Post-Operative Urinary Retention in Elective Total Hip and Knee Replacement Surgery
Sumit Dutta
Cite this article as: BJMP 2008:1(2) 28-32
|
Introduction:
Post-operative urinary retention affects up to 38% of the 200,000 patients undergoing elective TKRs or THRs in the UK every year, according to literature.
Objectives:
This study aims to identify both patient and anaesthetic factors that predispose to urinary retention, and in doing so develop a protocol of pre-operative urinary catheterisations that will minimize its incidence and subsequent complications, as well as hasten patient recovery and discharge.
Methods:
Analysis of prospectively collected data of 54 patients over a three-month period at a British district general hospital.
Results:
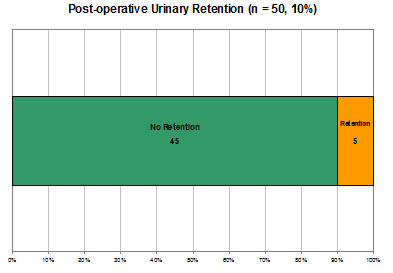
10% of patients in the study developed urinary retention, and 60% of these developed renal failure complicating recovery and lengthening stay. All were male, and a history of renal disease and a current elevated serum creatinine were identified as common factors in these patients.
Conclusions:
A protocol of pre-operatively catheterizing males with either a history of renal disease or a current elevated creatinine is suggested – this would potentially reduce incidence rates of urinary retention by 80% whilst only increasing the rate of unnecessary catheterizations by 2%.
Introduction:
Every year, approximately 200,000 people undergo elective total hip and knee replacement surgery in the UK 1. There is limited available literature on the incidence of post-operative urinary retention and even less regarding the onset of subsequent renal failure which, besides posing immediate medical problems, necessitates treatment and can significantly prolong recovery – all of which have personal and financial implications for both patient and healthcare trust.
Summary of Current Literature:
Surprisingly little research is available which offers data on the association on the incidence of, risk factors for, and associations with urinary retention for patients undergoing elective total hip or knee replacement surgery. The following table summarises seven studies conducted between 1980 and 2007:
| Study |
Year | n | Males | Females |
Retention |
Sepsis | ||
| TKR | THR | Overall | ||||||
| Wroblewski & Del Sel 2 | 1980 | 195 | 195 | 6.20% | ||||
| Waterhouse et al. 3 | 1987 | 103 | 103 | 0 | 10.70% | |||
| O' Riordan et al. 4 | 2000 | 116 | 47 | 69 | 18.10% | |||
| Kumar et al. 5 | 2004 | 19% | 22% | 0.93% | ||||
| Cronin et al. 6 | 2005 | 118 | 118 | 0 | 38.10% | |||
| Kumar et al. 7 | 2006 | 142 | 19.70% | 2.10% | ||||
| Lingaraj et al. 8 | 2007 | 119 | 10 | 109 | 10% | |||
Analysing the available literature, the following conclusions can be made.
- Males are more likely than females to develop urinary retention.
- Risk factors include a history of urinary retention, the use of epidural analgesia and patient-controlled analgesia (PCA).
- Retention rates varied between 10% and 38.1% (mean 19.6%).
- Deep sepsis rates varied between 0.93% and 2.1% in the total post-operative group, rising to 6.2% in those developing urinary retention.
Objectives:
This study aims to develop a policy of pre-operative catheterisation, anaesthetic technique and post-operative analgesia in patients undergoing elective total hip and knee replacement surgery that will:
- Minimize the incidence of urinary retention.
- Minimize the incidence of subsequent complications.
- Hasten patient recovery and discharge.
Methods:
A prospective study was conducted between February and April 2008 in the operating theatres and on the Orthopaedic wards at Bedford Hospital, a district general hospital in Bedfordshire, UK. Data was collected that would enable the following questions to be addressed:
- Are these patients catheterised pre-operatively?
- Of those who are not, how many develop urinary retention?
- Is any particular anaesthetic technique associated with an increased incidence of retention?
- Is antibiotic prophylaxis administered for catheterisation?
- How frequently does renal failure arise in those patients who develop urinary retention?
- Can a protocol be created which might reduce the incidence of retention?
- How effective and efficient would this be?
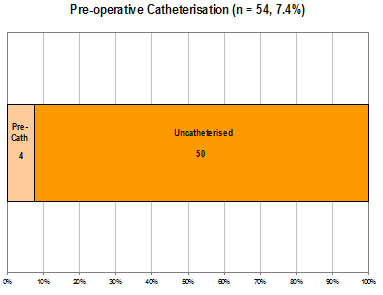
54 patients undergoing elective total hip and knee replacements were recruited into the study. Of these, 4 were catheterised pre-operatively and hence were excluded (n = 50).
Data Collection:
The primary source of data collection was from patients’ notes and anaesthetic charts, assessed pre- and post-operatively. Data was gathered in the following areas:
- Demographics – Name, Age, Sex
- ASA Classification – 1 to 4
- History of Renal disease
- History of Urological disease
- Pre-operative Creatinine
- Nature & Date of Operation
- Type of Anaesthetic Technique employed
- Onset of post-operative Urinary Retention necessitating catheterization
- Duration of Epidural Analgesia (if applicable)
- Administration of Antibiotic Prophylaxis for catheterization
- Progress from urinary retention to Renal Failure
Results:
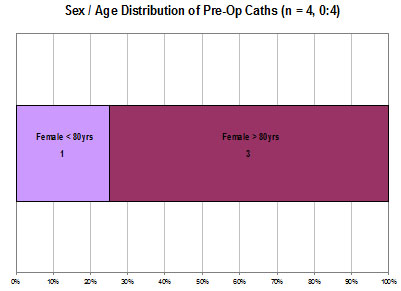
As mentioned, 4 of the original 54 patients were excluded from the study as they had already been catheterised pre-operatively. All were female, 75% of whom were over the age of 80; it appears that the main indication for pre-operatively catheterisation was existing urinary incontinence.
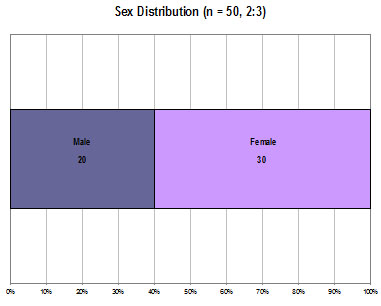
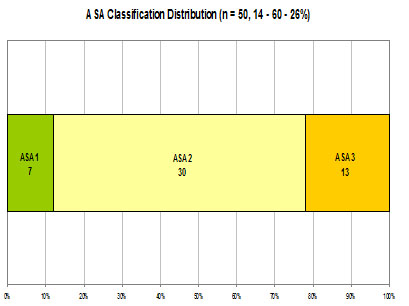
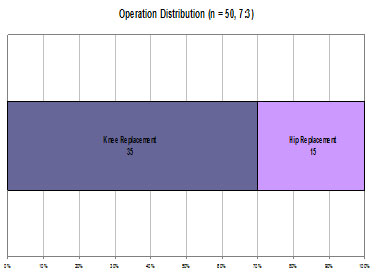
There was a female preponderance amongst the sample population, with females outnumbering males by a ratio of 3 to 2. In terms of the sample population’s co-morbidities and anaesthetic risk, the majority of patients were classified as ASA 2 (60%) by the assessing anaesthetist, with ASA 3 patients (26%) outnumbering ASA 1 patients (14%) by a ratio of approximately 2 to 1 in the remainder. Over the period covered, knee replacements (70%) outnumbered hip replacements (30%) by a ratio of 7 to 3.
A range of anaesthetic techniques were employed, including:
- Combined Spinal Epidural (CSE)
- Spinal Anaesthetic (Spinal)
- General Anaesthetic + Epidural (GA + Epidural)
- General + Spinal Anaesthetic (GA + Spinal)
- General Anaesthetic + Lumbar Plexus Block (GA + LPB)
- General Anaesthetic + Femoral Nerve Block (GA + FNB)
- General Anaesthetic +/- Patient Controlled Analgesia (GA + PCA)
Spinal anaesthetics appeared to be most commonly employed, either alone or in conjunction with a general anaesthetic. GAs in combination with a nerve block was also often used, followed by CSEs.
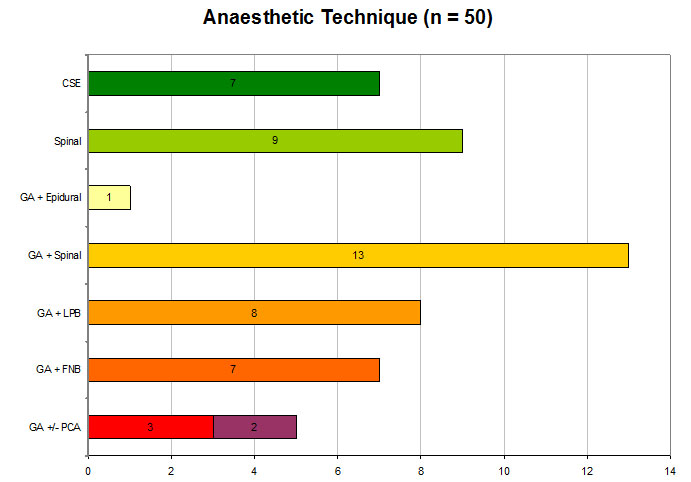
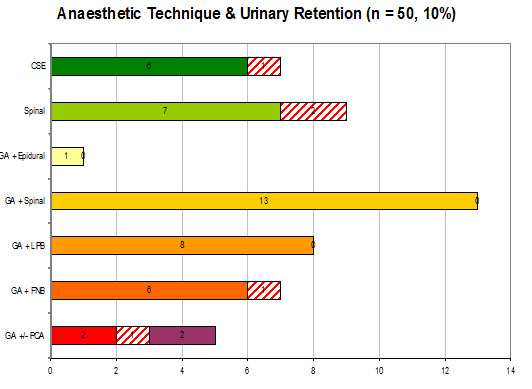
In total, there were a total of 5 cases of post-operative urinary retention, all of which necessitated catheterisation. This results in an incidence rate of 10% across elective total hip and knee replacements. Of these anaesthetic techniques, spinal anaesthesia was associated with the highest risk of post-operative urinary retention (22.2%), followed by GAs (20%), CSEs (14.3%) and GA + FNBs (14.3%). No cases were reported for patients who underwent GA + Spinals (n = 13), GA + LPBs (n = 8) or GA + Epidurals (n = 1).
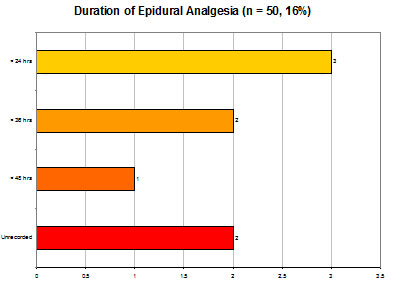
Of those patients who had undergone epidural anaesthesia, whether in combination either with a GA or a spinal, no documentation was found regarding the duration for which they had been active in 25% of cases. In the remainder, the epidural had been functional for less than 24 hours in 50% of cases.
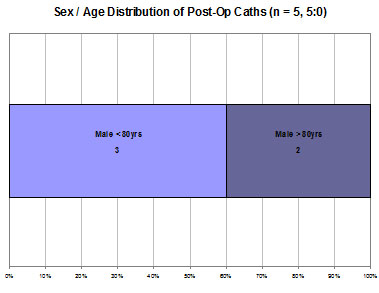
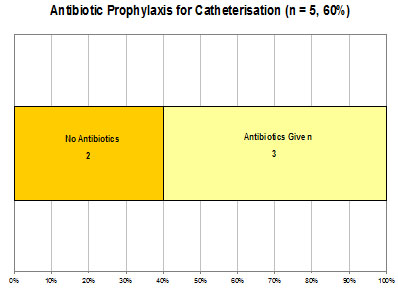
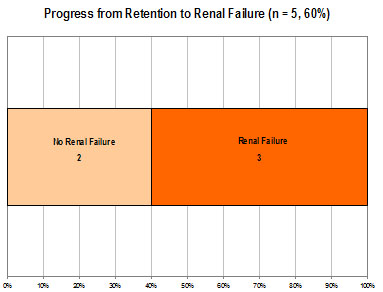
All five patients who developed post-operative urinary retention were male; three of whom were below the age of 80. Only three of these patients received the recommended antibiotic prophylaxis on catheterisation (60%), and on following up their subsequent inpatient progress and serum creatinine, it appeared the same number progressed to renal failure (60%).
Analysis:
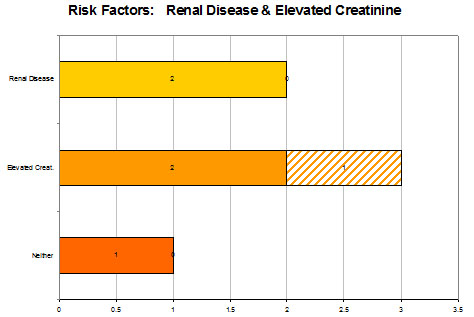
Two factors were identified in this study which may have predisposed these five patients into developing post-operative urinary retention. The first is a history of renal disease – 4% of the total sample had such a history (n = 2) and both went on to develop retention. The second is a currently elevated serum creatinine – 6% of the total sample had this at the time of surgery (n = 3), and of these, two went on the develop retention. The remaining patient who developed retention had neither of these risk factors.
The table below compares the results found in this study with those described in existing literature, namely the aforementioned publications. As can be seen, the post-operative urinary retention rate was on the lower extreme of that noted in the literature; only the studies by Waterhouse et al.3 and Lingaraj et al.7 demonstrated similar rates.
| Factor | Study | Literature |
| Pre-op Cath Rate | 7.4% | Unknown |
| Post-op Retention Rate | 10% | 10 - 38.1% |
| Hx of Renal Disease | Increased | Unknown |
| Elevated Creatinine | Increased | Unknown |
| Male Incidence | Increased | Increased |
| Epidural Incidence | Average | Increased |
This study concurred with the existing opinion that males have a higher incidence of retention, but the study population was insufficient to draw any specific conclusions regarding the influence of epidural anaesthesia on post-operative urinary retention. It was noted however, that in half of the cases for which data was available, the epidural was functional for less than 24 hours – one might argue that the risk/benefit ratio of epidural anaesthesia would cause it to be a relative contraindication if only employed for relatively short durations, particularly if the patient is admitted to a ward on which nursing staff are unfamiliar with its care.
Conclusions:
Existing literature fails to comment upon the impact of the aforementioned risk factors for retention highlighted in this study, namely a history of renal disease and a current elevated serum creatinine. However, these two factors in conjunction with the increased incidence in males allows for the creation of a system by which patients who are at high risk of developing post-operative urinary retention may be successfully identified and catheterised pre-operatively, hence preventing the problem from arising.
If a protocol had been established in which males with either of these two factors were catheterised pre-operatively, 5 patients from the sample population of 50 would have qualified; this includes 4 of the 5 patients who developed urinary retention post-operatively. In addition, only 1 patient who did not develop urinary retention post-operatively would have met these criteria and been unnecessarily catheterised pre-operatively. These figures are demonstrated in the graph below.
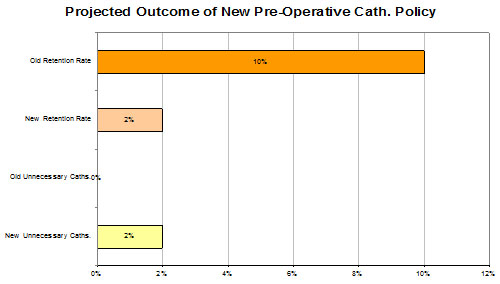
On the basis of these findings, one can deduce that a protocol indicating pre-operative catheterisation in males with either a history of renal disease and a current elevated serum creatinine undergoing total hip and knee replacement surgery would have a profound impact on the incidence of post-operative urinary retention, essentially reducing it by 80%. Unnecessary catheterisations as a result of this protocol would be minimal, affecting only 2% of patients.
Although this study has obvious limitations in terms of its size and its single-centred nature, findings were comparable to existing literature and are likely to be representative of incidence rates on a national, if not international basis. Further research, ideally with a larger population spread across multiple centres would allow for more accurate data to be collected, which in turn would allow for a more effective and efficient protocol to be developed.
COMPETING INTERESTS
None Declared
AUTHOR DETAILS
SUMIT DUTTA, MBBS, Speciality Trainee Registrar in Emergency Medicine, Bedford Hospital, United Kingdom
CORRESPONDENCE: Sumit Dutta, Specialty Trainee Registrar in Emergency Medicine, Bedford Hospital, Kempston Road, Bedford, MK429DJ, United Kingdom.
Tel: 01234 355122
References:
- Arthritis Research Campaign; www.arc.org.uk
- Wroblewski BM, del Sel HJ. Urethral instrumentation and deep sepsis in total hip replacement. Clinical Orthopaedic and Related Research. 1980 Jan-Feb; (146): 209-12
- Waterhouse N, Beaumont AR, Murray K, Staniforth P, Stone MH. Urinary Retention after Total Hip Replacement. A Prospective Study. Journal of Bone and Joint Surgery, British Volume. 1987 Jan; 69 (1): 64-6
- O’Riordan JA, Hopkins PM, Ravenscroft A, Stevens JD. Patient controlled analgesia and urinary retention following lower limb joint replacement: prospective audit and logistic regression analysis. European Journal of Anaesthesiology. 2000 Jul; 17 (7): 431-5
- Kumar P, Mannan K, Chowdhury AM, Kong KC, Pati J. Urinary retention following arthroplasty. Urology, 2005 Sep; 66(3); Supp I: 22
- Cronin JJ, Shannon FJ, Bale E, Quinlan W. Prediction of post-operative urinary retention following hip and knee arthroplasty in a male population. European Journal of Orthopaedic Surgery and Traumatology. 2007 Jan; (17): 47-50
- Kumar P, Mannan K, Chowdhury AM, Kong KC, Pati J. Urinary retention and the role of indwelling catheterization following total knee arthroplasty. International Brazilian Journal of Urology 2006 Jan-Feb; (32): 1
- Lingaraj K, Ruben M, Chan YH, De Das S. Identification of risk factors for urinary retention following total knee arthroplasty: a Singapore hospital experience. Singapore Medical Journal. 2007 Mar; 48 (3): 213-6

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




