S.M. Coughlin, I. Walker and W.S. Wassif
Abstract
The impact of extending the cut-off time for the provision of Troponin T assay from 4:00 to 7:00 pm, focusing specifically on same-day patient discharge was studied over a four-month period. The number of patients discharged on the same day, who would have otherwise been admitted overnight, was determined. The fiscal benefit of the extended laboratory service was then calculated. Of the 140 patients included in the study, 36 (26%) patients were discharged on the day of hospital presentation based on a negative Troponin T concentration; all except one had a Troponin T <0.03ug/L. Based on the cost of overnight stay of £657 we concluded that the extended service would save the hospital £70,956 annually.
Extending the provision of Troponin T assay for 3 hours daily is cost effective and reduces the number of unnecessary hospital admissions of patients presenting with chest pain of non-cardiac origin.
Keywords: Troponin T, lipid profile, cost-effectiveness, hospital admission
|
Introduction
Troponin T is a protein component of cardiac muscle. When death or damage of the myocardium occurs, it is released in to the circulation and can be detected by immunoassays 1. Troponin T is a sensitive and specific marker of myocardial damage when taken at least 12 hours after a suspected cardiac event and can be detected up to 7-10 days after myocardial damage 1,2. When used in conjunction with clinical history, electrocardiograms (ECGs) and cardiac imaging it is effective in excluding acute coronary syndrome (ACS) and myocardial infarction (MI). The cost of a Troponin T assay is £3.75 per sample inclusive of staff time.
Troponin concentrations have been incorporated in up to date definitions of acute MI. One of the criteria for diagnosis of acute MI is the detection of rise and/or fall of cardiac biomarkers (Troponin) with at least one value above the 99th percentile of the upper reference limit (URL) together with evidence of myocardial ischaemia with at least one of the following: ischaemic symptoms, new ischaemic ECG changes, pathological Q waves on ECG, or imaging suggesting loss of viable myocardium or new regional wall abnormality 3. Other criteria include unexpected cardiac death involving cardiac arrest, Troponin concentrations associated with percutaneous coronary intervention (PCI) and coronary bypass grafting (CABG) and pathological findings of acute MI 3. Troponin T is an important component of the risk stratification of patients with acute myocardial ischaemia and can be used to predict 30-day mortality 4,5.
Detection of a rise and/or fall in Troponin T concentration is important when diagnosing acute MI 3,6. It is the rise and fall that differentiates individuals who have sustained myocardial damage from other causes such as chronic kidney disease (CKD) 3, 7. In these other conditions the elevated Troponin T concentrations are sustained. To establish the diagnosis of MI, one elevated value above the decision level is required. The demonstration of a rise and/or fall in Troponin T levels assists clinicians in distinguishing elevated background Troponin T concentrations from elevations in the same patients suggestive of MI. Detection of rise and/or fall also identifies those patients with re-infarction within a short time period after an acute MI 8.
It is important to remember however that if the patient presents 24 hours after the onset of symptoms this rise and fall of Troponin T concentration is not necessary to make the diagnosis of MI. Troponin T levels must be interpreted in the light of the clinical presentation. An elevated concentration of Troponin T in the absence of clinical evidence of ischaemia should prompt a search for other aetiologies, such as CKD, congestive heart failure, myocarditis, aortic dissection, or pulmonary embolism 3, 6.
Risk stratification also includes the measurement of lipid profile in those presenting with suspected ACS or MI. To ensure that a cholesterol level representative of the patient’s normal baseline the blood sample must be organised within 24 hours of the event. In those with delayed presentation or where cholesterol is omitted on admission clinicians should wait until 3 months after the event to obtain a reliable cholesterol level, although most would be expected to have started lipid-lowering medications 9,10,11.
Method
We studied Troponin T requests made between 4pm and 7pm for a four-month period. Request cards were retrieved and the Troponin T result for each request was obtained. Any other Troponin T results obtained at any time relating to that event were noted as well as any rise and fall of the Troponin T concentrations. Review of the hospital notes for each patient established the working diagnosis, whether any other appropriate investigations had been carried out during admission, co-morbidities that were present and current relevant medications.
The final patient outcome was noted. The number of patients discharged on the same day, who would have otherwise been admitted overnight, based on Troponin T concentration was determined. Those patients with a Troponin T concentration above the 99th percentile of the upper reference limit (URL) used in the local laboratory (Troponin T <0.03ug/L) who were not discharged on the day of Troponin T measurement were identified and the reason for admission determined. The fiscal impact of the extended laboratory service was calculated.
Results
Of 162 Troponin T requests received during the four-month period, 140 (86%) were included in the study; 22 (14%) were excluded (12 haemolysed, 1 unlabelled, 2 not on computer system, 7 clinical notes unavailable).
The study population comprised of 74 (53%) male and 66 (47%) female patients. The age range was 21 – 101 years; mean (±SD) 67.6 (±16.8).
Half of Troponin T requests were received from the Acute Assessment Unit (AAU), 20% from the Emergency Department, 14% from inpatients, 8% from the Critical Care Complex (CCC) and 8% from the Coronary Care Unit (CCU).
Clinical notes indicated that 97 (69%) of Troponin T requests were taken appropriately at least 12 hours after the onset of the event, 19 (14%) were taken less than 12 hours after the event, in the remaining 24 (17%) the time of sample in relation to the event was not known. Interestingly only 30% of request cards had documented that sample was taken at least 12 hours after the event.
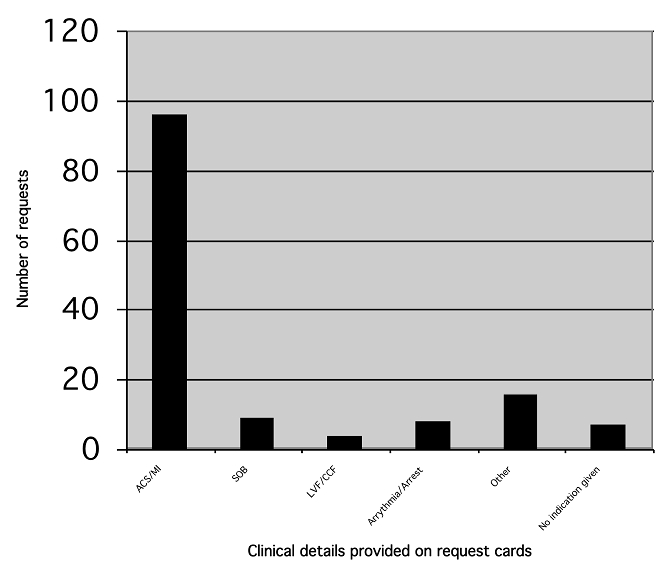
The indication documented on each request card is detailed in Figure 1. Indications detailed under other included: trauma, sepsis, collapse, cold & clammy, oesophageal cancer with hypercalcaemia, poor complex tachycardia, post-operative after abdominal aortic aneurysm repair, respiratory infection, sweating, palpitations, fall and repeat bleed because of previously unsuitable sample.
Figure 1: Indication noted on request card for Troponin T. ACS: acute coronary syndrome, MI: myocardial infarction, SOB: shortness of breath, LVF: left ventricular failure, CCF: congestive cardiac failure.
One hundred and two (73%) patients had a non-elevated Troponin T concentration of <0.030ug/L and 38 (27%) had an elevated Troponin T concentration >0.03ug/L. Only 5 (4%) patients had the rise and fall of Troponin T documented.
Eighty-three (59%) patients had no lipid profile measured during the attendance/admission. Of the remaining 57 patients, 31 (54%) had cholesterol assayed within 24 hours of the event, in 16 (28%) the cholesterol was taken between 2 and 17 days after the event and in 10 (18%) patients the time of cholesterol assay in relation to the event was not known. Overall only 1 in 5 patients had a lipid profile obtained within 24 hours of the event.
Interestingly of the 38 patients with raised Troponin T concentration of >0.03ug/L only 13 (34%) had a lipid profile organised. Only 7 of the 13 (54%) were obtained within 24 hours of the event, 4 were taken between 2 and 10 days after the event and in 2 patients it was not known when the lipid profile was obtained in relation to the event.
Overall no correlation was noted between cholesterol and Troponin T concentrations in all patients who had an elevated Troponin T concentration and cholesterol measured. Interestingly in those where cholesterol was measured within 24 hours of the suspected cardiac event there was some correlation, but the numbers involved were small.
The working diagnosis as stated in hospital notes is documented in Table 1.
Table 1: Working Diagnosis
|
Working Diagnosis
|
Number (%)
|
|
ACS/MI
|
62 (44.3%)
|
|
Arrythmia/Arrest
|
8 (5.5%)
|
|
Fast AF/atrial flutter
|
6 (4.3%)
|
|
CCF/LVF
|
5 (3.6%)
|
|
Myocarditis
|
1 (0.7%)
|
|
Musculoskeletal chest pain
|
7 (5.0%)
|
|
Respiratory complaint
|
18 (12.9%)
|
|
GORD put in legend
|
4 (2.9%)
|
|
Other
|
11 (7.9%)
|
|
No diagnosis
|
18 (12.9%)
|
|
Total
|
140 (100%)
|
ACS, acute coronary syndrome; MI, myocardial infarction; AF, atrial fibrillation; CCF, congestive cardiac failure; LVF, left ventricular failure; GORD, gastro-oesophageal reflux disease.
Table 2: Reason why those patients with non-elevated Troponin T concentration of <0.03 (ug/L) were not discharged on the same day by the clinician.
|
Reason for admission
|
Number of patients
|
|
Trop T assayed <12hrs
|
5 (8%)
|
|
Ongoing chest pain
|
10 (15%)
|
|
ECG changes
|
3 (5%)
|
|
High CAD risk patient
|
2 (3%)
|
|
Monitoring and cardiology review
|
2 (3%)
|
|
Already inpatient
|
7 (10%)
|
|
Repeat attendance in 24hrs
|
1 (1%)
|
|
Other medical (non-cardiac) problem
|
28 (42%)
|
|
No reason documented
|
6 (9%)
|
|
Outcome not available
|
1 (1%)
|
|
Self discharge
|
2 (3%)
|
|
Total
|
67 (100%)
|
All of the 36 (26%) patients except one who were discharged on the day of Troponin T assay had a negative Troponin T concentration of <0.030ug/L. This patient had CABG one month previously and presented with chest pain and associated cough, although his Troponin T was 0.14ug/L, this was deemed not significant in view of a previous Troponin T concentration of 0.16ug/L assayed two days earlier.
Sixty three (45%) patients remained in the AAU or were admitted to a medical ward, 15 (11%) were admitted to CCU, 4 (3%) to CCC and 18 (13%) were already inpatients. Of the remaining 3 patients, 2 self-discharged and in 1 the final destination was not available.
Of those patients with a raised Troponin T concentration of >0.03ug/L 5 died during this attendance.
The majority (60/102) of patients in whom Troponin T was not raised (<0.030ug/L) still required hospital admission (Table 2). Another 6 patients with a non-elevated Troponin T concentration had no obvious reason for admission documented.
Based on an overnight stay cost of £657 we conclude that the laboratory’s extension of Troponin T service of 3 hours would save the hospital £70,956 annually. No additional manpower was required to provide the extended laboratory service as Biomedical Scientists are already providing urgent out of hour on-call service for other biochemical analysis. No additional laboratory costs were incurred, as the same number of samples would have been analysed during working hours the following day.
Discussion
There was sufficient demand for Troponin T assay to justify extension of the laboratory service for 3 hours each day. As expected most requests for Troponin T came from the AAU and the Emergency Department where the majority of patients with chest pain of potential cardiac origin would initially present. In those patients presenting with suspected myocardial damage 3 out of 4 had chest pain of non-cardiac origin.
In those patients where the time of event was known the majority had an appropriate Troponin T assay taken at least 12 hours after the event suggesting that most of the medical and nursing staff were well informed. In contrast it appears that only few of the medical profession were aware of the need to measure lipid profile soon after admission as only 1 in 5 patients had their lipid profile organised within 24 hours of the event.
The majority of requests had appropriate clinical details to justify Troponin T request. However one in four requests were deemed inappropriate (Fig. 1). Since Troponin T may be raised in other conditions the assay should be reserved for those patients where myocardial damage is suspected. Inappropriate testing is potentially hazardous and may expose patients to further unnecessary invasive investigations e.g. cardiac catheterisation with associated morbidity and mortality.
In patients presenting with chest pain, Troponin T assayed appropriately >12 hours after onset of the event can be used effectively to exclude myocardial damage and discharge can be made on the basis of this result without the need for admission. A small proportion (6%) of patients with non-elevated Troponin T concentrations who had no obvious reason for admission, were deemed unnecessary.
Dyslipidaemia plays an important role in the risk stratification of patients with suspected ACS or MI, yet only one in five patients with myocardial damage had a lipid profile organised within 24 hours of the event. Cholesterol measurements organised between 2 and 17 days after the event would not have been representative of the true concentration and were deemed inappropriate. Too few lipid profiles were assayed within 24 hours of the event in patients with an elevated Troponin T concentration to determine whether there is any correlation between cholesterol and Troponin T concentrations.
Similarly only a small number of patients had the rise and fall of Troponin T documented. The lack of serial measurements of Troponin T concentrations may have resulted in failure to recognise some patients with other conditions, which may cause elevated Troponin T concentrations and potentially subject them to unnecessary further invasive investigations.
The provision of the extended laboratory service had a positive impact; it enabled earlier discharge of patients with chest pain of non-cardiac origin, resulted in fewer unnecessary overnight hospital admissions and reduced the demand on hospital beds. Extending the service did not result in extra work for junior doctors, on the contrary by improving the efficiency of the process has not only speeded the patient journey but has improved junior doctors’ time-management.
We have shown that extending the provision of Troponin T assay for 3 hours daily has both fiscal and management benefits and reduces the number of unnecessary hospital admissions. Further extension to incorporate a 24-hour laboratory service for this assay would potentially reduce hospital admissions further with more potential savings.
Conclusion
Extending the provision of Troponin T assay for 3 hours daily has fiscal and management benefits and reduces the number of unnecessary hospital admissions of patients presenting with chest pain of non-cardiac origin.
Learning Points
• Extending Troponin T service has a fiscal benefit.
• Rise and fall of Troponin T values should be documented.
• Lipid profile should be organised within 24 hours in all patients presenting with chest pain of potentially cardiac origin.
• Measuring Troponin T where myocardial damage is not clinically suspected is potentially hazardous and may expose patients to further inappropriate and invasive investigations with associated morbidity and mortality.
• In the current climate of litigation detailed documentation is necessary. |
Competing Interests
None declared
Author Details
S.M. COUGHLIN MBBChir DRCOG
I. WALKER Chief Biomedical Scientist, Bedford Hospital
W.S. WASSIF MB ChB MSc CSci MD FRCPath FRCP.Consultant Chemical Pathologist, Bedford Hospital
Departments of Emergency Medicine and Clinical Biochemistry, Bedford NHS Trust, Kempston Road, MK42 9DJ, UK.
CORRESPONDENCE: Stephanie Coughlin GPVTS ST3,
Lower Clapton Health Centre, 36 Lower Clapton Road, London, E5 0PD
Email: dr.stephaniecoughlin@gmail.com |
References
- British Heart Foundation (Factfile 08/2003). What are cardiac troponins?
- Ebell M H, Flewelling D, Flynn C A. A systematic review of Troponin T and I for diagnosing acute myocardial infarction. J Fam Pract 2000; 49: 550-6.
- Thygesen K, Alpert J S, White H D, Joint ESC/ACCF/AHA/WHF task force for redefinition of myocardial infarction, Jaffe A S, Apple F S et al. Universal definition of myocardial infarction. Circulation 2007; 116: 2634-53.
- Ohman E M, Armstrong P W, Christenson R H, Granger C B, Katus H A, Hamm C W et al. Cardiac troponin T levels for risk stratification in acute myocardial ischaemia. New Engl J Med 1996; 335: 1333-42.
- Atkinson P R T, Lawson L A, Shankar S, Cooper J, Wassif W S. Bedside cardiac marker testing as a tool in risk assessment for acute coronary syndromes in the emergency department. The Middle East Journal of Emergency Medicine 2003; 3:1.
- Jaffe A S. Chasing troponin: how long can you go if you can see the rise? J Am Coll Cardiol 2006; 48: 1763-4.
- Le E H, Klootwijk P J, Weimar W, Zietse R. Significance of acute versus chronic troponin T elevation in dialysis patients. Nephron Clin Pract 2004; 98: 87-92.
- Apple F S, Murakami M M. Cardiac troponin and creatine kinase MB monitoring during in-hospital myocardial re-infarction. Clin Chem 2005; 51: 460-3.
- Wattanasuwan N, Khan I A, Gowda R M, Vasavada B C, Sacchi T J. Effect of acute myocardial infarction on cholesterol ratios. Chest 2001; 120: 1196-9
- Sewdarsen M, Vythilingum S, Jialal I, Nadar R. Plasma lipids can be reliably assessed within 24 hours after acute myocardial infarction. Postgrad Med J 1988; 64: 352-6.
- Gore JM, Goldberg RJ, Matsurroto AS, Castelli WP, McNamara PM, Dalen JE. Validity of serum total cholesterol levels obtained within 24 hours of acute myocardial infarction. Am J Cardiol 1984; 54: 722-5.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.