Hypertensive Crises – the Acute Take
Andrew Kristian Grech
Cite this article as: BJMP 2015;8(3):a823
|
|
Abstract Despite chronic hypertension affecting over one billion individuals worldwide, presentation with acute hypertensive crises has been associated with low rates of appropriate management. According to established guidelines this includes lowering of pressure by 25% over the first hour following diagnosis, with target definition and treatment options described hereunder. Oral treatment can prove sufficient in many instances, with potential precipitous pressure drop and inherent detriment to patients borne in mind. Female gender, coronary artery disease and history of antihypertensive therapy (particularly with poor adherence to the latter) are thought to represent risk factors for acute crises. Presenting symptomatology includes headache, chest pain and shortness of breath, dizziness and nausea and emesis. End organ damage is a distinguishing feature in the subtypes of hypertensive crises, with investigation of presenting crises focusing on making this distinction. Keywords: hypertension crisis emergency acute |
Introduction
The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure has long reported chronic hypertension as affecting over one billion individuals worldwide1. While the role of primary care providers in the long term management of this ubiquitous condition cannot be overstated, the hypertensive patient can also present challenges to an acute physician when the control of arterial blood pressure reaches crisis level.
The What
The clinical entity extravagantly referred to as a hypertensive crisis describes an elevated systolic blood pressure of >180mmHg with diastolic pressure of >120mmHg. Within this category of acute presentations, two subcategories are defined – the hypertensive urgency and the hypertensive emergency. Flamboyant terminology aside, what distinguishes the latter ‘emergency’ from the former ‘urgency’ is evidence of acute end-organ damage. Emergencies therefore include various incipient pathologies of the cardiovascular, renal and central nervous systems. Fortunately these are less common encounters for receiving physicians, with a recent large multicentre study identifying acute pulmonary oedema (30.9%), myocardial infarction (17%), acute aortic dissection (7.9%), acute kidney injury (5.9%), cerebrovascular accident (22%) and hypertensive encephalopathy (4.9%) as features of hypertensive emergencies in 25.3% of hypertensive crises, with the remainder of the presenting population demonstrating a hypertensive urgency with inherent lack of evidence of end organ damage2.
The Why
The pathophysiology of acute hypertension remains yet to be fully elucidated, however authors in the field of hypertensive crisis3,4 appear to converge on the point of two common proposed pathophysiological events. A sharp elevation in systemic vascular resistance is thought to be one precipitating factor, with an aberrance of cerebral autoregulation of blood flow being another.
For the purposes of an acute clinician faced with a bleeping blood pressure monitor, what is perhaps more applicable to everyday clinical practice is the potential role of non-adherence to regular antihypertensive medications5,6as discussed below.
The Who
A longitudinal study carried out in Switzerland and led by Saguner7identifies several potential risk factors for manifestation of a hypertensive crisis. Female gender, obesity and concurrent somatoform disorder accompany hypertensive and coronary artery related cardiac disease as potential red flags. Perhaps unsurprisingly, a history of multiple antihypertensive therapies was also associated with greater likelihood of presentation with hypertensive crises, as was non-adherence to the same therapeutic regimen. The latter compliance related issue was identified as the most significant by the study’s authors.
Elderly patients and also those of African American ethnicity have been shown to demonstrate higher rates of hypertensive crises in general8, while Caucasian patients are reported to have higher rates of emergencies as opposed to the more benign urgency equivalent9.
The When
The findings of a comparatively small Italian hospital-based study10utilising 360 patients were recently supported by a larger United States-based analysis11of over 400,000 patients, with a seasonal variation in presentation of hypertensive crises noted. A winter peak and summer trough was reported by both groups of authors, suggesting transcontinental extrapolation of a potential seasonal phenomenon.
Evaluation
Comprehensive disposition notwithstanding, acute physicians are urged to adopt a targeted approach when considering a presentation with alarming blood pressure readings.
Present…
By nature of definition, the presentation of a hypertensive crisis encompasses a wide variety of symptomatology depending on whether a hypertensive urgency or incipient emergency is manifested.
The symptomatology of a patient demonstrating hypertensive urgency can be fairly non-specific to acute blood pressure elevation. A 2014 study into clinical presentation of hypertensive crises reported headache as the most prevalent symptom (74.11% of patients), followed by chest discomfort and dyspnoea (62.35%), vertiginous dizziness (49.41%), nausea and emesis (41.47%)12 as demonstrated in Figure 1.
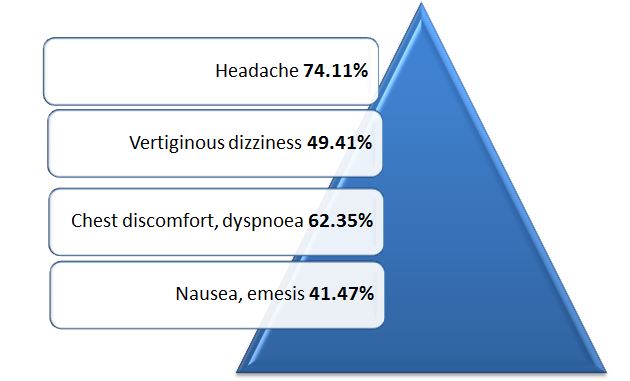
Figure 1. Symptomatology in hypertensive crises (adapted from Salkic S, Batic-Mujanovic O, Ljuca F, et al12)
While all of these common presenting complaints can bring a patient to a physician’s attention, what often alerts the attending physician to the particular possibility of an acute hypertensive condition is the blood pressure reading obtained on initial assessment of the patient (for instance for triage purposes) even in the absence of overt symptomatology as reported above. Indeed, patients with minimal symptomatology may be prompted to present themselves for acute medical care by no more than the sounding of an ominous alarm on a home blood pressure reader or the disconcerted look of a perturbed primary care physician, sphygmomanometer in hand!
…and Past
The history taking process of an acute physician faced with a hypertensive crisis should target several key areas which may prove essential in differentiating a case of urgency from an evolving emergency. With the potential for end organ heart, kidney and brain-related complications in mind, a physician should probe the possibility of chest discomfort, dyspnoea and signs of congestive cardiac failure (as indicators for incipient cardiovascular complications), headache, visual changes, dizziness and altered consciousness (potential harbingers of neurological complications) as well as recent history of oliguria as a marker of possible related renal insult.
Having conducted an interrogation for worrisome symptomatology, evaluation should proceed to a ‘hypertension history’. Prior diagnosis of hypertension and hypertensive crises in particular should be elaborated on, with this including a history of any prescribed regular antihypertensive therapy and both the adherence to and effect of the latter. Relevant to the notorious polypharmacy patients, any history of concurrent medication use must be clarified so as to give an indication of potential interactions.
Of historical note is the potential for hypertensive crisis following interaction of tyramine with mono-amine oxidase inhibitors (the so-called cheese effect), while a provoked hypertensive crisis more relevant to modern medicine is the potential effect of illicit substances including cocaine and amphetamine-based products13.
Examination
As with the evaluation of the hypertensive crisis patient’s history, examination should place particular emphasis on distinguishing urgency from emergency.
Parameters
Assessment of vital signs can provide valuable indicators. Whilst initial systolic pressure is not necessarily a predictor of the ability to achieve a prespecified target range pressure within thirty minutes14, the presence of tachycardia has been shown to be an ominous sign more prevalent in emergency than urgency, with a strong statistical association demonstrated with hypertension-related left ventricular failure15.
Physical
Cardiovascular examination should assess for the presence of signs of cardiac failure (including an elevated jugular venous pressure, added S3 heart sound or pulmonary rales) as well as the feared asymmetric pulses or new mid-diastolic murmur associated with aortic dissection. Auscultation for renal bruits should be performed, and a neurological assessment for possible stroke indicators undertaken.
Whilst chronic hypertension patients will often have subtle fundoscopic abnormalities, ophthalmological review for evidence of acute changes including new retinal haemorrhages or exudates together with papilloedema should be carried out.
Investigation
The unique circumstances of individual presentations aside, the prompt acute medical investigation of a hypertensive crisis should include a minimum number of bedside, laboratory and imaging investigations16as suggested in Figure 2. Comparison of each of these to pre-existing baseline investigations may be invaluable in giving an indication of level of acute pathology and therefore care required.
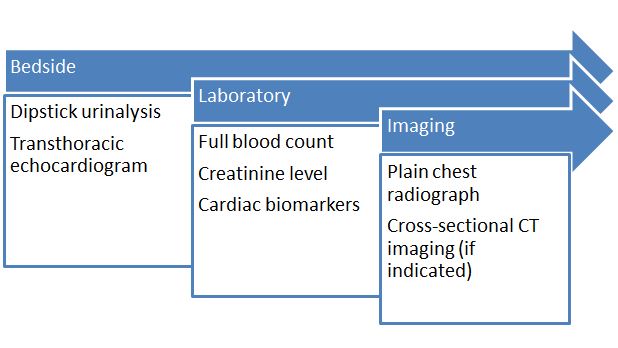
Figure 2. Investigations in hypertensive crises
Bedside
Electrocardiography affords rapid exclusion of major acute ischaemic cardiac events, as well as providing an indication of chronic hypertrophic changes and a quantitative indicator of heart rate elevation. Simple dipstick urine testing can assist in exclusion of significant proteinuria pending formal urinalysis studies16.
Laboratory
Full blood count analysis will give an indication of haemoglobin level where dissection is suspected, while serum markers of renal profile including creatinine level in particular may suggest varying degrees of acute kidney injury where present. Cardiac biomarkers may complement electrocardiography in exclusion of acute events.
As ever, a metabolic panel and blood gas analysis represent valuable tools in the acute physician’s arsenal where acute and evolving physiological disturbances are suspected.16
Imaging
Presence of pulmonary congestion in keeping with left ventricular failure as well as the mediastinal widening of an aortic dissection may be assessed via simple chest radiography. More complex imaging such as computerised tomographic (CT) scanning may be indicated as dictated by clinical presentation, as in the event of neurological manifestations16.
Treatment
Established guidelines1 suggest definitive management of a hypertensive emergency should involve lowering of blood pressure by 25% in the first hour and then to 160/100-110mmHg thereafter if stable, as indicated in Figure 3. Meticulous and continuous monitoring in an intensive care setting for parenteral administration of antihypertensive agents including labetalol17, clevidipine18–20 and fenoldopam21 is beyond the scope of most practising acute physicians.
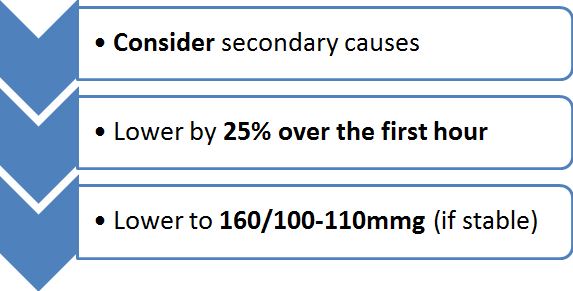
Figure 3. Broad management of a hypertensive emergency (adapted from Chobanian A V, Bakris GL, Black HR, et al1 and Börgel J, Springer S, Ghafoor J, et al26
Hypertensive urgency, however, need not require such invasive interventions, with oral therapy utilising labetalol, captopril or clonidine followed by a period of vigilant observation usually proving sufficient1,17. A once popular practice of oral nifedipine is advised against, owing to the precipitous drop in pressure with inherent risk of tissue ischaemia observed on administration of this agent1. Emergent pharmaceutical options including novel felodipine formulations22 may also be considered.
A pitfall of physicians, perhaps, panicked by the jargon ‘hypertensive urgency’ has been observed, with inappropriate management in such cases reported in multiple independent studies in recent years23–25, with a 42.6% appropriate treatment rate in one study25. A chief consideration when faced with hypertensive crises therefore, may be to avoid rash intervention.
Worthy of mention is the potential for common co-prevalent secondary causes of hypertension including sleep apnoea, renal artery stenosis or a state of hyperaldosteronism; present in 15% of cases in one series26, recommendations have been made for consideration of these prior to therapeutic intervention26.
Outcome
There…
Indicators of greater likelihood of admission in patients presenting with severe hypertension may include presence of age >75 years, dyspnoea, altered mental status or creatinine elevation27.
…And Back Again
Following discharge after an admission for acute severe hypertension, a 90-day readmission rate of up to 35% has been reported28; this includes a multiple readmission rate of 41% with similar re-presentation accounting for 29% of this data. Curiously, dyspnoeic initial presentation is emphasised by the same data source as a risk factor for readmission, with additional risk factors including ictal phenomena at initial presentation and history of both drug abuse and prior severe hypertensive admission.
Key Points
Definition
- A hypertensive crisisinvolves pressures of >180mmHg systolic and >120mmHg diastolic
- Ahypertensive urgency does not include end organ damage
- A hypertensive emergency implies end organ damage
Symptomatology
- The commonest symptoms are headache (74.11%), chest discomfort & dyspnoea (62.35%), vertiginous dizziness (49.41%) and nausea & emesis (41.47%)
Investigations
- Bedside should include urinalysis and echocardiography
- Laboratory should include creatinine level
- Imaging should include plain chest radiography
Management
- Blood pressure should be lowered by 25% over the first hour
- In hypertensive urgency, oral therapy is often sufficient
- Consider co-prevalent secondary causes
|
Competing Interests None declared Author Details ANDREW GRECH, M.D. (MELIT.), Department of Emergency Medicine, Mater Dei Hospital, Msida MSD 2090, Malta. CORRESPONDENCE: ANDREW GRECH, Department of Emergency Medicine, Mater Dei Hospital, Msida MSD 2090, Malta. Email: andrew-kristian.grech@gov.mt |
References
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42(6):1206-52. doi:10.1161/01.HYP.0000107251.49515.c2.
- Pinna G, Pascale C, Fornengo P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS One 2014;9(4):e93542. doi:10.1371/journal.pone.0093542.
- Smithburger PL, Kane-Gill SL, Nestor BL, et al. Recent advances in the treatment of hypertensive emergencies. Crit. Care Nurse 2010;30(5):24-30; quiz 31. doi:10.4037/ccn2010664.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs 2008;68(3):283-97. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18257607. Accessed December 2, 2014.
- Lip GY, Beevers M, Potter JF, et al. Malignant hypertension in the elderly. QJM 1995;88(9):641-7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7583078. Accessed December 4, 2014.
- Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest 2000;118(1):214-27. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10893382. Accessed December 4, 2014.
- Saguner AM, Dür S, Perrig M, et al. Risk factors promoting hypertensive crises: evidence from a longitudinal study. Am. J. Hypertens. 2010;23(7):775-80. doi:10.1038/ajh.2010.71.
- Varon J, Marik PE. Clinical review: the management of hypertensive crises. Crit. Care 2003;7(5):374-84. doi:10.1186/cc2351.
- Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, et al. Hypertensive crisis: clinical-epidemiological profile. Hypertens. Res. 2011;34(3):367-71. doi:10.1038/hr.2010.245.
- Marchesi C, Dentali F, Maresca AM, et al. Seasonal and monthly variation in occurrence of hypertensive urgency. Intern. Emerg. Med. 2013;8(3):269-71. doi:10.1007/s11739-012-0878-6.
- Pant S, Badheka AO, Mehta K, et al. Seasonal and monthly variation in occurrence of hypertensive urgency. Intern. Emerg. Med. 2013;8(3):273. doi:10.1007/s11739-013-0905-2.
- Salkic S, Batic-Mujanovic O, Ljuca F, et al. Clinical presentation of hypertensive crises in emergency medical services. Mater. Sociomed. 2014;26(1):12-6. doi:10.5455/msm.2014.26.12-16.
- Varon J, Polanski M. Hypertensive Crises: Recognition and Management. Internet J. Anesthesiol. 1997;Vol I.
- Farias S, Peacock WF, Gonzalez M, et al. Impact of initial blood pressure on antihypertensive response in patients with acute hypertension. Am. J. Emerg. Med. 2014;32(8):833-6. doi:10.1016/j.ajem.2014.03.021.
- Al Bannay R, Böhm M, Husain A. Heart rate differentiates urgency and emergency in hypertensive crisis. Clin. Res. Cardiol. 2013;102(8):593-8. doi:10.1007/s00392-013-0570-5.
- Stewart DL, Feinstein SE, Colgan R. Hypertensive urgencies and emergencies. Prim. Care 2006;33(3):613-23, v. doi:10.1016/j.pop.2006.06.001.
- Varon J. The diagnosis and treatment of hypertensive crises. Postgrad. Med. 2009;121(1):5-13. doi:10.3810/pgm.2009.01.1950.
- Varelas PN, Abdelhak T, Corry JJ, et al. Clevidipine for acute hypertension in patients with subarachnoid hemorrhage: a pilot study. Int. J. Neurosci. 2014;124(3):192-8. doi:10.3109/00207454.2013.836703.
- Ndefo UA, Erowele GI, Ebiasah R, et al. Clevidipine: a new intravenous option for the management of acute hypertension. Am. J. Health. Syst. Pharm. 2010;67(5):351-60. doi:10.2146/ajhp080692.
- Awad AS, Goldberg ME. Role of clevidipine butyrate in the treatment of acute hypertension in the critical care setting: a review. Vasc. Health Risk Manag. 2010;6:457-64. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2922306&tool=pmcentrez&rendertype=abstract. Accessed December 2, 2014.
- Rodriguez MA, Kumar SK, De Caro M. Hypertensive crisis. Cardiol. Rev. 18(2):102-7. doi:10.1097/CRD.0b013e3181c307b7.
- Basalious EB, El-Sebaie W, El-Gazayerly O. Rapidly absorbed orodispersible tablet containing molecularly dispersed felodipine for management of hypertensive crisis: development, optimization and in vitro/in vivo studies. Pharm. Dev. Technol. 18(2):407-16. doi:10.3109/10837450.2012.659258.
- Devlin JW, Dasta JF, Kleinschmidt K, et al. Patterns of antihypertensive treatment in patients with acute severe hypertension from a non-neurologic cause: Studying the Treatment of Acute Hypertension (STAT) registry. Pharmacotherapy 2010;30(11):1087-96. doi:10.1592/phco.30.11.1087.
- Fursov AN, Potekhin NP, Chernov SA, et al. [Hypertensive crisis: problems of diagnostics and paradigm of the treatment]. Voen. zhurnal 2012;333(7):11-5. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23038954. Accessed December 2, 2014.
- Monteiro Júnior F das C, Anunciação FAC, Salgado Filho N, et al. Prevalence of true hypertensive crises and appropriateness of the medical management in patients with high blood pressure seen in a general emergency room. Arq. Bras. Cardiol. 2008;90(4):247-51. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18516384. Accessed December 2, 2014.
- Börgel J, Springer S, Ghafoor J, et al. Unrecognized secondary causes of hypertension in patients with hypertensive urgency/emergency: prevalence and co-prevalence. Clin. Res. Cardiol. 2010;99(8):499-506. doi:10.1007/s00392-010-0148-4.
- Kleinschmidt K, Levy P, Wyman A, et al. Emergency department patients with acute severe hypertension: a comparison of those admitted versus discharged in studying the treatment of acute hypertension registry. Crit. Pathw. Cardiol. 2014;13(2):66-72. doi:10.1097/HPC.0000000000000014.
- Gore JM, Peterson E, Amin A, et al. Predictors of 90-day readmission among patients with acute severe hypertension. The cross-sectional observational Studying the Treatment of Acute hyperTension (STAT) study. Am. Heart J. 2010;160(3):521-527.e1. doi:10.1016/j.ahj.2010.06.032.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




