Lypmhoplasmacyte rich meningioma-a rare morphological variant of meningioma
Manveen Kaur, Varsha Dalal, Karam Chand Sharma, Avninder Singh
Cite this article as: BJMP 2016;9(1):a905
|
|
Abstract Lymphoplasmacyte-rich meningioma (LPM) is a rare variant of meningioma accounting for less than 1% of all meningiomas. It is characterized by extensive infiltrate of lymphocytes and plasma cells often obscuring the meningothelial component. We report a case of a 21-year-old male who presented with a solid cystic lesion in the right fronto-parietal region. Histopathological and immunohistochemical examination finally helped in reaching the diagnosis of lymphoplasmacyte-rich meningioma. Recognition of this entity is of paramount importance to guide appropriate therapy and management. Keywords: lymphoplasmacyte, meningioma, intracranialAbbreviations: LPM- Lymphoplasmacyte- rich meningioma; WHO- World Health Organisation; IHP- idiopathic hypertrophic pachymeningitis; EMA- Epithelial membrane antigen |
Introduction
Meningiomas are common intracranial neoplasms with a wide range of histopathological appearances. The WHO classification of tumours of the central nervous system recognises 15 subtypes of meningiomas, of which meningothelial, fibrous and transitional subtypes are most common. Lymphoplasmacyte-rich meningiomas (LPM) are rare WHO subtype that belong to Grade I meningiomas.1 The estimated incidence is less than 1% of all meningiomas.2 LPM usually occurs in young and middle age patients, with most common locations being cerebral convexities, skull base, parasagittal area within the superior sagittal sinus, cervical canal, optic nerve and tentorium.3 Histopathological examination shows extensive infiltrates of lymphocytes and plasma cells often obscuring the meningothelial component.
Case report
A 21-year-old man presented with a history of headache since 4 months. It was a dull pain not associated with vomiting, seizures or visual symptoms. The patient did not have any features suggestive of cranial nerve involvement. Physical examination was unremarkable except for the presence of papilloedema. Non-contrast CT scan showed a large isodense lesion with peri- lesional oedema and eccentric enhancing nodular component in the right fronto-parietal region (Figure 1). A radiological diagnosis of glioma with mass effect and shift to left was rendered. A right frontoparietal free bone flap craniotomy was performed. Operatively, a well encapsulated tumour probably arising from the dura mater was found. Gross total removal of the tumour was done and the excised tumour was sent for histopathological examination with a provisional clinical diagnosis of meningioma.
Histopathological examination revealed a tumour arranged as sheets and whorls of meningothelial cells without any mitoses or atypia. A dense infiltrate of lymphocytes and plasma cells was seen in large areas of the tumour (Figure 2).
On immunohistochemistry, tumour cells were positive for epithelial membrane antigen (EMA) (Figure 3) and vimentin. The lymphoplasmacytic infiltrate contained mixture of CD3 and CD20 positive lymphocytes. A diagnosis of lymphoplasmacyte- rich meningioma was given.
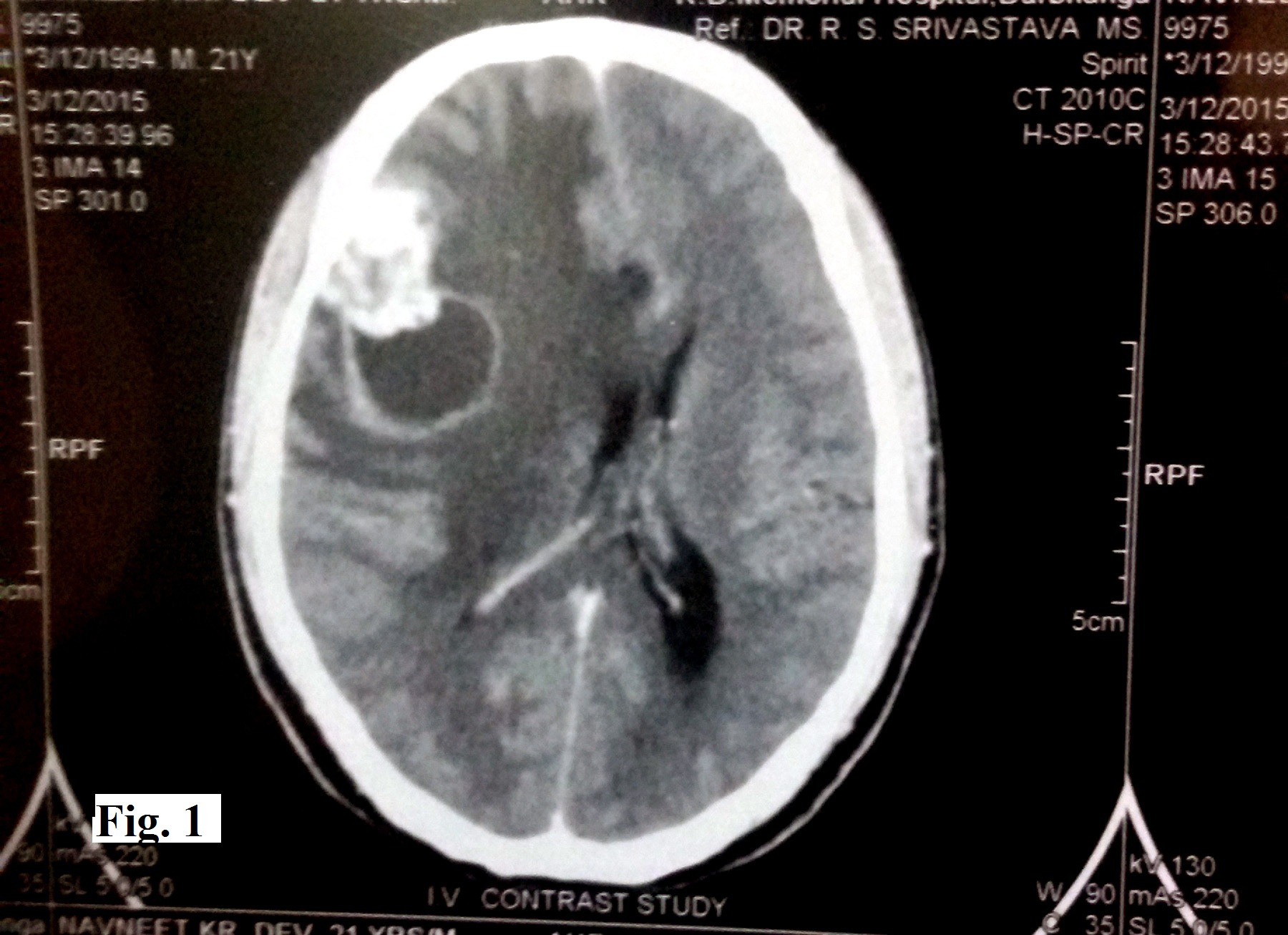
Figure 1. Non-contrast CT scan showing a large isodense cystic lesion with perilesional oedema and eccentric enhancing nodular component in the right frontoparietal region
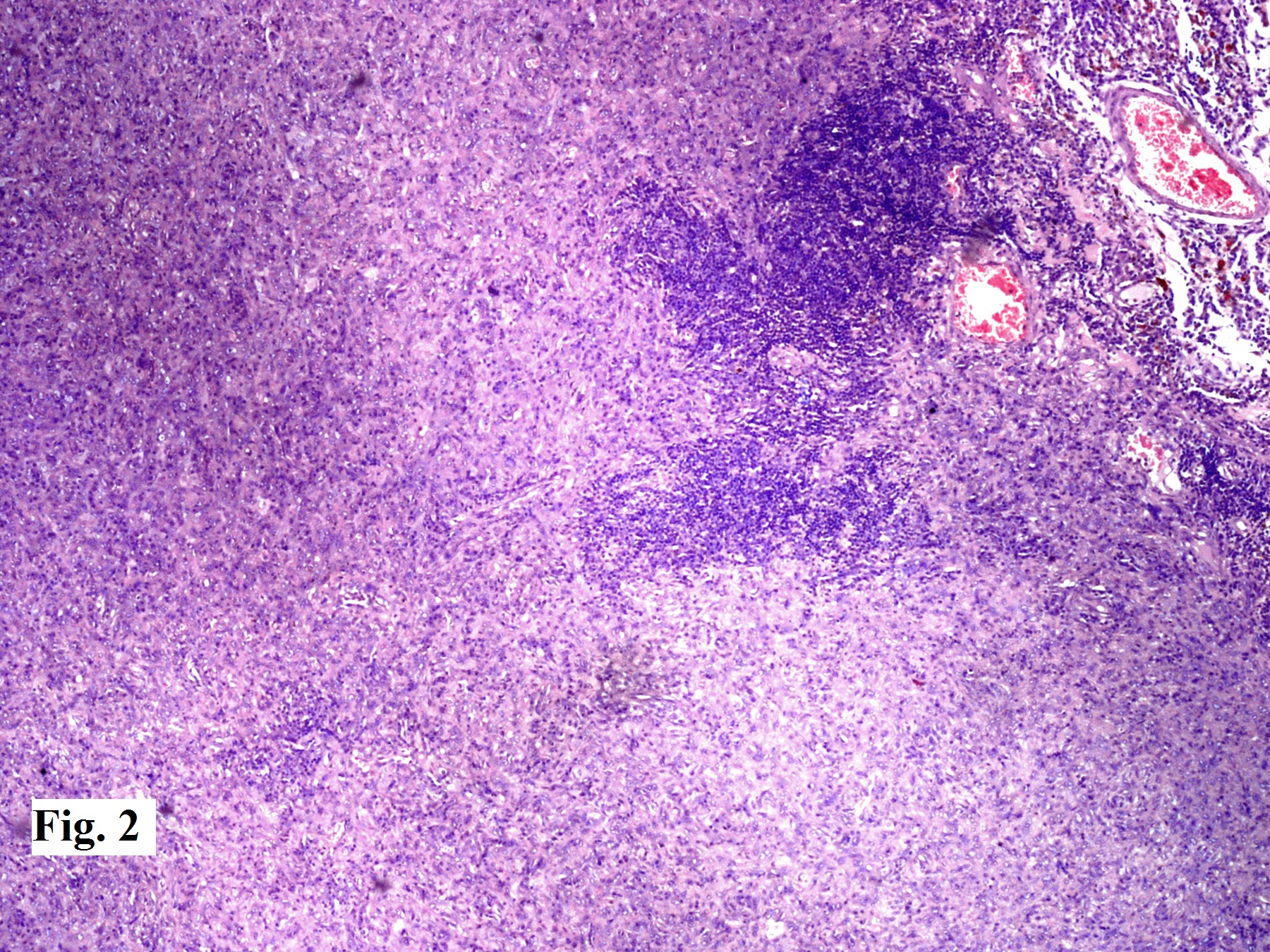
Figure 2: Tumour arranged as sheets and whorls of meningothelial cells without any mitoses or atypia. A dense infiltrate of lymphocytes and plasma cells seen in large areas of the tumour (H & E x 100)
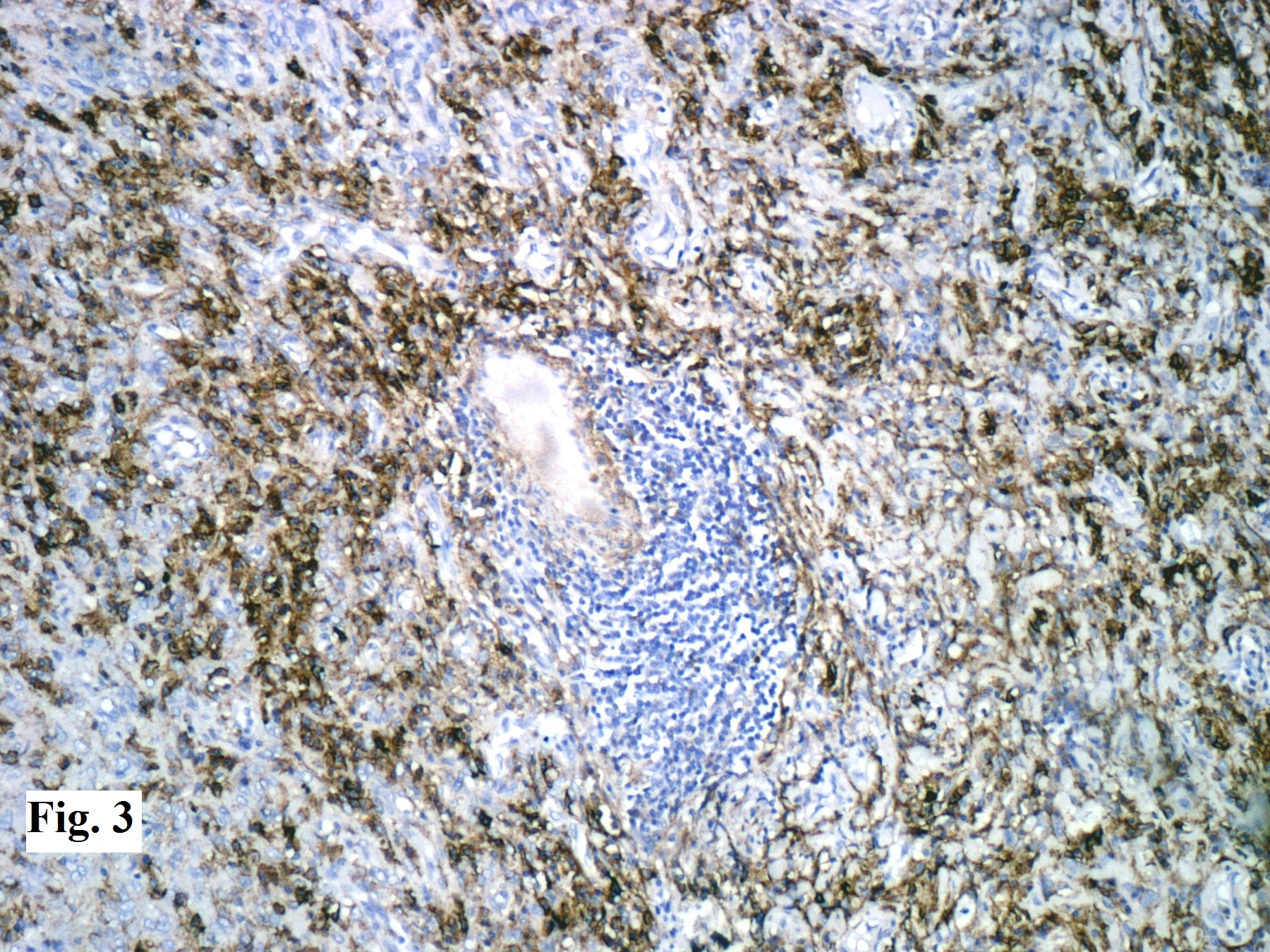
Figure 3: Tumour cells positive for epithelial membrane antigen (x 200)
Discussion
Meningiomas are common neoplasms accounting for 24-30% of all primary intracranial tumours. They arise from the arachnoidal cells, and are typically attached to the inner surface of the duramater.1 Most of the meningiomas are benign, corresponding to WHO grade I and associated with a favourable clinical outcome. LPM is a rare low grade histopathological subtype of meningioma, usually seen in younger patients, with the mean age of onset being 34 years.4,5 The patients with LPM have variable clinical manifestations according to the location of the tumour. The common presentations include headache, hemiparesis, seizure, vomiting, dizziness, visual disturbance, dyscalculia, dysgraphia and slurred speech.3 Although the natural history of LPM is often over one year, few cases might occur in short duration due to inflammatory cell infiltration and oedema.6 Systemic haematological abnormalities such as hyperglobulinemia and iron refractory anaemia have been documented in some patients with LPM, believed by some to be due to the plasma cell infiltrate.3,6,7
Radiologically, LPMs are usually globular, highly vascular, contrast- enhancing, and dural based tumours. The typical characters of LPM on MRI are isointense lesions on T1-weighted images and hyperintense lesions on T2-weighted images, with a strong homogenous enhancement after the administration of gadolinium; obvious peritumoural brain oedema and dural tail signs.3 Sometimes, cystic component and heterogeneous enhancement may also be encountered, making pre-operative diagnosis difficult, as in our case.8
On microscopic examination, this tumour is characterised by a conspicuous infiltrate of lymphocytes and plasma cells, sometimes completely obscuring the tumour cells. The massive infiltration of lymphocytes and plasma cells has been postulated to play a central role in the development of brain oedema associated with LPM. The origin of this tumour (neoplastic or inflammatory) is unclear, so it is considered closer to intracranial inflammatory masses rather than typical meningiomas.7
The differential diagnoses include collision tumour of meningioma and plasmacytoma, inflammatory pseudotumour, idiopathic hypertrophic pachymeningitis (IHP), and intracranial plasma cell granuloma.3,7 The use of staining for EMA and vimentin is useful in indicating the meningothelial origin of the tumour, and differentiates LPM from other intracranial lesions.9
The pathological findings of IHP usually include thickened fibrotic dura mater with marked infiltration of lymphocytes and plasma cells, occasionally accompanied with small islands of meningothelial proliferation mimicking those of LPM. Localised nodular lesion can sometimes rule out this diagnosis in that IHP usually shows diffused lamellar thickenings or plaque-like features.4
Chordoid meningiomas often contain regions that are histologically similar to chordoma, with cords or trabeculae of eosinophilic, vacuolated cells in a background of abundant mucoid matrix background.3 Detailed histological studies can aid the differential diagnosis. The plasma cell component is not neoplastic and thus plasmacytoma with reactive meningothelial hyperplasia or a collision tumour involving meningioma and plasmacytoma can both be excluded.10
The knowledge of this rare entity is important to avoid its underdiagnosis as an inflammatory pseudotumour or plasma cell granuloma and overdiagnosis as a plasmacytoma.
|
Competing Interests None declared Author Details MANVEEN KAUR, MD Pathology, Senior Resident, National Institute of Pathology, ICMR, New Delhi. VARSHA DALAL, MD Pathology, Senior Resident, National Institute of Pathology, ICMR, New Delhi. KARAM CHAND SHARMA, Head of department, Department of Neurosurgery, Vardhman Mahavir Medical College and Safdarjang Hospital, New Delhi. AVNINDER SINGH, Scientist D, National Institute of Pathology, ICMR, New Delhi. CORRESPONDENCE: AVNINDER SINGH, Scientist D, National Institute of Pathology, ICMR, New Delhi. Email: avninders@hotmail.com |
References
- Perry A, Louis DN, Scheithauer BW et al. Meningeal tumours. In: Louis DN, Ohgaki H, Weistler OD, Cavenee WK (eds). WHO Classification of Tumours of the Central Nervous System. 4th ed. Lyon: IARC; 2007. p. 163-72.
- Moradi A, Semnani V, Djam H et al. Pathodiagnostic parameters for meningioma grading. J Clin Neurosci 2008; 15:1370–1375.
- Zhu HD, Xie Q, Gong Y et al. Lymphoplasmacyte-rich meningioma: our experience with 19 cases and a systematic literature review. Int J Clin Exp Med 2013; 6: 504–515.
- Hosler MR, Turbin RE, Cho ES et al. Idiopathic hypertrophic pachymeningitis mimicking lymphoplasma-cyte-rich meningioma. J Neuroophthalmol 2007; 27: 95-98
- Bruno MC, Ginguene C, Santangelo M et al. Lymphoplasmacyte rich meningioma: a case report and review of the literature. J Neurosurg Sci 2004; 48:117–24.
- Liu JL, Zhou JL, Ma YH et al. An analysis of the magnetic resonance imaging and pathology of intracal lymphoplasmacyte-rich meningioma. Eur J Radiol 2012; 81: 968-973.
- Gi H, Nagao S, Yoshizumi H et al. Meningioma with hypergammaglobulinemia. Case report. J Neurosurg 1990; 73: 628-629.
- Katayama S, Fukuhara T, Wani T et al. Cystic lymphoplasmacyte-rich meningioma--case report. Neurol Med Chir 1997;37:275–278
- Avninder S, Gupta V, Sharma KC. Lymphoplasmacyte-rich meningioma at the foramen magnum. Br J Neurosurg. 2008;22:702-4.
- Horten BC, Urich H, Stefoski D. Meningiomas with conspicuous plasma cell-lymphocytic components: a report of five cases. Cancer 1979; 43: 258-264.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




