Management of Drooling of saliva
Ganesh Bavikatte, Poh Lin Sit and Ali Hassoon
Cite this article as: BJMP 2012;5(1):a507
|
|
Abstract Drooling, also known as ptyalism or sialorrhea can be defined as salivary incontinence or the involuntary spillage of saliva over the lower lip. Drooling could be caused by excessive production of saliva, inability to retain saliva within the mouth, or problems with swallowing. Drooling can lead to functional and clinical consequences for patients, families, and caregivers. Physical and psychosocial complication includes maceration of skin around the mouth, secondary bacterial infection, bad odour, dehydration and social stigmatisation. People with drooling problems are also at increased risk of inhaling saliva, food, or fluids into the lungs especially when body's normal reflex mechanisms, such as gagging and coughing are also impaired. Successful management of sialorrhea can alleviate the associated hygienic problems, improve appearance, enhance self-esteem, and significantly reduce the nursing care time of these sufferers.Chronic drooling can be difficult to manage; this article gives overview of the causes, effects and management of drooling of saliva in general practice. |
Saliva is the watery and usually frothy substance produced in and secreted from the three paired major salivary (parotid, submandibular and sublingual) glands and several hundred minor salivary glands, composed mostly of water, but also includes electrolytes, mucus, antibacterial compounds, and various enzymes. Healthy persons are estimated to produce 0.75 to 1.5 liters of saliva per day. At least 90% of the daily salivary production comes from the major salivary glands while the minor salivary glands produce about 10%. On stimulation (olfactory, tactile or gustatory), salivary flow increases five fold, with the parotid glands providing the preponderance of saliva.1
Saliva is a major protector of the tissues and organs of the mouth. In its absence both the hard and soft tissues of the oral cavity may be severely damaged, with an increase in ulceration, infections, such as candidiasis, and dental decay. Saliva is composed of serous part (alpha amylase) and a mucus component, which acts as a lubricant. It is saturated with calcium and phosphate and is necessary for maintaining healthy teeth. The bicarbonate content of saliva enables it to buffer and produce the condition necessary for the digestion of plaque which holds acids in contact with the teeth. Moreover, saliva helps with bolus formation and lubricates the throat for the easy passage of food. The organic and inorganic components of salivary secretion have got a protective potential. They act as barrier to irritants and a means of removing cellular and bacterial debris. Saliva contains various components involved in defence against bacterial and viral invasion, including mucins, lipids, secretory immunoglobulins, lysozymes, lactoferrin, salivary peroxidise, and myeloperoxidase. Salivary pH is about 6-7, favouring digestive action of salivary enzyme, alpha amylase, devoted to starch digestion.
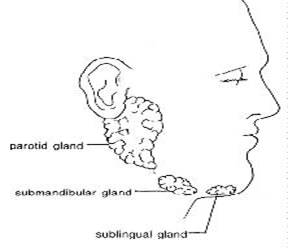
Image -1. (Source of this image- http://www.entdoctor.co.nz)
Salivary glands are innervated by the parasympathetic and sympathetic nervous system. Parasympathetic postganglionic cholinergic nerve fibers supply cells of both the secretory end-piece and ducts and stimulate the rate of salivary secretion, inducing the formation of large amounts of a low-protein, serous saliva. Sympathetic stimulation promotes saliva flow through muscle contractions at salivary ducts. In this regard both parasympathetic and sympathetic stimuli result in an increase in salivary gland secretions. The sympathetic nervous system also affects salivary gland secretions indirectly by innervating the blood vessels that supply the glands.
Table 1: Functions of saliva
| Digestion and swallowing Initial process of food digestion Lubrication of mouth, teeth, tongue and food boluses Tasting food Amylase- digestion of starch Disinfectant and protective role Effective cleaning agent Oral homeostasis Protect teeth decay, dental health and oral odour Bacteriostatic and bacteriocidal properties Regulate oral pH Speaking Lubricates tongue and oral cavity |
Drooling (also known as driveling, ptyalism, sialorrhea, or slobbering) is when saliva flows outside the mouth, defined as “saliva beyond the margin of the lip”. This condition is normal in infants but usually stops by 15 to 18 months of age. Sialorrhea after four years of age generally is considered to be pathologic. The prevalence of drooling of saliva in the chronic neurological patients is high, with impairment of social integration and difficulties to perform oral motor activities during eating and speech, with repercussion in quality of lifeDrooling occurs in about one in two patients affected with motor neuron disease and one in five needs continuous saliva elimination7, its prevalence is about 70% in Parkinson disease8, and between 10 to 80% in patients with cerebral palsy9.
Pathophysiology
Pathophysiology of drooling is multifactorial. It is generally caused by conditions resulting in
- Excess production of saliva- due to local or systemic causes (table 2)
- Inability to retain saliva within the mouth- poor head control, constant open mouth, poor lip control, disorganized tongue mobility, decreased tactile sensation, macroglossia, dental malocclusion, nasal obstruction.
- Problems with swallowing- resulting in excess pooling of saliva in the anterior portion of the oral cavity e.g. lack of awareness of the build-up of saliva in the mouth, infrequent swallowing, and inefficient swallowing.
Drooling is mainly due to neurological disturbance and less frequently to hyper salivation.Under normal circumstances, persons are able to compensate for increased salivation by swallowing. However, sensory dysfunction may decrease a person’s ability to recognize drooling and anatomic or motor dysfunction of swallowing may impede the ability to manage increased secretion.
Table 2 Aetiology of hypersalivation
| Physiological Pregnancy Local causes Oral inflammation- teething Infection –oral cavity infection, dental caries, tonsillitis, peritonsilar abscess Systemic Toxin exposure- pesticides, mercury, capsaicin, snake poisoning Medication –tranquilizers, anticonvulsants, anticholinesterases, lithium Neuromuscular –cerebral palsy, Parkinson’s disease, motor neuron disease, bulbar/ pseudobulbar palsy, Stroke Infection- rabies Gastric- gastroesophageal reflux |
Depending on duration of drooling, it can be classified as acute e.g. during infections (epiglottitis, peritonsilar abscess) or chronicneurological causes.
Symptoms
Drooling of saliva can affect patient and/or their carers quality of life and it is important to assess the rate and severity of symptoms and its impact on their life.
Table 3 Effect of untreated Drooling of saliva
| Physical | Psychological |
| Perioral chapping (skin cracking) Maceration with secondary infection Dehydration Foul odour Aspiration/ pneumonia Speech disturbance Interference with feeding |
Isolation Barriers to education (damage to books or electronic devices) Increased dependency and level/intensity of care Damage to electronic devices Decreased self esteem Difficult social interaction |
Assessment
Assessment of the severity of drooling and its impact on quality of life for the patient and their carers help to establish a prognosis and to decide the therapeutic regimen. A variety of subjective and objective methods for assessment of sialorrhoea have been described3.
History (from patient and carers)
Establish possible cause, severity, complications and possibility of improvement, age and mental status of patient, chronicity of problems, associated neurological conditions, timing, provoking factors, estimation of quantity of saliva – use of bibs, clothing changing required/ day and impact on the day today life (patient/carer)
Physical examination
Evaluate level of alertness, emotional state, hydration status, hunger, head posture
Examination of oral cavity- sores on the lip or chin, dental problems, tongue control, swallowing ability, nasal airway obstruction, decreased intraoral sensitivity, assessment of health status of teeth, gum, oral mucosa, tonsils, anatomical closure of oral cavity, tongue size and movement, jaw stability. Assessment of swallowing
Assess severity and frequency of drooling (as per table 4)
Investigation
- Lateral neck x ray (in peritonsilar abscess)
- Ultrasound to diagnose local abscess
- Barium swallow to diagnose swallowing difficulties
- Audiogram- to rule out conductive deafness associated with oropharyngeal conditions
- Salivary gland scan- to determine functional status
Table 4 : System for assessment of frequency and severity of drooling
| Drooling severity | Points |
| Dry (never drools) | 1 |
| Mild (wet lips only) | 2 |
| Moderate (wet lips and chins) | 3 |
| Severe (clothing becomes damp) | 4 |
| Profuse (clothing, hands, tray, object become wet) | 5 |
| Frequency | Points |
| Never drools | 1 |
| Occasionally drools | 2 |
| Frequency drools | 3 |
| Constantly drools | 4 |
| Other methods of assessing salivary production and drooling 1) 1- 10 visual analogue scale (where 1 is best possible and 10 is worst possible situation) 2) Counting number of standard sized paper handkerchiefs used during the day 3) Measure saliva collected in cups strapped to chin 4) Inserting pieces of gauze with a known weight into oral cavity for a specific period of time and then re-measuring weight and calculating the difference between the dry and wet weights. 5) Salivary gland scintigraphy / technetium scanning 6) Salivary duct canulation 12 and measuring saliva production. |
|
Management
Drooling of saliva, a challenging condition, is better managed with a multidisciplinary team approach. The team includes primary care physician, speech therapist, occupational therapist, dentist, orthodontist, otolaryngologist, paediatrician and neurologist. After initial assessment, a management plan can be made with the patient. The person/ carer should understand the goal of treating drooling is a reduction in excessive salivary flow, while maintaining a moist and healthy oral cavity. Avoidance of xerostomia (dry mouth) is important.
There are two main approaches
- Non invasive modalities e.g. oral motor therapy, pharmacological therapy
- Invasive modalities e.g. surgery and radiotherapy
No single approach is totally effective and treatment is usually a combination of these techniques. The first step in management of drooling is correction of reversible causes. Less invasive and reversible methods, namely oral motor therapy and medication are usually implemented before surgery is undertaken5
Non invasive modalities
Positioningprior to implementation of any therapy, it is essential to look at the position of the patient. When seated, a person should be fully supported and comfortable. Good posture with proper trunk and head control provides the basis for improving oral control of drooling and swallowing.
Eating and drinking skills-drooling can be exacerbated by pooreating skills. Special attention and developing better techniques in lip closure, tongue movement and swallowing may lead to improvements of some extent. Acidic fruits and alcohol stimulate further saliva production, so avoiding them will help to control drooling10
Oral facial facilitation - this technique will help to improve oral motor control, sensory awareness and frequency of swallowing.Scott and staios et al 18 noted improvement in drooling in patients with both hyper and hypo tonic muscles using this technique. This includes different techniques normally undertaken by speech therapist, which improves muscle tone and saliva control. Most studies show short term benefit with little benefit in long run. This technique can be practiced easily, with no side effects and can be ceased if no benefits noted.
a) Icing – effect usually last up to 5-30 minutes. Improves tone, swallow reflex.
b) Brushing- as effect can be seen up to 20- 30 minutes, suggested to undertake before meals.
c) Vibration- improves tone in high tone muscles
d) Manipulation – like tapping, stroking, patting, firm pressure directly to muscles using fingertips known to improve oral awareness.
e) Oral motor sensory exercise - includes lip and tongue exercises.
Speech therapy-speech therapy should be started early to obtain good results. The goal is to improve jaw stability and closure, to increase tongue mobility, strength and positioning, to improve lip closure (especially during swallowing) and to decrease nasal regurgitation during swallowing.
Behaviour therapy-this uses a combination of cueing, overcorrection, and positive and negative reinforcement to help drooling. Suggested behaviours, like swallowing and mouth wiping are encouraged, whereas open mouth and thumb sucking are discouraged. Behavior modification is useful to achieve (1) increased awareness of the mouth and its functions, (2) increased frequency of swallowing, (3) increased swallowing skills. This can be done by family members and friends. Although there is no randomized controlled trial done, over 17 articles published in last 25 years, show promising results and improved quality of life. No reported side effects make behavioural interventions an initial option compared to surgery, botulinum toxin or pharmaceutical management. Behaviour interventions are useful prior and after medical management such as botulinum toxin or surgery.
Oral prosthetic device- variety of prosthetic devices can be beneficial, e.g. chin cup and dental appliances, to achieve mandibular stability, better lip closure, tongue position and swallowing. Cooperation and comfort of the patient is essential for better results.
Pharmacological methods
Systematic review of anticholinergic drugs, show Benztropine, Glycopyrrolate, and Benzhexol Hydrochloride, as being effective in the treatment of drooling. But these drugs have adverse side-effects and none of the drugs been identified as superior.
Hyoscine- The effect of oral anticholinergic drugs has been limited in the treatment of drooling. Transdermal scopolamine (1.5 mg/2.5 cm2) offers advantages. One single application is considered to render a stable serum concentration for 3 days. Transdermal scopolamine has been shown to be very useful in the management of drooling, particularly in patients with neurological or neuropsychiatric disturbances or severe developmental disordersIt releases scopolamine through the skin into the bloodstream.
Glycopyrrolatestudies have shown 70-90% response rates but with a high side effect rate. Approximately 30-35% of patients choose to discontinue due to unacceptable side effects such as excessive dry mouth, urinary retention, decreased sweating, skin flushing, irritability and behavior changes. A study on 38 patients with drooling due to neurological deficits had shown up to a 90% response rateMier et al21 reported Glycopyrrolate to be effective in the control of excessive sialorrhea in children with developmental disabilities. Approximately 20% of children given glycopyrrolate may experience substantial adverse effects, enough to require discontinuation of medication.
Antimuscarinic drugs, such as benzhexol, have also been used, but limited due to their troublesome side effects.
Antireflux Medication: The role of antireflux medication (Ranitidine & Cisapride) in patients with gastro esophageal reflux due to esophageal dysmotility and lower esophageal tone did not show any benefits in a study 21.
Modafinil - One case study noticed decreased drooling in two clients who were using the drug for other reasons, but no further studies have been done.
Alternate medications: (Papaya and Grape seed extract) – Mentioned in literature as being used to dry secretions but no research in to their efficacy has been conducted.
Botulinum toxin It was in 1822 that a German poet and physician, Justinus Kerner, discovered that patients who suffered from botulism complained of severe dryness of mouth which suggested that the toxin causing botulism could be used to treat hypersalivation. However, it was only in the past few years that botulinum toxin type A (BTx-A)has been used for this purpose. BTx-A binds selectively to cholinergic nerve terminals and rapidly attaches to acceptor molecules at the presynaptic nerve surface. This inhibits release of acetylcholine from vesicles, resulting in reduced function of parasympathetic controlled exocrine glands. The blockade though reversible is temporary as new nerve terminals sprout to create new neural connections. Studies have shown that injection of botulinum toxin to parotid and submandibular glands, successfully subsided the symptoms of drooling 30,31. Although there is wide variation in recommended dosage, most studies suggest that about 30- 40 units of BTx-A injected into the parotid and submandibular glands are enough for the symptoms to subside The injection is usually given under ultrasound guidance to avoid damage to underlying vasculature/ nerves. The main side effects from this form of treatment are dysphagia, due to diffusion into nearby bulbar muscles, weak mastication, parotid gland infection, damage to the facial nerve/artery and dental caries.
Patients with neurological disorders who received BTX-A injections showed a statistically significant effect from BTX-A at 1 month post injection, compared with control, this significance was maintained at 6 months. Intrasalivary gland BTX-A was shown to have a greater effect than scopolamine.
The effects of BTx-A are time limited and this varies between individuals.
Invasive modalities
Surgerycan be performed to remove salivary glands, (most surgical procedures focused on parotid and submandibular glands). ligate or reroute salivary gland ducts, or interrupt parasympathetic nerve supply to glands. Wilke, a Canadian plastic surgeon, was the first to propose and carry out parotid duct relocation to the tonsillar fossae to manage drooling in patients with cerebral palsy. One of the best studied procedures, with a large number of patients and long term follow up data, is submandibular duct relocation 32, 33.
Intraductal laser photocoagulation of the bilateral parotid ducts has been developed as a less invasive means of surgical therapy. Early reports have shown some impressive results34.
Overall surgery reducedsalivary flow and drooling can be significantly improved often with immediate results – 3 studies noted that 80 – 89% of participants had an improvement in their control of their saliva. Two studies discussed changes in quality of life. One of these found that 80% of those who participated improved across a number of different measures including receiving affection from others and opportunities for communication and interaction. Most evidence regarding surgical outcomesof sialorrhea management is low quality and heterogeneous. Despitethis, most patients experience a subjective improvement followingsurgical treatment 36.
Radiotherapy - to major salivary glands in doses of 6000 rad or more is effective Side effects which include xerostomia, mucositis, dental caries, osteoradionecrosis, may limit its use.

Key messages
|
|
Competing Interests None declared Author Details Ganesh Bavikatte, MBBS, MD (Medicine), MRCP(UK), MRCP(London), Speciality Registrar Rehabilitation Medicine, Manchester, UK. Poh Lin Sit, MBBch, Staff Grade in Rehabilitation Medicine, Central Manchester University Hospitals, Manchester, UK. Ali Hassoon, MB ChB, FRCP (London), Consultant Physician Rehabilitation Medicine, Central Manchester NHS Trust, Manchester, UK. CORRESPONDENCE: Ganesh Bavikatte, MBBS, MD (Medicine), MRCP(UK), MRCP(London, Speciality Registrar Rehabilitation Medicine, 9 averhill, worsley, Manchester, M281ZN. Email: ganeshbavikatte@ukdoctor.org |
References
1. Stuchell RN, Mandel ID. Salivary gland dysfunction and swallowing disorders. Otolayngol Clin North Am 1988;21:649-61.2. Costanzo, L. Text book of Physiology, 3rd edition. Saunders Elsevier. ISBN 10:1-4160-2320-8.3. Sochaniwskyj AE. Drool Quantification: noninvasive technique. Arch Phys Med Rehabil 1982;63:605-74. Neil G. Hockstein, Daniel S. Samadi, Kristin Gendron, Steven D. Handler, Am Fam Physician 2004;69:2628-345. Louise Cummings, Text book of Clinical Linguistics, edin univ press, page 95-99, 2008 6. Hilary Johnson, Amanda Scott, Text book on A practical approach to saliva control page31, 86.7. Giles R, Naummann M, Werner E, Riemann M, Beck I, Puls I, Reinners C, Toyka KV. Injection of botulinum toxin A in to salivary glands improve sialorrhoea in amyotropic lateral sclerosis. J Neurol Neurosurg Psychiatry 200;69:121-38. Jongerius PH, Rotteveel JJ, Van Limbeck J, Gabreels FJM, Van Ilulst KBS, Van Den Ilogen FJA. Botulinum toxin effect on salivary flow rate in children with cerebral palsy. Neurology 2004;63:1371-59. Boothwell JE, Clarke K, Dooley JM, Gordon KE, Anderson R, Wood Camfied CS, Camfield PR. Botulinum toxin A as a treatment for excessive drooling in children. Paediatr Neurology 2002; 27(1):18-2210. Johnson H, Scott A. 1993; Book on practical approach to saliva control and communication; 199311. Scully C, Limeres J, Gleeson M, Tomás I, Diz P. Drooling, J Oral Pathol Med. 2009 Apr;38(4):321-7. Epub 2009 Feb 23.12. Suskind DL, Tilton A. Clinical study of botulinum toxin- A in the treatment of sialorrhoea in children with cerebral palsy. Laryngoscope 2002. 112:73-81.13. Crysdale WS, McCann C, Roske L. Saliva control issues in the neurologically challenged: a 30 year experience in team management. Int J Paedatr Otolarynol: 2006; 70: 519-52714. Sullivan PB, Lambert B, Rose M. Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding study. Dev Med Child Neuol 2000;42:674-68015. Meningaud JP, Pitak-Arnnop P, Chikhani L, Bertrand JC. Drooling of saliva: A Review of the etiology and management options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(1):48-57.16. Hockstein NG, Samadi DS, Gendron K, Handler SD, Sialorrhoea: a management Challenge, Am Fam Physician 2004; 69:2628-2634.17. Jongerius PH, Van Tiel P, Van Limbeek J, A systematic review for evidence of efficacy of anticholinergic drugs to treat drooling. Arch Dis Child 2003; 88: 911-91418. Scott, A., & Staios, G. (1993). Oral-facial facilitation. In J. Hilary & A. Scott (Eds.), A practical approach to saliva control (pp. 32-42). San Antonio, TX: Communication Skill Builders.19. Potulska A, Friedman A. Controlling sialorrhoea: a review of available treatment options. Expert Opin Pharmacother. 2005 Aug;6(9):1551-4.20. Mato Montero A, Limeres Posse J, Tomás Carmona I, Fernández Feijoo J, Diz Dios P.Med Oral Patol Oral Cir Bucal. 2008 Jan 1;13(1):E27-30.21. Mier RJ, Bachrach SJ, Lakin RC, Barker T, Childs J, Moran M. Treatment of sialorrhea with glycopyrrolate: A double-blind, dose-ranging study. Arch Pediatr Adolesc Med. 2000 Dec;154(12):1214-8.22. Blasco P.A. Glycopyrrolate treatment of chronic drooling. Archives of paediatric adolescent medicine, vol 150, sept 1996:932-935. 23. Heine R.G. Effect of antireflux medication on salivary drooling in children with cerebral palsy. Developmental medicine and child neurology, 1996, vol 38, 1030-36.24. Blasco P.A. (2002) Management of drooling: 10 years after the consortium on drooling, 1990. Dev. Med. Child Neurol. 44, 778–78125. Camp-Bruno J.A., Winsberg B.G., Green-Parsons A.R. (1989) Efficacy of benztropine therapy for drooling. Dev. Med. Child Neurol. 31, 309–31926. Lloyd Faulconbridge R.V., Tranter R.M., Moffat V. Review of management of drooling problems in neurologically impaired children: A review of methods and results over 6 years at Chailey Heritage clinical services. Clin. Otolaryngol. Allied Sci. (2001) 26, 76–8127. Porta M., Gamba M., Bertacchi G. et al. (2001) Treatment of sialorrhoea with ultrasound guided botulinum toxin type A injection in patients with neurological disorders. J. Neurol. Neurosurg. Psychiatry 70, 538–54028. Jongerius P.H., van den Hoogen F.J., van Limbeek J. et al. (2004) Effect of botulinum toxin in the treatment of drooling: A controlled clinical trial. Pediatrics 114, 620–62729. Diamant H, Kumlien A. A treatment for drooling in children with cerebral palsy. J Laryngol Otol. 1974;88(1):61-64.30. Peter Misra. Botulinum toxin as a treatment for drooling of saliva. ACNR; nov/dec 2002: v2 n2 11-12.31. Dayse Manrique, application of botulinum toxin to reduce the saliva in patients with amyotropic lateral sclerosis; Rev Bras Otorrinolaringol; sept-oct 2005, v.71, n.5, 566-6932. Borg M, Hirst, the role of radiation therapy in the management of sialorrhea international journal of radiation oncology, biology and physics; 1998 jul: 1113-933. Crysdale W.S. Management of drooling in individuals with neurodisability: a surgical experience. Developmental medicine and child neurology. 2001(43) 379- 383.34. O’Dwyer T.P. the surgical management of drooling- a 15 year follow up. Clinical Otolaryngology. 1997(22) 284-287.35. Chang C. Intraductal laser photocoagulation of the bilateral parotid ducts for reduction of drooling in patients with cerebral palsy. Plastic and reconstructive Surgery. 2001(107) 907- 913.36. Jeremy Reed, MD, MPH; Carolyn K. Mans, MD; Scott E. Brietzke, MD, MPH Surgical Management of Drooling A Meta-analysis. Arch Otolaryngol Head Neck Surg. 2009;135(9):924-931.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




