Generalized Lymphadenopathy : an unusual presentation of syphilis
Naziha Khammassi, Asma Gargoura, Haykel Abdelhedi, Youssef Kort, Manel Mabrouk and Ouahida Cherif
Cite this article as: BJMP 2015;8(3):a827
|
|
Abstract This report describes a case of secondary syphilis represented by generalized lymphadenopathy . Histopathological analysis of biopsy specimen revealed the presence of a well-developed epithelioid granuloma including central areas of caseous necrosis . As granuloma formation can be seen in numerous diseases, additional clinical and laboratory diagnoses are necessary aids in the diagnosis of the granuloma aetiology .In this case granulomatous lesion with caseous necrosis was highly suggestive of tuberculosis , but the identification by Ziehl-Neelsen staining was negative.However, the serologic tests of syphilis (VDRL and TPHA) confirmed the diagnosis of syphilis. As illustrated by this case, syphilis should also be considered as a possible cause of generalized lymphadenopathy. Awareness by the clinician of such a presentation would make it easy to diagnose syphilis at an earlier stage. Keywords: Syphilis; Granuloma; Diagnosis; Lymphadenopathy; Caseous necrosis. |
Introduction
As syphilis is a notable clinical and pathological imitator, its diagnosis remains challenging. Physicians should be vigilant to suspect syphilis in cases of non-specific signs, such as lymphadenopathies, even in patients with no apparent risk for sexually transmitted infections or a history of primary syphilis.
Case Report
We report the case of a seventy-year old woman with a medical history of arterial hypertension. She had neither smoked cigarettes nor drunk alcohol and she had no significant medical family history. The patient presented with a history of swelling in the left axilla of one year duration. The swelling gradually increased in size and was painless. There was a history of occasional low-grade fever and weight loss, but no cough or night sweats.
On initial examination, the patient was thin with generalised lymphadenopathy: she had an axillary adenopathy that measured 4 cm in diameter in the right axilla and one measuring 3 cm in the left axilla. She also had two cervical lymph nodes that were less significant, and one enlarged right inguinal lymph node of about 3 cm in diameter. The existing lymph nodes were painless, mobile, mildly tender and smooth. Otherwise, breasts, limbs and other regions were essentially normal. No skin rash or suspect lesions were noticed. All her family members were well, with no contributory medical history, and none of them had similar symptoms.
A complete blood count revealed a white blood cell count of 5300/l (neutrophils 40%, eosinophils 19%, lymphocytes 30%, monocytes 10%), and a C-reactive protein of 14 mg/l. The remaining results of her full blood count, electrolytes, liver enzymes, lactate dehydrogenase and urine analysis were within normal limits. Calcium and phosphate levels were normal in both blood and urine analyses. Both human immunodeficiency virus screening and the serological tests for hepatitis B and C were negative. Mantoux test did not show any indurations. Smear and culture of the sputum were negative. Her chest x-ray and abdominal ultrasound were normal.
A CT scan of the patient’s neck and chest showed a marked anterior mediastinal mass of about 50 mm diameter with multiple calcifications. Several small lymph nodes were also noticed in the cervical and axillary areas. An axillary lymph node biopsy was performed. Histopathological examination of the biopsy specimen revealed a granulomatous lesion with epithelioid and multinucleated giant cells (Fig.1) associated with calcifications and central areas of caseous necrosis (Fig.2), which were highly suggestive of tuberculosis.
Fig 1: Epithelioid granuloma with giant cell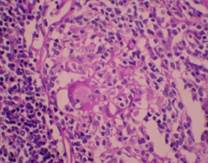
Fig 2: Eosinophilic granuloma with acellular caseous necrosis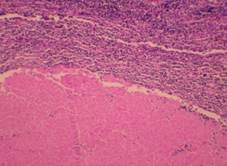
According to these clinical and pathological findings, the most common granulomatous diseases are mycobacterial diseases such as tuberculosis, hence why the diagnosis of tuberculous lymphadenitis was highly suspected, and the patient was given anti-TB drugs. However, other differential diagnoses were considered, including bacterial infections like syphilis or actinomycosis, protozoal infections such as toxoplasmosis, and miscellaneous diseases such as sarcoidosis, Crohn's disease and Wegener's granulomatosis. To distinguish disease processes and make a definitive diagnosis, further investigations, such as special stains, culture methods and serologic tests, were indicated.
Additional histological stains, including Ziehl-Nielsen, were performed and returned negative, excluding the diagnosis of tuberculosis. In the meantime, the serological tests showed a positive venereal disease research laboratory test (VDRL: 1/8) and Treponema Pallidum haemagglutination assay (TPHA: 1/350). As a result, the diagnosis of secondary syphilis was confirmed and tuberculosis treatment was ceased.
The patient received intramuscular injections of 2.4 million units of benzathine penicillin every three weeks. Additional clinical and laboratory examinations were performed for both the patient and her family. She did not present with any manifestations of cardiovascular or neurological syphilis. Her husband’s VDRL and TPHA tests were negative. After a nine-month follow-up, the patient had no clinical or laboratory evidence of syphilis.
Discussion
Syphilis is predominantly a sexually-transmitted disease with both local and systemic manifestations. The causative organism is the spirochete Treponema Pallidum (TP) which was first demonstrated on the 17th of May 1905 1.
Syphilis has many non-specific signs and symptoms that may be overlooked by the physician, because in some cases it may simply be indistinguishable from other more common diseases. In fact, syphilis can share clinical manifestations with other treponemal and non-treponemal diseases, and it may be asymptomatic in some stages. Unfortunately, undiagnosed and untreated syphilis may lead to life-threatening complications such as hepatitis, stroke and neurological damage 2. Therefore its clinical diagnosis must be supported by laboratory tests.
Several older methods can be used to confirm syphilis diagnosis such as direct identification of TP by dark-field microscopy or direct fluorescent antibody tests, but such tests are not practical in a routine clinical setting and these methods can only be performed on lesion exudate or tissue 3.
As a consequence, the diagnosis in most patients is based on serological tests. Guidelines from the United States of America (USA) and Europe recommend a combination of two tests: the first one is a non treponemal (cardiolipin, reaginic) test, essentially Venereal Disease Research Laboratory (VDRL) or rapid plasma reagin (RPR); and the second is a treponemal test, essentially TP haemagglutination assay (TPHA), TP particle agglutination, or the fluorescent treponemal antibody absorption (FTA-abs) test 3,4.
In our patient, the most significant clinical finding was lymphadenopathy. This case presented diagnostic difficulties because of its clinical and histopathological resemblance to other pathological conditions. In fact, the presence of generalised lymphadenopathy and the finding of granulomatous lesions with epithelioid cells in the biopsy were highly suggestive of tuberculosis. As a matter of fact, tuberculosis tops the list of aetiological causes of granulomatous infections5. Worldwide it is considered the leading cause of contagious disease leading to approximately 1.4 million deaths per year 6. Its prevalence is still extremely high in certain populations especially in low-and middle-income countries such as Tunisia where the disease is endemic.
Tuberculosis is caused by Mycobacterium tuberculosis (M. tuberculosis) and M. bovis, an acid and alcohol fast organism 7,8. Histopathology is characterized by the presence of epitheloid granuloma with Langerhans giant cells and central caseous necrosis 7.
Lymphadenitis is the most common extra-pulmonary manifestation of tuberculosis but its diagnosis is difficult, often requiring biopsy. In such granulomatous disease, and in cases of persisting doubts, it is necessary to identify the specific etiological agent by further investigations such as special stains, culture methods and molecular techniques like polymerase chain reaction (PCR) and serological tests, as in the case of syphilis.
In the case of tuberculosis infection, demonstration of the mycobacteria can be done with Ziehl-Neelsen staining or by immunofluorescence using auramine-rhodamine. Mycobacterial culture and detection of mycobacterial DNA using PCR are also used 7,9. Since the growth of mycobacterium in culture requires a long time, additional histological stain with Ziehl-Nielsen was performed, but returned negative in the case of our patient. As a consequence, the diagnosis of tuberculosis was excluded and syphilis was considered as a definitive diagnosis.
Conclusion
Granulomatous lesions can be seen in numerous diseases. A definitive diagnosis cannot be made on the basis of the history and physical examination alone, confirmatory testing should be performed in order to identify the specific etiologic agent correctly. Diagnosis of the disease in the initial stages would be beneficial not only to allow the patients to receive early treatment, but also to prevent the spread of the disease to others.
|
Competing Interests None declared Author Details NAZIHA KHAMMASSI, ASMA GARGOURA, HAYKEL ABDELHEDI, YOUSSEF KORT, MANEL MABROUK and OUAHIDA CHERIF, Department of Internal Medicine, Razi Hospital, 2010- Manouba, Tunisia. CORRESPONDENCE: NAZIHA KHAMMASSI, Doctor, Department of Internal Medicine, Razi Hospital, 2010- Manouba, Tunisia. Email: naziha.khammassi@rns.tn |
References
- Schaudinn F, Hoffmann E, Vorläufiger Bericht über das Vorkommen von Spirochaeten in syphilitischen Krankheitsprodukten und bei Papillomen, Arbeit Kaiser-Klin. Gesundheits 1905; 22: 527.
- Markle W, Conti T, Kad M. Sexually transmitted diseases. Prim Care. 2013; 40(3):557-87.
- Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006; 55: 997.
- Carol R. Emerson. Syphilis: A Review of the Diagnosis and Treatment. The Open Infectious Diseases Journal, 2009, 3, 143-147.
- Kumar SN, Prasad TS, Narayan PA, Muruganandhan J. Granuloma with langerhans giant cells: An overview. J Oral Maxillofacial Pathol. 2013; 17:420-3.
- World Health Organisation. Global tuberculosis report, WHO Library Cataloguing-in-Publication Data. Switzerland. 2012. p. 3 [chapter 1].
- Diagnostic Standards and Classification of Tuberculosis in Adults and Children. AM J Respir Crit Care Med. 2000; 161(4 Pt 1):1376-95.
- Hernandez-Pando R, Bornstein QL, Aguilar Leon D, Orozco EH, Madrigal VK, Martinez Cordero E. Inflammatory cytokine production by immunological and foreign body multinucleated giant cells. Immunology. 2000; 100:352–8.
- Baek CH, Kim SI, Ko YH, Chu KC. Polymerase chain reaction detection of Mycobacterium tuberculosis from fine-needle aspirate for the diagnosis of cervical tuberculous lymphadenitis. Laryngoscope. 2000 Jan;110(1):30-4.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




