Evidence based evaluation of syncope of uncertain origin
Vinoth Sankar, Steven Close and Stephen J Leslie
Cite this article as: BJMP 2010;3(4):a340
|
|
Abstract Syncope is a common medical condition encountered in clinical practice. The pathophysiology can be complex and at times making a definitive diagnosis can be difficult. It can be associated with high rates of morbidity and mortality. Physicians’ approaches to this condition are varied and at times, due to lack of a methodical approach, potential life threatening conditions are missed. Some patients are under investigated while other patients are over investigated. This increases the already high health care costs associated with managing this condition. This article discusses an evidence based methodical approach to diagnosis and treatment of this often complex condition.
Keywords: Syncope, Collapse, Guidelines |
Introduction
Syncope is a common condition encountered in acute medical practice. Many patients with syncope are initially labelled as having “collapse query cause”. It is defined as transient loss of consciousness (T-LOC) due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery1. Incidence of syncope is difficult to determine accurately as many cases remain unreported. Some studies quote an overall incidence rate of a first report of syncope to be 6.2 per 100 person-years. Clearly this is age related and the incidence increases dramatically in patients over the age of 70 years2. Syncope accounts for 1-6% of hospital admissions and 1% of emergency department (ED) visits per year3-5. Hospital episode statistics from NHS hospitals in England reported a total of 119,781 episodes of collapse/syncope for the financial year 2008-09 which is about twice the number of episodes reported in the year 1999-2000. About 80% of patients were admitted and they have an average length of stay of 3 days accounting for over 269,245 bed days during that financial year6.
Syncope is also associated with significant mortality and morbidity if left untreated. Literature reports a 6-month mortality of 10%, which can go up to 30% if cardiac syncope is untreated7. Non-cardiac syncope is associated with a survival rate comparable to people with no syncope2. Syncope is also a risk factor for fractures related to falls especially in elderly and can cause significant morbidity in this group8. In addition, there are significant health care related costs associated with management of syncope. Cost per diagnosis can vary from over £611 in the UK to €1700 in Italy. Hospitalisation alone accounted for 75% of cost in some studies9,10. Diagnosis of this condition can be difficult especially if there is a lack of structured approach. Over the last few years this topic has attracted enormous interest and several studies have been published, aiming at improving the approach to this condition. Standardised syncope pathways improve diagnostic yield and reduced hospital admissions, resource consumption and over all costs10. Recently the task force for the diagnosis and management of syncope of the European Society of Cardiology published guidelines for the diagnosis and management of syncope1. However, in spite of the available evidence very few hospitals have standardised syncope pathways for the management of this complex condition. Only 18% of EDs have specific guidelines and access to a specialist syncope clinic11. This article focuses on evidence based structured evaluation of syncope. Current practice in the management of syncope Due to the difficulty in diagnosis and mortality associated with this condition, a cautious approach may be taken by physicians resulting in hospitalisation of majority of patients presenting with syncope. We recently audited the practice of syncope in our hospital, which is a tertiary centre in the north of Scotland. 58 patients admitted with this condition over a period of a month were included in the audit. It showed an average length of stay (LOS) of 4.76 days in these patients. Due to a lack of methodical approach and standardised pathway for management of this condition many patients were subjected to several inappropriate inpatient investigations significantly prolonging the LOS and increasing the cost. Only 7 (12%) cardiac events were observed in this group and in retrospect a good methodical approach would have predicted these events. It should be noted that even in the geriatric population, reflex syncope that carries a benign prognosis is more common than cardiac syncope2. A systematic approach to the management of syncope (Figures 1 and 2). 
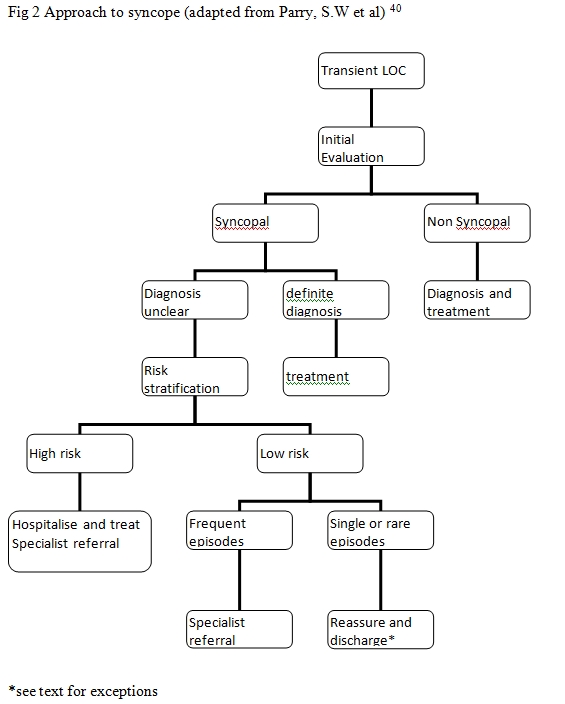 The causes of syncope can be broadly divided in to cardiac causes and non-cardiac causes (Table 1). Initial evaluation leads to a diagnosis in less than 50% patients in most instances4,12-14. If there is uncertainty about diagnosis then the patient is risk stratified. High-risk patients are hospitalised, evaluated and treated whereas early discharge could be considered in low risk patients. Aetiology of Syncope41
The causes of syncope can be broadly divided in to cardiac causes and non-cardiac causes (Table 1). Initial evaluation leads to a diagnosis in less than 50% patients in most instances4,12-14. If there is uncertainty about diagnosis then the patient is risk stratified. High-risk patients are hospitalised, evaluated and treated whereas early discharge could be considered in low risk patients. Aetiology of Syncope41
| Neurally-mediated (Reflex) Syncope | Cerebro vascular |
e.g., Micturition, post prandial, defecation, cough |
|
| Cardiac | Orthostatic |
Structural cardio-pulmonary disease
Cardiac arrhythmias
|
|
Initial evaluation (Table 2)
|
History Many patients with syncope are initially labelled as having “collapse query cause”. Loss of postural tone is termed “collapse”. Indeed, the term “collapse query cause” does not give any useful information regarding the underlying condition. A clear history from the patient and the bystander or witness (if available) is the key to the diagnosis. Firstly, determine if the collapse was associated with loss of consciousness (LOC). LOC can be transient (T-LOC) or prolonged. Categorising “collapse” is important at this stage as the aetiology and approach to each category is different (Figure 1). Secondly, establish if the collapse was syncopal. The LOC should be transient (e.g. did the patient regain consciousness in the ambulance, before or on arrival to hospital?), of rapid onset and associated with a spontaneous complete recovery. Also the mechanism should be due to transient global hypoperfusion. T-LOC secondary to other mechanisms such as trauma and brief seizures should be excluded. On occasions syncope could be associated with brief jerking movements mimicking seizures15. Also note that a transient ischemic attack (TIA), commonly listed as a differential diagnosis of syncope by physicians, is not a cause of syncope as this is not associated with global cerebral hypoperfusion. The absence of a coherent history because patient had no recollection of events and there was no witness account available can make this distinction difficult. This is also particularly difficult in the elderly with cognitive impairment. Other useful information includes whether the syncope was associated with postural change. Orthostatic hypotension occurs after standing. If present it will be useful to check drug history (new vasodepressive drugs). Features suggestive of Parkinson’s disease or amyloidosis may raise the possibility of autonomic neuropathy. A strong family history of sudden cardiac death may be of relevance. Table 3 summarises the features of neurally mediated and cardiac syncope. Table 3 Features suggesting neurally mediated and cardiac syncope42
| Neurally mediated | Cardiac |
|
|
Physical examination The next step is a thorough physical examination. This should include an ABC approach if the patient is very ill and particular attention should be given to exclude immediate life threatening conditions such as pulmonary embolism, acute myocardial infarction, life threatening arrhythmias, acute aortic dissection, seizures etc… Recording the vital signs is important as it may give a clue to diagnosis (e.g., acute hypoxia may indicate massive pulmonary embolism). Recording postural blood pressure when lying and during active standing for 3 minutes is useful to exclude orthostatic hypotension1. Recording a deficit in blood pressure in both arms may be a useful clinical finding especially if acute aortic dissection is suspected. Thorough cardio respiratory examination may reveal an obvious condition such as cardiac failure or aortic stenosis. Patients should also be examined for potential injuries as a result of syncope. Standard ECG A 12 lead ECG should be performed in all patients admitted with syncope. The abnormalities in table 4 would suggest a cardiac aetiology. The QT interval should always be measured, as it is a commonly overlooked abnormality. Blood tests Blood tests are usually unhelpful in establishing a diagnosis but can detect metabolic abnormalities such as hypoglycaemia, electrolyte abnormalities and other causes to explain LOC especially when witness account is not available. An acute drop in haemoglobin suggests blood loss. One recent study claims the usefulness of brain natriuretic peptide (BNP) for predicting adverse outcomes in syncope but it is not externally validated yet and it is too early to recommend for routine clinical practice16. Pacemaker check It is not uncommon to see a patient with a pacemaker implanted, admitted to hospital with syncope. In these circumstances, it is essential to rule out a device malfunction although this is not a common cause of syncope. A preliminary and easy test will be interrogating the pacemaker if available. This should pick up any problems with the pacemaker in most instances. With the above information establishing a diagnosis will be possible in a significant proportion of patients. Further investigations and management should be guided by the underlying diagnosis1. However in over half of patients the diagnosis may still be uncertain12,13,17. The following section explains the management of unexplained syncope. Risk stratification in patients with unexplained syncope (Tables 4 and 5) Table 4 ECG changes in ‘high-risk’ Syncope41
ECG changes favouring bradyarrhythmias
ECG changes favouring tachyarrhythmias
|
Table 5 – Clinical features of high-risk syncope1,18-23
|
When the cause of syncope is uncertain it is essential to risk stratify patients to enable appropriate treatment and further investigation. Risk stratification tools There are several scoring systems for risk stratification of syncope. Syncope Evaluation in the Emergency Department Study (SEEDS), Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL score), Evaluation of Guidelines in SYncope Study (EGSYS score), San Francisco Syncope Rule (SFSR), The Risk stratification Of Syncope in the Emergency department (ROSE) and American College of Emergency Physicians clinical policy are the popular ones and each has its own advantages and disadvantages1,16,18-23. Discussing each scoring system is beyond the scope of this article and we shall restrict the discussion to the summary of these risk stratification tools (Table 5). It will be too early to include all the factors mentioned in the ROSE study, as it is not externally validated yet. It could be argued that taking all the risk factors described may increase admission rates but this approach may at least not miss the high-risk patient. This is a developing field and more evidence is likely to be published soon. High-risk vs. low-risk syncope: A high-risk syncope patient is the one where a cardiac cause is likely and where the short-term mortality is high due to major cardiovascular events and sudden cardiac death. High-risk syncope is said to be present if any of the features in the table 4 or 5 are present. Management of low-risk syncope Patients with a single or very infrequent syncope are usually reassured and discharged, as the short-term mortality is low1,2. Tilt table test is not usually required where a single or rare episode of neurally mediated syncope is diagnosed clinically. One exceptional circumstance where single rare episodes are investigated further with a tilt table test is when there could be an occupational implication (e.g. aircraft pilot) or if there is a potential risk of physical injury. Patients with recurrent unexplained syncope need to be further investigated (see below). Management of high-risk syncope / suspected cardiac syncope High-risk patients usually require hospitalisation and inpatient evaluation. Other high-risk patients who may be considered for admission are vulnerable patients susceptible to serious injuries, for example, elderly patient or a patient with multiple co-morbidities. Further investigations (Table 6)
| Non invasive | Invasive |
|
|
* Specialist Investigation Echocardiography Echocardiography is a relatively inexpensive and non-invasive investigation. It should be performed if there is a clinical suspicion of a significant structural abnormality of heart such as ventricular dysfunction, outflow tract obstruction, obstructive cardiac tumours or thrombus, pericardial effusion etc… The yield of this test is low in the absence of clinical suspicion of structural heart disease. However in the presence of a positive cardiac history or an abnormal ECG, one study detected LV dysfunction in 27% of patients and half of these patients had syncope secondary to an arrhythmia. In patients with suspected obstructive valvular disease 40% had significant aortic stenosis as a cause of syncope24. ECG monitoring These tests have utility in identifying arrhythmogenic syncope. If a patient has syncope correlating with a significant rhythm abnormality during the monitoring period with the device, then the cause of syncope is due to the underlying rhythm abnormality. On the other hand, if no rhythm abnormality is recorded during a syncopal attack, then an underlying rhythm problem as a cause of syncope is excluded. Therefore, these tests are meaningful only if there is a symptom-rhythm correlation, which is the working principle of these devices. In the absence of syncope, during the monitoring period, these tests may pick up other abnormalities that may be relevant. For example, rapid prolonged supra-ventricular tachycardias, ventricular tachycardias, periods of high degree AV blocks (mobitz type 2 or complete heart block) or significant sinus pauses >3seconds (except during sleep, negatively chronotropic therapy and trained athletes), which will require further investigation or treatment. Telemetry Telemetry can be used in inpatients. Although the diagnostic yield of this investigation is only 16%, given the high short-term mortality, this test is indicated in the high-risk group 1. Usually patients are monitored for 24 to 48 hours although there is no agreed standard period for monitoring25. Holter monitoring This involves connecting the patient through cutaneous patch electrodes. It records the ECG activity conventionally over 24-48 hours or at times up to 7 days. It is particularly useful only in patients who have frequent regular symptoms (≥1 per week). For this reason, the yield of this test can be as low as 1-2% in unselected population1. Long inpatient waiting lists in some hospitals can significantly prolong the length of stay and cost. Selecting patients carefully for this test based on risk stratification will reduce costs and waiting lists. Carotid sinus massage This simple bedside test is indicated in patients over the age of 40 years with syncope of unexplained origin after initial evaluation. A ventricular pause lasting >3 s and/or a fall in systolic BP of >50mmHg defines carotid sinus hypersensitivity (CSH) syndrome. It is contraindicated in patients with recent cerebrovascular accidents (past 3 months) or with carotid bruit except when a Doppler study has excluded significant stenosis1. Cognition test If an elderly patient had forgotten about the events, in the absence of an obvious cause, it may be useful to test cognition. If cognitive impairment is present, common problems associated with cognitive dysfunction should be considered e.g. falls, orthostatic hypotension. Other investigations In spite of the above tests if a cause is not determined, early specialist input is recommended for further investigation and treatment. The following non-invasive and invasive investigations may be appropriate in these circumstances. An external loop recorder This is a non-invasive form of electrocardiographic monitoring. The principle is same as that of Holter monitoring. External loop recorders have a loop memory that continuously records and deletes ECG. When activated by the patient, typically after a symptom has occurred, 5 – 15 min of pre-activation ECG is stored and can be retrieved for analysis. Studies have shown that they have increased diagnostic yield compared to Holter1. They should be considered in patients who have symptoms on a monthly basis. A Tilt table test This is indicated in cases of recurrent unexplained syncope after relevant cardiac causes of syncope are excluded and a negative Carotid sinus massage performed in the absence of contraindications. It is also indicated when it is of clinical value to demonstrate patients susceptibility to reflex syncope and thereby to initiate treatment. Other less common indications are recurrent unexplained falls, differentiate jerking movements secondary to syncope and epilepsy, diagnose psychogenic pseudo syncope and differentiate orthostatic and reflex syncope. Indication of this test in the context of a single unexplained syncope is discussed above. Ambulatory blood pressure monitoring This may be useful in patients with unexplained syncope particularly in old age to check if there is an element of autonomic failure and if a single set of orthostatic blood pressure recording is not helpful. In one study, it has been shown that 25% of the elderly patients admitted with falls or syncope had postprandial hypotension especially after breakfast26. It may be more readily available than a tilt table test in some centres. Exercise stress test This may be useful in a rare entity called exercise induced syncope. Outflow tract obstruction should be excluded by echocardiography before subjecting a patient to this test especially in the presence of relevant signs. However there is no evidence for supporting this test in investigating syncope in general population. Implantable loop recorders These are implanted subcutaneously. It needs to be activated either by the patient or a bystander after a syncopal attack. It is indicated in high-risk patients where a comprehensive evaluation did not establish an underlying diagnosis. In the absence of high risk factors, it is also indicated in patients with recurrent unexplained syncope especially if infrequent. Conventionally it is used as a last resort in patients with recurrent unexplained syncope as the initial costs are high. It has been shown in one study to be more cost effective than the conventional strategy and was more likely to provide a diagnosis in patients with recurrent unexplained syncope27. However patients with poor LV function and those at high risk of life-threatening arrhythmias were excluded from this study. Coronary angiography or CT coronary angiography This may be helpful in suspected myocardial ischemia or ischemia related arrhythmias. Electrophysiological study may be considered in certain circumstances by cardiologists. When a standardised pathway is used, diagnosis is ascertained in 21% patients on initial evaluation and further 61% patients with early investigations. Only in 18% patients the diagnosis was still uncertain12. Other studies have shown similar results28. Although these results are from a dedicated syncope unit following a standardised pathway, these could be extrapolated to any unit following these standardised pathways. Further management is dictated by the underlying diagnosis with early specialist input for appropriate treatment. Treatments Single or rare episodes of reflex syncope do not require treatment. However, recurrent troublesome reflex syncope may warrant treatment. Treatment modalities are primarily non-pharmacological such as tilt training, physical counter pressure manoeuvres (leg crossing, hand gripping) and ensuring adequate hydration29. If refractory to non-pharmacologic measures midodrine (alpha agonist) may be considered in patients with frequent hypotensive symptoms30,31. Fludrocortisone may be used in elderly but there is no trial evidence to support this. Betablockers have been presumed to lessen symptoms but are shown to be ineffective in several studies 32. They may potentially exacerbate bradycardia in carotid sinus syncope and are not recommended in treatment of reflex syncope. Treatment with cardiac pacing in reflex syncope is controversial and may be considered in patients with predominant cardio inhibitory response on carotid sinus massage (in CSH syndrome) or on tilt test (in reflex syncope). It should be noted that cardiac pacing has no effect on the often-dominant vasodepressor component of reflex syncope. In patients with orthostatic hypotension, non-pharmacologic measures like increased salt and water intake, head up tilt sleeping, physical counter pressure manoeuvres, abdominal binders and compression stockings may help reducing symptoms. Midodrine is an efficient alternative in these circumstances and fludrocortisone also can be used.33,34Syncope secondary to cardiac arrhythmias needs treatment if a causal relationship is established. Potential reversible causes such as electrolyte abnormalities and drug induced causes should be excluded. Cardiac pacing is a modality of treatment in significant bradyarrhythmias secondary to sinus node or advanced AV nodal disease such as mobitz type 2 block, complete heart block or tri-fascicular block. Catheter ablation and anti-arrhythmic drug therapy are the main modalities of treatment for tachyarrhythmias. Implantable cardioverter defibrillator may be indicated in patients susceptible to malignant ventricular tachyarrhythmias. Treatment of syncope secondary to structural cardio pulmonary abnormality will need surgical intervention if possible. Driving and Syncope Doctors are poor at addressing and documenting this issue35. Table 7 gives some useful information from the DVLA website (http://www.dft.gov.uk/dvla/medical/ataglance)36. This information is country specific and subject to change. Table 7 – Driving and Syncope in the UK36
| Type of Syncope | Group 1 entitlement (car, motorcycle etc.,) | Group 2 entitlement (Large goods vehicle, passenger carrying vehicle) |
| Simple faint | No restrictions | No restrictions |
| Unexplained syncope with low risk of recurrence* | Allowed to drive 1 month after the event | Allowed to drive 3 months after the event |
| Unexplained syncope with high risk of recurrence** and cause identified and treated | Allowed to drive 1 month after the event | Allowed to drive 3 months after the event |
| Unexplained syncope with high risk of recurrence** and cause not identified | Licence is refused or revoked for 6 months | Licence is refused or revoked for 12 months |
*Absent clinical evidence of structural heart disease and normal ECG** Abnormal ECG, clinical evidence of structural heart disease, syncope causing injury, recurrent syncope Syncope unitsSyncope units aim to evaluate syncope (and related conditions) in dedicated units consisting of generalists and specialists with an interest in syncope. A sufficient number of patients are required to justify such a unit. They are well equipped with facilities for recording ECG, blood pressures, tilt table, autonomic function testing, ambulatory blood pressure monitoring, and invasive and non-invasive electrocardiographic monitoring. It has been shown to be cost effective and reduces health care delivery costs by reducing admission rates, readmission rates and event rates. Examples include the Newcastle model, Manchester model and the Italian model.12,18,37,38 Conclusions The incidence of syncope is increasing in the UK with an aging population. There is significant cost incurred in the delivery of health care for this condition. The approach to syncope varies widely amongst practising physicians due to lack of a methodical approach. A thorough initial evaluation yields a diagnosis in less than half of the patients. When the cause of syncope remains unexplained after initial evaluation, the patients should be risk stratified. While a patient with a single episode of low risk syncope can be reassured and discharged, those with high-risk features should be hospitalised for further management. Outpatient evaluation could be offered for low risk patients if recurrent. Early specialist input should be sought in high-risk syncope and recurrent unexplained syncope. This standardised approach or pathway will reduce cost by reducing hospitalisation, inappropriate investigations and length of stay.
Key Facts
|
Future Interests Syncope had been known for several decades and still remains a complex condition, as the exact mechanisms are poorly understood especially in non-cardiac syncope. Mechanism of syncope in the elderly patients may be different from those of young patients and studies should focus in understanding the mechanics. Further research is needed in risk stratifying syncope. It may enable us to develop more robust care pathways for management of syncope. The role of BNP in investigating and risk stratifying syncope need to be further clarified. In spite of sophisticated tests the cause of syncope in a proportion of patients remain uncertain. Studies should focus on the long-term outcome and management of syncope in this group. The role of implantable loop recorder in the investigation of syncope should be better defined and more studies should focus on when it should be offered in the pathway of management of syncope. Studies are also required to develop effective pharmacotherapies for this condition.
|
Acknowledgements Dr Robert Peel FRCP (Edin), Consultant Physician and Nephrologist, Raigmore Hospital, Inverness, UK Competing Interests None declared Author Details VINOTH SANKAR, MBBS, MRCP.Specialty Registrar, Acute Medicine,Ward 49, Aberdeen Royal Infirmary, Aberdeen, UK STEVEN CLOSE,MBChB, MRCP,Consultant and Clinical Lead Acute Medicine Aberdeen Royal Infirmary, Aberdeen, UK STEPHEN J LESLIE, BSc, MBChB, FRCP (Edin), PhD Consultant Cardiologist, Raigmore Hospital, Old Perth Road, Inverness,Highland Campus, University of Stirling, Centre for Health Science, Inverness, UK CORRESPONDENCE: Vinoth Sankar, MBBS, MRCP. Specialty Registrar, Acute Medicine, Ward 49, Aberdeen Royal Infirmary, Aberdeen, UK Email: vinothsankar@nhs.net |
References
(1) European Heart Rhythm Association (EHRA), Heart Failure Association (HFA), Heart Rhythm Society (HRS), European Society of Emergency Medicine (EuSEM), European Federation of Internal Medicine (EFIM), European Union Geriatric Medicine Society (EUGMS), et al. Guidelines for the diagnosis and management of syncope (version 2009): the Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). Eur.Heart J. 2009 Nov;30(21):2631-2671.(2) Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N.Engl.J.Med. 2002 Sep 19;347(12):878-885.(3) Martin GJ, Adams SL, Martin HG, et al. Prospective evaluation of syncope. Ann.Emerg.Med. 1984 Jul;13(7):499-504.(4) Kapoor WN. Evaluation and outcome of patients with syncope. Medicine (Baltimore) 1990 May;69(3):160-175.(5) Kapoor WN. Diagnostic evaluation of syncope. Am.J.Med. 1991 Jan;90(1):91-106.(6) hospital episode statistics. Available at: http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=203.(7) Kapoor WN, Karpf M, Wieand S, et al. A prospective evaluation and follow-up of patients with syncope. N.Engl.J.Med. 1983 Jul 28;309(4):197-204.(8) Campbell AJ, Reinken J, Allan BC, et al. Falls in old age: a study of frequency and related clinical factors. Age Ageing 1981 Nov;10(4):264-270.(9) Farwell DJ, Sulke AN. Does the use of a syncope diagnostic protocol improve the investigation and management of syncope? Heart 2004;90:52-58.(10) Brignole M, Ungar A, Bartoletti A, et al. Standardized-care pathway vs. usual management of syncope patients presenting as emergencies at general hospitals. Europace 2006 Aug;8(8):644-650.(11) Stockley CJ, Bonney ME, Gray AJ, et al. Syncope management in the UK and Republic of Ireland. Emerg.Med.J. 2009 May;26(5):331-333.(12) Brignole M, Ungar A, Casagranda I, et al. Prospective multicentre systematic guideline-based management of patients referred to the Syncope Units of general hospitals. Europace 2010 Jan;12(1):109-118.(13) Kapoor WN. Evaluation and management of the patient with syncope. JAMA 1992 Nov 11;268(18):2553-2560.(14) Crane SD. Risk stratification of patients with syncope in an accident and emergency department. Emerg.Med.J. 2002 Jan;19(1):23-27.(15) Song PS, Kim JS, Park J, Yim HR, et al. Seizure-like activities during head-up tilt test-induced syncope. Yonsei Med.J. 2010 Jan 31;51(1):77-81.(16) Reed MJ, Newby DE, Coull AJ, et al. The ROSE (risk stratification of syncope in the emergency department) study. J.Am.Coll.Cardiol. 2010 Feb 23;55(8):713-721.(17) Croci F, Brignole M, Alboni P, et al. The application of a standardized strategy of evaluation in patients with syncope referred to three syncope units. Europace 2002 Oct;4(4):351-355.(18) Shen WK, Decker WW, Smars PA, et al. Syncope Evaluation in the Emergency Department Study (SEEDS): a multidisciplinary approach to syncope management. Circulation 2004 Dec 14;110(24):3636-3645.(19) Colivicchi F, Ammirati F, Melina D, et al. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur.Heart J. 2003 May;24(9):811-819.(20) Del Rosso A, Ungar A, Maggi R, et al. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: the EGSYS score. Heart 2008 Dec;94(12):1620-1626.(21) Quinn J, McDermott D, Stiell I, et al. Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann.Emerg.Med. 2006 May;47(5):448-454.(22) Huff JS, Decker WW, Quinn JV, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Ann.Emerg.Med. 2007 Apr;49(4):431-444.(23) Suzuki M, Hori S, Aikawa N. Application of the recent American practice resources for risk stratification system for patients presenting to a Japanese emergency department because of syncope. Int.Heart J. 2007 Jul;48(4):513-522.(24) Sarasin FP, Junod AF, Carballo D, et al. Role of echocardiography in the evaluation of syncope: a prospective study. Heart 2002 Oct;88(4):363-367.(25) Bass EB, Curtiss EI, Arena VC, et al. The duration of Holter monitoring in patients with syncope. Is 24 hours enough? Arch.Intern.Med. 1990 May;150(5):1073-1078.(26) Puisieux F, Bulckaen H, Fauchais AL, et al. Ambulatory blood pressure monitoring and postprandial hypotension in elderly persons with falls or syncopes. J.Gerontol.A Biol.Sci.Med.Sci. 2000 Sep;55(9):M535-40.(27) Krahn AD, Klein GJ, Yee R, et al. Cost implications of testing strategy in patients with syncope: randomized assessment of syncope trial. J.Am.Coll.Cardiol. 2003 Aug 6;42(3):495-501.(28) Fedorowski A, Burri P, Juul-Moller S, et al. A dedicated investigation unit improves management of syncopal attacks (Syncope Study of Unselected Population in Malmo--SYSTEMA I). Europace 2010 May 27.(29) van Dijk N, Quartieri F, Blanc JJ, et al. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial). J.Am.Coll.Cardiol. 2006 Oct 17;48(8):1652-1657.(30) Perez-Lugones A, Schweikert R, Pavia S, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J.Cardiovasc.Electrophysiol. 2001 Aug;12(8):935-938.(31) Samniah N, Sakaguchi S, Lurie KG, et al.. Efficacy and safety of midodrine hydrochloride in patients with refractory vasovagal syncope. Am.J.Cardiol. 2001 Jul 1;88(1):A7, 80-3.(32) Sheldon R, Connolly S, Rose S, et al. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006 Mar 7;113(9):1164-1170.(33) Low PA, Gilden JL, Freeman R, et al. Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. A randomized, double-blind multicenter study. Midodrine Study Group. JAMA 1997 Apr 2;277(13):1046-1051.(34) van Lieshout JJ, ten Harkel AD, Wieling W. Fludrocortisone and sleeping in the head-up position limit the postural decrease in cardiac output in autonomic failure. Clin.Auton.Res. 2000 Feb;10(1):35-42.(35) Brooke BT, Southward RD. An audit of advice on fitness to drive during accident and emergency department attendance. Emerg.Med.J. 2006 Feb;23(2):103-104.(36) For Medical Practitioners - At a glance guide to the current medical standards of fitness to drive - issued by Drivers Medical Group, DVLA Swansea, Feb 2010; Available at: http://www.dft.gov.uk/dvla/medical/ataglance.aspx?keywords=fitness+to+drive.(37) Parry SW, Frearson R, Steen N, Newton JL, et al. Evidence-based algorithms and the management of falls and syncope presenting to acute medical services. Clin.Med. 2008 Apr;8(2):157-162.(38) Petkar S, Cooper P, Fitzpatrick AP. How to avoid a misdiagnosis in patients presenting with transient loss of consciousness. Postgrad.Med.J. 2006 Oct;82(972):630-641.(39) Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med.Clin.North Am. 2006 Sep;90(5):807-824.(40) Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ 2010 Feb 19;340:c880.(41) Brignole M, Alboni P, Benditt DG, et al. Guidelines on management (diagnosis and treatment) of syncope-update 2004. Executive Summary. Eur.Heart J. 2004 Nov;25(22):2054-2072.(42) The European Society of Cardiology Guidelines for the diagnosis and management of syncope reviewed by Angel Moya, MD, FESC, Chair of the Guideline Taskforce with J. Taylor, MPhil. Eur.Heart J. 2009 Nov;30(21):2539-2540.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




