and minimum systolic pressure and calculating the mean, range and standard deviation. We have chosen to primarily measure variability by the range as it is a simple calculation that can be done by anyone on a ward. It doesn’t require a calculator nor any detailed knowledge of mathematics. It is therefore an effective and repeatable measure which could be easily implemented as part of a scoring system. Data processing and Statistical Analyses was done in MS Excel 2002 and SPSS v.14. ResultsThe mean age of fallers was 79 years old (SD 16, n=30) and of the acute medical admission controls 67 years old (SD 20, n=110) with p=0.003. The gender distribution of males to females was 63% to 37% respectively for fallers (n=30), but 38% to 62% in general medical take controls (Fishers exact test p<0.001). 54% of fallers (n=13) were admitted from their own home with 31% from Residential Homes and 15% from Nursing Homes. 54% were known to have a preceding falls history (n=13). The timings of the falls showed that 60% of falls occurred between 08.00 and 20.00 (n=30). 77% of falls occurred within 48 hours of admission (n=13). The circumstances of the falls were consistent with the NPSA statistics with 20% falling out of bed, 17% from chair, 17% from commode / toilet, 20% when walking, 3% in the bath and 23% not documented. The significance of the falls as measured by the incident report forms (n=26, in 4 cases not recorded) was 70% under the level of 6 (i.e. low level and did not require further investigation), 13% were over the level of 6 (i.e. were serious and required further investigation) and 17% were unrecorded. Most of the injuries (n=30) were none or minor – 47%, 10% had a head injury and 43% were not recorded. 95% of the falls were not observed. 31% of the patients (n=13) were taking fewer than 4 medications, 38% were taking between 4 and 7 medications and 32% were taking over 8 medications. Comparing the demographic characteristics of our fallers to the age and gender matched controls; average age was 79 for both fallers and controls (p=0.94) and the gender distribution was 7 females : 6 males in the fallers, and 27 females: 21 males in the controls (Fisher’s Exact Test p=1.0). The overall PAR score (n=13) was not sufficiently sensitive to predict falls risk – 77% had no change in their PAR score, 8% had a 1 point change and 15% had a 2 point change ( Table 1). Temperature variation (n=13) was minimal with 69% having less than 1 degree Celsius change and 31% having change of 1 to 1.5 degrees Celsius . Recorded respiratory rate variation was also minor (n=13) with 85% having a maximum change of up to 4 breaths per minute. Table 1. Physiological Parameter Data * denotes p<0.05
| Fallers N = 13Mean ± SDRange (x-x) | Controls N = 47Mean ± SDRange (x-x) | |
| PAR Score | 1.2 ± 0.6(1 – 3) | |
| PAR Score Variability | 0.4 ± 0.6(0 – 2) | |
| Temperature (Celsius) | 37.1 ± 0.5(36.4 - 38.1) | |
| Temperature Variability (Celsius) | 0.6 ± 0.5(0 – 1.3) | |
| Respiratory Rate (Breaths/Minute) | 18.5 ± 1.9(16 – 22) | |
| Respiratory Rate Variability (Breaths/Minute) | 1.1 ± 1.5(0 – 4) | |
| Highest Heart Rate (Beats/Minute) | 86 ± 13(70 - 110) | 86 ± 14(60 -112) |
| Lowest Heart Rate(Beats/Minute) | 71 ± 16(50 -101) | 79 ± 14(55 – 110) |
| *Heart Rate Variability (Beats/Minute) | 15 ± 10(0 – 39) | 7 ± 7(0 – 27) |
| Highest Systolic BP (mmHg) | 142 ± 22(102 – 180) | 140 ± 24(99 – 218) |
| Lowest Systolic BP(mmHg) | 116 ± 19(71 – 150) | 129 ± 24(86 – 199) |
| *Systolic Variability (mmHg) | 26 ± 12(2 – 40) | 11 ± 7(0 – 26) |
In fallers (n=13), the mean highest heart rate was 86 bpm (SD=13) and the mean lowest heart rate was 71 bpm (SD=16). The range was 15 bpm (SD=9.6) with p<0.001. In controls (n=47) the mean highest heart rate was 86 bpm (SD=14) and the mean lowest heart rate was 79 bpm (SD=14). The range was 7 bpm (SD=7) with p<0.001. The significance test when comparing the highest average heart rate between fallers and controls shows p=0.98 showing that they were well matched. The significance test for comparing the variation of the heart rate between fallers and controls is p<0.001. In fallers (n=13), the mean highest systolic BP was 142 mmHg (SD=22) and the mean lowest systolic BP was 116 mmHg (SD=19). The average variation was 26 mmHg (SD=12) with p<0.001. In controls (n=47) the mean highest systolic BP was 140 mmHg (SD=24) and the mean lowest systolic BP was129 mmHg (SD=24). The average variation was 11 mmHg (SD=6.5) with p<0.001. The significance test when comparing the highest average systolic BP between fallers and controls shows p=0.77 showing that they were well matched. The significance test for comparing the variation of the systolic BP between fallers and controls is p<0.001. Charts 1 and 2 show the spread of measurements in the cardiovascular parameters between fallers and controls.
Chart 1. Comparison of the heart rate variation between Fallers and Controls 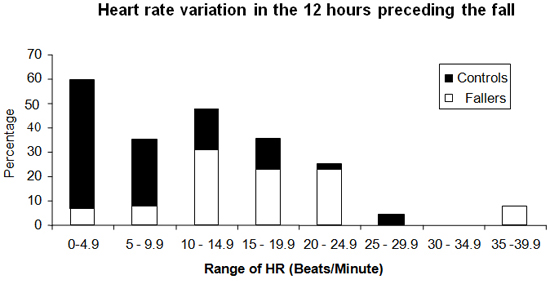
Chart 2. Comparison of the systolic blood pressure variation between Fallers and Controls 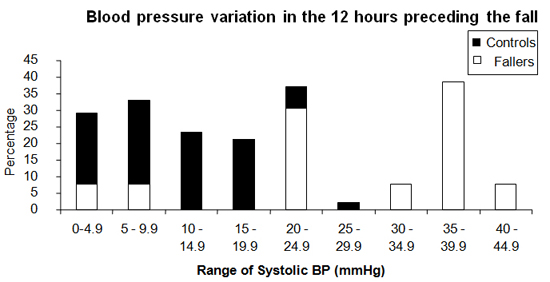
DiscussionThe average age of the fallers was significantly greater than the average age of those admitted to the hospital in general. This is unsurprising considering both mechanical deterioration of the musculoskeletal system with advancing age and the accumulation of disease processes. It is noteworthy that despite making up the smaller percentage of admissions to the hospital, men made up the greater proportion of fallers. Other much larger studies show considerable variability in their gender proportions 11,12, therefore this finding is unlikely to be truly significant. Apart from age and gender, polypharmacy was also a feature of our fallers. This is consistent with other studies 13,14,15. Additionally, our data was consistent with the overall NPSA statistics in terms of the significance and circumstances of the falls 5. The main and novel finding of our study was that fallers were significantly more likely to display a larger range in their cardiovascular observations than the standard hospital population. Whilst it is generally expected that subjects undergoing any routine measurement of heart rate and blood pressure will have a variation in measurements of about 10% over the course of 12 hours 16,17, we found that our fallers had a variation in their heart rate and blood pressure of approximately 20%. This is similar to the dips experienced by the normal population over the course of the night and during orthostatic challenge. This was despite the fact that the baseline measurements of highest value were virtually the same for both populations. Furthermore, almost all the values recorded were within normal limits – and would not normally require specific remedial action to be taken. This could also explain why this risk factor has not previously been identified in other studies. Our study indicates that it is the cardiovascular lability rather than the cardiovascular measurements per se, which acts as an acute predictor of falls. In fact, the sensitivity for falls prediction with either a range of HR values > 15 beats per minute or range of BP systolic values >25 mmHg was 77%. We would therefore expect that when such patients mobilize, the superadded orthostatic challenge would be too great for cardiac output to be suitably matched and so patients are at greater risk of falling. In terms of the 12 hour prospective risk of falling this could certainly explain why a patient with known risk factors will fall during a given nursing shift. Indeed it may also explain why a patient may fall during a hospital admission when patients were, for example, already parkinsonian and arthritic and yet had not previously fallen. Interestingly, neither temperature, respiratory rate, nor PAR Score showed any significant lability in the lead up to the falls. This was surprising as we would have expected them to be predictive of other well known risk factors. The lack of fluctuation in temperature and respiratory rate could provide further evidence that the key short term factor responsible for falls is cardiovascular lability. More detailed analysis showed that it was more likely that these measurements were insufficiently sensitive. Only four of the fallers were admitted with infections, and those subjects showed some temperature fluctuations. However, only 2 had temperatures above 37.5 degrees Celsius, which is consistent with the blunted fever response that is well known to occur in 50% of the elderly population 19,20 (and most fallers were elderly). The lack of value in respiratory rate recordings probably reflects the lack of due care and attention paid to this, the only manually measured parameter. It has long been recognized that respiratory rate recordings tend to be inaccurate 21 . The highly limited range of measurements recorded (16-22 breaths per minute) amongst all the fallers, despite some patients having severe pneumonia, further supports this finding. Finally, the PAR score tended to be quite static. This was a result of its constituent parameters not being sensitive (temperature, respiratory rate) and the fact that most of the heart rate and blood pressure recordings were within normal limits. LimitationsDespite the fact that this study was well powered and statistically significant, ultimately it is quite limited in numbers with just 13 patients. It was disappointing that we were not able to obtain case-notes or the appropriate file in the other 17. We are also presenting calculated data from the MAP measurements, without knowing the exact algorithms being used. For this reason, we analysed the given systolic pressures as further data manipulation would have increased inaccuracies. Our data is taken from relatively acute admissions and as such may not necessarily be applicable to long stay patients, where cardiovascular lability may not play an important role.Furthermore, controls were not matched for diagnosis or for the number of medications taken. This could lead to criticism that the comparison was poor, though the baseline measurements for the two were remarkably consistent. One of our aims was to see if variability could be used to accurately model general falls risk. We therefore thought it would be more useful to study the hospital’s general physiology, in all its varying degrees of illness. ConclusionsThis study shows the value of looking closely at patients’ observations and that even ‘normal’ values have to be interpreted in context . The data supports the finding that the risk of falling at a given point in time relates not only to predisposing factors, but also to their current cardiovascular status. We therefore suggest that a one-off falls risk assessment is no longer appropriate, but should be continuously reviewed on a shift-by-shift basis by nursing staff. This has significant ramifications for modernizing current risk stratification tools so that they are able take this into account.
|
Competing Interests None declared Author Details SIMON FREILICH, MBBS (Dist) BSc (Hons), Clinical Decision Unit, Barnet General Hospital, Barnet and Chase Farm NHS Trust, Enfield, UK ROBERT BARKER, MBBS MSc FRCP, Consultant Orthogeriatician, Clinical Decisions Unit, Barnet General Hospital, Barnet and Chase Farm NHS Trust, Enfield, UK CORRESPONDENCE: SIMON FREILICH, Clinical Decision Unit, Barnet General Hospital, Wellhouse Lane, Enfield, UK. EN5 3DJ Tel: 07730650918 Email: simonfreilich@googlemail.com |
References
1. Droller H. Falls among elderly people living at home. Geriatrics1955 May;10(5):239-44.
2. Healey F, Scobie S, Oliver D et al. Falls in English and Welsh hospitals: a national analysis of 12 months of patient safety incident observational study based on retrospective reports. Safety Health Care 2008;17;424-430.
3. Schwendimann R, Joos F, De Geest S et al. Are patient falls in the hospital associated with lunar cycles? A retrospective observational study. BMC Nursing 2005, 4:5 doi:10.1186/1472-6955-4-5
4. Oliver D, Britton M, Seed P et al. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies BMJ 1997;315:1049-1053.
5. The third report from the Patient Safety Observatory. Slips, trips and falls in hospital.
www.npsa.nhs.uk
6. Murray GR, Cameron ID, and Cumming RG. The Consequences of Falls in Acute and Subacute Hospitals in Australia That Cause Proximal Femoral Fractures. JAGS 55:577–582, 2007.
7. Corsinovi L, Bo M, Aimonino NR et al. Predictors of falls and hospitalization outcomes in elderly patients admitted to an acute geriatric unit. Arch Gerontol Geriatr (2008), doi:10.1016/j.archger.2008.06.004.
8. Vassallo M, Poynter L, Sharma JC et al. Fall risk-assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward. Age and Ageing 2008; 37: 277–281.
9. Downton JH. Falls in the Elderly. London, UK: Edward Arnold; 1993:64-80, 128-130
10. Healey F, Monro A, Cockram A et al. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age and Ageing 2004; 33: 390–395.
11. Heskestad B, Baardsen R, Helseth E et al. Incidence of hospital referred head injuries in Norway: A population based survey from the Stavanger region. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2009, 17:6.
12. van Hensbroek PB, van Dijk N, van Breda GF et al.on behalf of the Combined Amsterdam and Rotterdam Evaluation of FALLs (CAREFALL) study group. The CAREFALL Triage instrument identifying risk factors for recurrent falls in elderly patients. The American Journal of Emergency Medicine Volume 27, Issue 1, January 2009, Pages 23-36.
13. Ganz DA, Bao Y, Shekelle PG et al. Will my patient fall? J Fam Pract. 2007 Apr;56(4):276.
14. Costello E, Edelstein JE. Update on falls prevention for community-dwelling older adults: Review of single and multifactorial intervention programs. J Rehabil Res Dev. 2008;45(8):1135-52.
15. Hanlon JT, Boudreau RM, Roumani YF et al for the Health ABC study. Number and Dosage of Central Nervous System Medications on Recurrent Falls in Community Elders: The Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2009 Feb 4.
16. Redon J, Lurbe E. Nocturnal Blood Pressure Versus Nondipping Pattern What Do They Mean? Hypertension. 2008;51:41.
17. Marshall TP. Blood Pressure Variability: The Challenge of Variation
American Journal of Hypertension (2008) 21 3–4.
18. Verdecchia P, Schillaci G, Guerrieri M et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 1990;81;528-536
19. Roghmann MC, Warner J, Mackowiak PA. The relationship between age and fever magnitude. Am J Med Sci. 2001 Aug;322(2):68-70.
20. Norman DC. Fever in the elderly. Clin Infect Dis. 2000 Jul;31(1):148-51
21. Lovett PB, Buchwald JM, Stürmann K et al. The vexatious vital: Neither clinical measurements by nurses nor an electronic monitor provides accurate measurements of respiratory rate in triage. Annals of Emergency Medicine Volume 45, Issue 1, January 2005, Pages 68-76.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




