Gastrointestinal bleeding in spinal injuries patient: Is prophylaxis essential?
Fahim Anwar, Ahmad Al-Khayer, Hoda El-Mahrouki and Muriell Purcell
Cite this article as: BJMP 2013;6(1):a607
|
|
Abstract Introduction: Acute gastrointestinal (GI) ulcerations and erosions are common in major trauma victims and in intensive care units. The reported incidence of gastrointestinal haemorrhage in acute spinal cord injuries is between 5 and 22%. |
Introduction
Acute gastrointestinal ulcerations and erosions (stress ulcers) are common in major trauma victims and in intensive care units. In fact, 75% of all critically ill admissions may have endoscopic evidence of gastroduodenal or upper gastrointestinal bleeding1. The bleeding could be in mutiple forms such as haematemesis,coffee ground aspirates, melaena, or haematochezia. Clinically significant haemorrhage causes hypotension and tachycardia and requires blood transfusion. Aggressive management is required in order to improve the outcomes of this potentially fatal complication. Prevention of stress ulcers helps reduce the morbidity and mortality of major bleeding2. Multiple causes may be responsible for gastrointestinal ulceration in patients with spinal cord injury1. Furthermore, steroids, thrombophylactic agents, anticoagulants and heavy cigarette smoking may act as predisposing factors to gastrointestinal bleed.
The aim of this study was to review our practice of stress ulcer prophylaxis after spinal cord injury and analyse morbidity and mortality associated with stress ulcer bleeding.
Patients and Methods
The Queen Elizabeth National Spinal Injuries Unit is the sole spinal cord injury centre in Scotland. It serves a population of 5.1 million and admits approximately 175 acute spinal injuries patients per year.
This study is retrospective. Only cases of life threatening or massive gastrointestinal haemorrhage were included. The period studied is between January 2006 and May 2008.
The department policy is to start all patients on Ranitidine 150 mg twice daily provided they are not on alternative medications before their admission, in which case the policy is to continue with the original pre admission medication.
Clinical notes of included patients were reviewed and information on patient’s demographics, cause and level of injury, past medical history, preadmission medications, clotting profile, prophylaxis, and management of bleeding were collected.
Results
A total of 360 patients were admitted. Out of them 19 (2 Female:17 Male) met the inclusion criteria as they suffered a life threatening GI bleed or major haemorrhage. The age range was 19 to 78 years with a mean age of 51.2 years. The majority of patients had a cervical spine injury (63%) followed by lumbar (21%) and thoracic (16%) spine injuries . Fall down stairs was the most common cause of injury occurring in 6 (31.5%) patients followed by road traffic accidents (26.3%) and fall from a height (21%). One patient suffered spinal injury whilst playing rugby and 1 patient suffered a cycling accident. The majority of cases (17 out 19) were admitted with acute injuries. However, 2 patients were admitted for complications of chronic injuries (one with a post surgical abscess and one with pressure sores). The various causes of spinal injuries are shown in table 1.
The American Spinal Injury Association (ASIA) impairment scales of all 19 patients are shown in Table 2. Associated injuries were encountered in 4 (21%) of patients. These associated injuries include sternum fracture, rib fractures, clavicle fracture, tendon injury and a calcaneum fracture. Significant past medical history was found in 14 (73.6%) patients whereas 5 (26.4%) did not have any previous medical illness. The list of all the significant past medical problems is shown in Table 3.
4 (21%) patients were already taking Omeprazole before admission, whereas 2 (10.5%) were taking Ranitidine and 1 (5.2%) patient was taking Lansoprazole.
7 out of 19 patients (36.8%) had either one or two episodes of significant coffee ground vomiting, 6 (31.5%) patients had an episode of haematemesis and 4 (21%) patients had combined coffee ground vomiting and haematemesis. Two (10.5%) patients had positive nasogastric aspirate for bleeding.
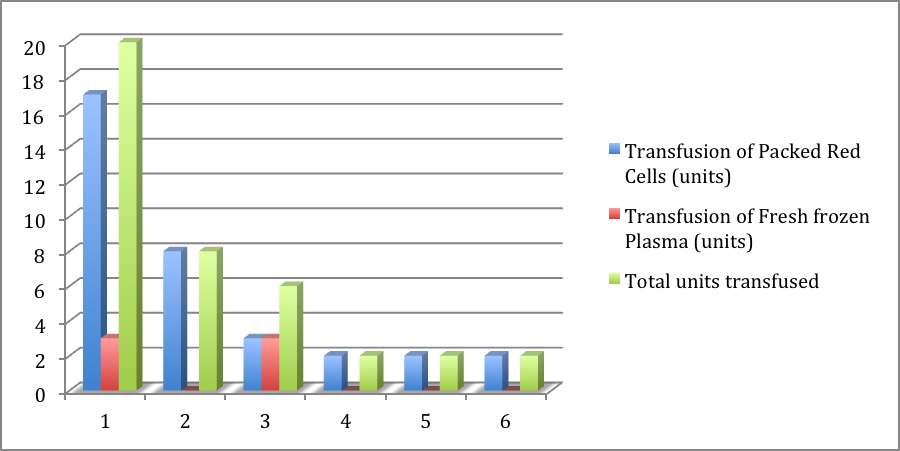
All 19 patients were started on intravenous Omeprazole and Sucralfate was added in 13 patients. Low molecular weight heparin, Ibuprofen and Aspirin was discontinued in all patients. Six (31.5%) patients were transfused 40 units of fresh frozen plasma and packed red cells (Figure 1). Eight patients (42.1%) underwent endoscopic treatment (Table 4) and 3 (15.7%) patients underwent laparotomy. There was one (5.2%) fatality reported.
Table 1:Causes of Spinal Cord Injury
| Cause of Injury | Number of Patients | Percentage |
| Fall from stairs | 6 | 31.5% |
| Road traffic accidents | 5 | 26.3% |
| Fall from height | 4 | 21% |
| Rugby injury | 1 | 5.2% |
| Cycling accident | 1 | 5.2% |
| Old injury admitted with skin problem | 1 | 5.2% |
| Post surgical abscess | 1 | 5.2% |
Table 2:American Spinal Injury Association Impairment Scale
| ASIA Impairment Scale | Number of Patients | Percentage |
| A= Complete: No motor or sensory function is preserved in the sacral segments S4-S5. | 3 | 15.7% |
| B=Incomplete: Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5 | 1 | 5.2% |
| C=Incomplete: Motor function is preserved below the neurological level, and more than half of key muscles below the neurological level have a muscle grade less than 3 | 10 | 52.6% |
| D=Incomplete: Motor function is preserved below the neurological level, and at least half of key muscles below the neurological level have a muscle grade of 3 or more | 2 | 10.5% |
| E=Normal: motor and sensory function are normal | 3 | 15.7% |
Table 3: Previous Risk Factors in Spinal Cord Injured Patients with Stress Ulcers
| Adverse Factor | Number of Patients with the Problem |
| Smoking | 13 (68.4%) |
| Alcohol | 5 (26.3%) |
| Reflux Oesophagitis | 4 (21%) |
| Hypertension | 3 (15.8%) |
| Diabetes Mellitus | 3 (15.8%) |
| Hiatus Hernia | 2 (10.5%) |
| Ischemic Heart Disease | 2 (10.5%) |
| Asthma | 1 (5.3%) |
| Duodenal Ulcers | 1 (5.3%) |
| Anaemia | 1 (5.3%) |
| Pyloric Stenosis | 1 (5.3%) |
Table 4:Endoscopic Findings, Procedures and Outcome
| Number of Patients | Endoscopic findings, Procedures and Outcome |
| 2 | Bleeding Duodenal Ulcer injected with adrenaline Bleeding stopped |
| 1 | Had Endoscopy twice and bleeding Duodenal Ulcer injected with adrenaline on both occasions Continuous bleeding Underwent Laparotomy and over Sewing of the ulcer |
| 1 | Endoscopic findings were Oesophagitis, Hiatus Hernia and superficial ulcerations No procedure performed Treated Conservatively |
| 1 | Bleeding Duodenal Ulcer injected with adrenaline Continuous bleeding Prepared for Laparotomy but could not survive |
| 1 | Bleeding Duodenal Ulcer injected with adrenaline Bleeding stopped Barrett’s oesophagus was found and biopsied but biopsy results were negative |
| 2 | Bleeding Duodenal Ulcer injected with adrenaline Continuous bleeding Laparotomy and over sewing |
Figure 1: Packed Red Cells and Fresh frozen Plasma Transfusion Units Patients
Discussion
The development of “stress” ulceration in the upper GI tract has been part of critical care folklore for a long time. In 1823 Curling described a series of severe duodenal ulceration associated with burns3; in 1832 Cushing reported ulcer disease associated with surgery and trauma4In the early years of intensive care, a strong association between severity of illness and the incidence of GI bleeds was established. Patients who had major bleeds had a high mortality rate and, consequently, prophylaxis against this complication has become a central issue in ICU care.
Gastrointestinal haemorrhage in patients with spinal cord disease was not reported until 1933 when Polstorff described gastric ulceration in an epileptic patient with spontaneous hematomyelia5. El Marsi and colleagues in 1982 reported 5.5% incidence of gastrointestinal bleeding in acute spinal cord injury patients6. Lesions of the spinal cord including traumatic, viral and infectious have been described with gastrointestinal bleeding7. It has been found mainly associated with injury to the cervical spinal cord8.
Controversy still exists regarding the appropriate prophylaxis of stress ulcers in trauma patients. There have been numerous randomized, controlled trials and several meta-analyses evaluating the use of drug therapy for stress ulcer prophylaxis in trauma patients9. One meta-analysis concluded that Sucralfate is as effective as pH-altering medications in preventing stress ulcer bleeding10. There is currently no large study that proves the superiority of proton pump inhibitors over H2- receptor antagonists for stress ulcer prophylaxis 11, 12. A survey of all the Level I trauma centers in the United States by Barletta et al9 revealed that H2-receptor blockers were the preferred agents. It is important to mention that some studies have questioned the need for prophylaxis altogehter but these were mainly retrospective studies that primarily evaluated medical patients as compared to trauma patients13, 14, 15, 16. The reported incidence of gastrointestinal haemorrhage in the medical literature in acute spinal cord injuries is between 5 and 22% 6, 17,18. In our study 19 out of 360 patients (5.2%) suffered a major bleed from the gastrointestinal tract. This incidence is similar to lower percentage reported in the medical literature17, 18. The strict adherence to the department policy of early prophylaxis for all admitted patients could be the reason for this low percentage of significant bleeding.
It is interesting to note that despite the increasing use of steroids and anticoagulants in the last decade, the incidence of gastrointestinal bleeding in acute spinal cord injuries have remained the same. The possible reason for this could be the increased awareness of this condition by spinal cord injury specialists and the regular prophylaxis initiated in the early phases of the injury. Our unit aims to admit patients as soon as they are fit for transfer and approximately 50% of our patients are transferred within the 48 hours of their injury from the peripheral hospitals. The referring hospitals are advised to commence H2 receptor antagonist at the time of referral.
Increasing use of antacids, H2 receptor antagonists and proton pump inhibitors in primary care19 may also contribute to the reduction of the incidence of gastrointestinal bleeding in patients with spinal cord injuries. This assumption is supported by our study as 7 (36.8%) patients in our study were already on these medications prior to their spinal cord injury.
The aetiology of gastroduodenal bleeding in spinal cord injury is multifactorial including, synergetic effects of the stress of the accident along with added effects of concomitant surgery, sepsis, unopposed reduced vagal tone and mucosal ischemia20. Also prolonged mechanical ventilation and coagulopathy has been shown to be associated with increased risk of stress ulcers in spinal injuries21.Other identified risk factors include multiple injuries, acute renal failure and use of high dose steroids22. Croft23 in 1977 first described the dynamics of the surface epithelium in the stomach. He reported that various agents were responsible for the damage of the gastric mucosa; stress, steroids and uraemia were causing decrease in the production of the mucosal cells; and alcohol and aspirin were causing increase in the shed of the gastric mucosal cells. This serious complication usually develops during the first four weeks after the spinal cord injury20,24. However, the period of greatest risk for gastrointestinal haemorrhage is reported to be between the fourth and tenth day after the injury8Nuseilben also reported focal ischemia of the gastric mucosa as early as 24 hours following the acute spinal cord injuries25.
Spinal injuries seldom occur in isolation; in a study by Silver26 in 1985 a 15% incidence of associated injuries was reported. The incidence of associated injuries in our study was 21%.
In a study by Walters and Silver1 all patients that bled had a combination of at least 3 risk factors. In our study 73.6% of patients who developed gastroduodenal bleeding had significant history of risk factors with smoking (68.4%) and alcohol (26.3%) being the major contributors. The other risk factors in our study were reflux oesophagitis (21%), hypertension (15.8%), diabetes mellitus (15.8%), hiatus hernia (10.5%) and ischemic heart disease (10.5%). However, only 7 (36.8%) patients had a combination of three or more risk factors at the time of admission. The reason for this decreased incidence as compared to Walter and Silver1 is difficult to explain.
In this study the majority of patients with gastrointestinal bleeding had cervical cord injuries (63.1%) as compared to thoracic and lumbar spine injuries. Kewalramani20 also showed predominance of gastrointestinal bleeding in patients with cervical cord injuries. This favours the neurogenic hypothesis as a major cause of gastrointestinal bleeding following the spinal injury 20.
Finally, there is no consensus, in literature, over the discontinuation of stress ulcer prophylaxis. Some studies suggest the continuation of prophylaxis throughout the duration of the critical illness or intensive care unit stay27, 28, 29.
Conclusion:
Gastrointestinal haemorrhage is a serious complication in spinal cord injured patients. Appropriate prophylaxis, early diagnosis and prompt management may help to avoid a possible fatality. Patients with spinal cord injury especially with cervical cord injury are at a high risk of gastrointestinal bleeding at all times even during period of rehabilitation30, 31. All acute spinal cord injured patients and patients who are undergoing rehabilitation who become critically ill may benefit from receiving chemical prophylaxis for stress ulceration. The duration of treatment is ill defined but is maybe better to continue while risk factors are present. Prevention could be the cornerstone in the overall management of this problem.
|
Competing Interests None declared Author Details FAHIM ANWAR, MRCSEd, FEBPRM, Consultant in Rehabilitation Medicine, Addenbrooke’s Hospital, Cambridge, CB2 0QQ, UK. AHMAD AL-KHAYER, MRCS, FEBPRM, Consultant in Rehabilitation Medicine, Al-Ahli Hoospital, Doha, Qatar. HODA EL-MAHROUKI, Specialist Registrar, Southern General Hospital, Glasgow, G51 4TF, UK. MURIELL PURCELL, MRCP, Consultant in Spinal Injuries, Queen Elizabeth Spinal Injuries Unit, Southern General Hospital, Glasgow, G51 4TF, UK. CORRESPONDENCE: DR FAHIM ANWAR, MRCSEd, FEBPRM, Consultant in Rehabilitation Medicine, Addenbrooke’s Hospital, Hills Road, Box 248, Cambridge, CB2 0QQ, UK. Email: fanwar10@gmail.com |
References
- Walters K, Silver JR. Gastrointestinal bleeding in patients with acute spinal injuries. Int. Rehabil.Med.1985; 8,44-47.
- Zuckerman GR, Shuman R. Therapeutic goals and treatment options for prevention of stress ulcer syndrome. Am J Med 1987; 18: 83(6A): 29-35.
- Curling TB. On acute ulceration of the duodenum in cases of burns. M Clin Tr London 1842; 25: 260-281.
- Cushing H. Peptic ulcers and the interbrain. Surg.Gynaecol.Obstet 1932; 1.
- Polstorff F. Uber eine seltene Verletzung in epileptischen Anfall mit , Ausgang, gleichzeitig Beitrag zur Entstehung des runden Magengeschwtirs. Psychiatr Neurol Wochenschr 35:566-570, 1933.
- Masri WE, Cochrane P, Silver JR. Gastrointestinal bleeding in patients with acute spinal injuries. Injury 1982 Sep; 14(2):162-7.
- Perret G, Solomon A: Gastrointestinal haemorrhage and cervical cord injuries. Proceedings of the 17th VA Spinal Cord Injury Conference,1969, pp 106-110.
- Leramo OB, Tator, CH, Hudson AR. Massive gastroduodenal haemorrhage and perforation in acute spinal cord injury. Surg Neurol 1982; 3: 186-190.
- Barletta JF, Erstad BL, Fortune JB. Stress ulcer prophylaxis in trauma patients. Critical Care 2002; 6 (6): 526-530.
- Cook DJ, Reeve BK, Guyatt GH, Heyland DK, Griffith LE, Buckingham L, Tryba M. Stress ulcer prophylaxis in critically ill patients. JAMA 1996; 275:308-314.
- Balaban DH, Duckworth CW, Peura DA. Nasogastric omeprazole: effects on gastric pH in critically Ill patients. Am J Gastroenterol1997;92:79-83.
- Mallow S, Rebuck JA, Osler T, et al. Do proton pump inhibitors increase the incidence of nosocomial pneumonia and related infectious complications when compared with histamine-2 receptor antagonists in critically ill trauma patients? Curr Surg 2004;61:452-458.
- Devlin JW, Ben-Menachem T, Ulep SK, et al. Stress ulcer prophylaxis in medical ICU patients: annual utilization in relation to the incidence of endoscopically proven stress ulceration. Ann Pharmacother 1998;32:869-874.
- Faisy C, Guerot E, Diehl JL, et al. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress-ulcer prophylaxis. Intensive CareMed 2003;29:1306-1313.
- Zandstra DF, Stoutenbeek CP. The virtual absence of stress-ulceration related bleeding in ICU patients receiving prolonged mechanical ventilation without any prophylaxis. A prospective cohort study. Intensive Care Med 1994;20:335-340.
- Zeltsman D, Rowland M, Shanavas Z, et al. Is the incidence of hemorrhagic stress ulceration in surgical critically ill patients affected by modern antacid prophylaxis? Am Surg 1996;62:1010-1013.
- Guttmann L. Spinal cord injuries. Comprehensive management and research. Blackwell, Oxford 1973.
- Miller LS, Stass WE, Herbison GJ. Abdominal problems in patients with spinal cord lesions. Archives of Physical Medicine and Rehabilitation 1975; 49: 348-358.
- Martin RM, Lim AG, Kerry SM, Hilton SR. Trends in H2-receptor antagonists and proton pump inhibitors in primary care. Aliment Pharmacol Ther 1998; 12(8): 797-805.
- Kewalramani LS. Neurogenic gastroduodenal ulceration and bleeding associated with spinal cord injuries. J Trauma 1979;19: 259-265.
- Priebc HJ, Skillman JJ, Bushness LS. et al.Antacid versus cirnetidine in preventing acute gastrointestinal bleeding – a randomized trial in 75 critically ill patients. N EnglJMed 1980; 302: 426.
- Stremple JF. Mori H. Lev R. The stress ulcer syndrome. Current Problems in Surgery 1913; 4: 1-64.
- Croft DN. Cell turnover and loss and the gastric mucosal barrier. American Journal of Digestive Diseases 1977; 22 (4): 383-386.
- Wilmot CB, Walsh JJ. Abdominal emergencies in acute spinal cord injuries. Proceedings of the 19th VA Spinal Cord Injury Conference 1973; 202-205.
- Nuseiben JM. Stress ulceration in spinal injuries. In: Vinken PJ, Bruyn GW: Handbook ofclinical neurology 1976; 26. Amer. Elsevier Publishing Co. Inc., New York, 351.
- Silver JR, Morris WR, Otfinowski JS. Associated injuries in patients with spinal injury. Injury 2004; 12(3): 219-224.
- Simms HH, DeMaria E, McDonald L, et al. Role of gastric colonization in the development of pneumonia in critically ill trauma patients: results of a prospective randomized trial. J Trauma 1991; 31:531-536; discussion 536-537.
- Martin LF, Booth FV, Reines HD, et al. Stress ulcers and organ failure in intubated patients in surgical intensive care units. Ann Surg 1992; 215:332-337.
- Prod'hom G, Leuenberger P, Koerfer J, et al. Nosocomial pneumonia in mechanically ventilated patients receiving antacid, ranitidine, or sucralfate as prophylaxis for stress ulcer. A randomized controlled trial. Ann Intern Med 1994; 120:653-662.
- Chamey KJ, Jules GL, Comarr AE: General surgery problems in patients with spinal cord injuries, Arch Surg 1975; 110:1083-1088.
- Tanaka M, Uchiyama M, Kitamo M: Gastroduodenal disease in chronic spinal cord injuries. Arch Surg 1979; 114:185-187.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




