Evidence and recovery; improving outcomes in opiate substitution treatment
James Bell, Christine Healey, Fiona Kennedy, Mohammad Faizal and Aadil Jan Shah
Cite this article as: BJMP 2013;6(1):a601
|
|
Abstract Background: Based on the perception that many patients on methadone are not receiving effective treatment, drug policy in the UK is being reoriented towards the ‘recovery agenda’1. Aim: To assess the extent to which current delivery of OST is evidence-based, and whether bringing treatment into line with evidence improves outcomes. Method: Clinical audit in two OST services in Merseyside. Non-responding patients - those reporting regular heroin use in treatment - were identified from files, and patients in one service were referred for medical review to bring their treatment into line with current UK guidelines2 – predominantly, ensuring adequate methadone doses. Patients in the other clinic continued to receive treatment as usual. Files were re-audited 9 months later and rates of heroin use between the clinics compared. Results: 175 (17% of patients in treatment) reported regular heroin use; most were on less than 60mg/day of methadone. Although reporting high depression scores and low quality of life, patients resisted changes to their treatment; of 104 patients referred for medical review, only 47 attended. Medical review and changes to treatment were seen as an intrusion into patients’ choices. At follow up audit, there was no difference in reductions in heroin use between the two OST services. Conclusion: Many non-responders appeared “stuck”, but resisted change. The clinical ethos was oriented towards supporting clients in their choices rather than achieving specific treatment objectives. By focusing on outcomes rather than process, the ‘recovery agenda’ may facilitate the implementation of evidence based care, as opposed to being a competing paradigm. Keywords: opiate substitution treatment, recovery agenda, optimisation clinic, audit, evidence-based care. |
Introduction
Driven by a global rise in opioid dependence, Opioid Substitution Treatment (OST), the prescribing of opioids (usually methadone or buprenorphine) as maintenance treatment, has expanded worldwide over the last two decades3. Participation in OST reduces the risk of death by overdose4, reduces the risk of HIV transmission5 and reduces participants’ involvement in property crime6. For these reasons, maintenance with methadone remains the major public health response to reduce the harms caused by heroin addiction.
In the United Kingdom (UK) in the late 1990s, government funding to expand access to OST was provided, with the explicit objective of reducing crime7. The expansion of treatment was supported with clinical guidelines2, and targets were set to try to ensure good outcomes. Given the research evidence on the importance of retention in producing better outcomes, service providers were set a target of retaining at least 75% of people in treatment for 3 months. A tool to monitor outcomes, the Treatment Outcomes Profile (TOP)8, was developed and service providers nationally were set a target of 80% of people in OST completing TOP at entry and after 6 months9. This 20-item self-report questionnaire records a set of core data for the previous 28 days, including the number of days on which heroin and cocaine have been used.
The amount of methadone prescribed in England and Scotland increased fourfold over the decade 1998 – 20083. However, in 2010, Britain’s newly-elected government signalled a change in the direction of drug policy1. The paradigm on which the new policy is based is “recovery”, a concept embracing self-help, mutual support, and optimism about the possibility of positive change. The policy is in part driven by the perception that treatment services have a defeatist attitude, expecting little positive change – hence the claim that there are too many patients “parked on methadone”. To counteract this perceived pessimism, the “recovery agenda” includes incentives to services to promote abstinence from all drugs including prescribed OST medication. This policy has been criticized as being inconsistent with the available evidence10, but has been defended on the grounds that many patients on methadone were doing poorly, and needed encouragement to make positive changes in their lives.
In 2010, we decided to investigate to what extent people were responding poorly to treatment, and whether this could be improved by implementation of evidence-based treatment.
Methods
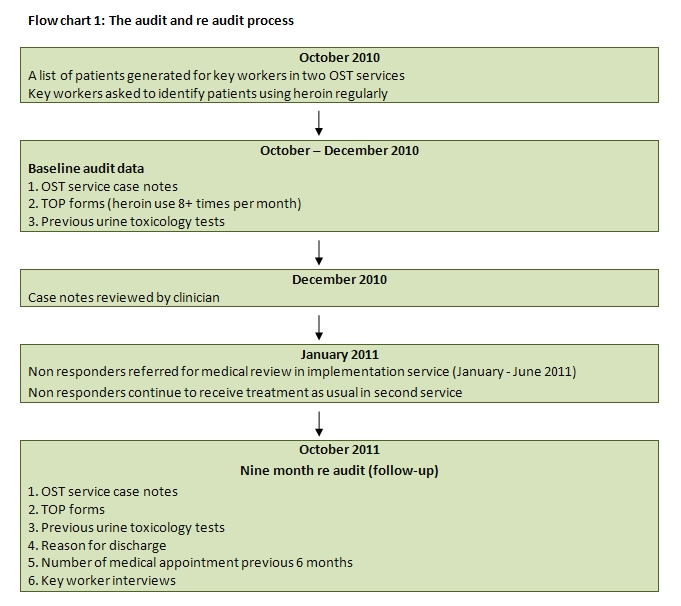
This quality improvement project was undertaken in two OST clinics in Merseyside, managing in total over 1000 patients. The services had the same senior leadership and medical staff, but separate teams of nurses and key workers. Supervised administration was provided by local retail pharmacies.
In October 2010 key workers were provided with list of patients currently under their care and asked to identify patients they thought were using heroin regularly. A research assistant then checked case notes of identified patients, looking at self-reported heroin use as recorded in TOP monitoring forms, and at the results of previous urine toxicology tests. Those whose most recent TOP was performed at entry to treatment were excluded (since their self-reported heroin use covered a time when they were not in treatment). Among the remainder patients reporting use of heroin on at least 8 days in the 4 weeks preceding their last TOP interview were classified as “non-responding” patients. The case notes of all identified “non-responders” were reviewed using an audit tool covering age, sex, postcode, date of entry into treatment, duration of treatment, dose of medications, extent of supervised administration, dates and results of recent urine toxicology, and date and self-reported drug use from previous TOP questionnaires. This data was collected at baseline and again at re-audit (follow-up) 9 months later.
Postcodes were used to derive Index of Multiple Deprivation (IMD) scores11. The English index of multiple deprivation (IMD) is a measure of multiple deprivations, with domains including employment deprivation, health deprivation and disability, education skills and training deprivation, barriers to housing and services, living environment deprivation, and crime.
In one clinic, the “implementation clinic”, beginning January 2011, key workers were asked to refer all non-responders for a medical review. Patients were also screened for comorbidity, taking advantage of a separate project running concurrently which was designed to test the psychometric properties of a new questionnaire on mental health and well-being. All service users at the implementation clinic were invited to take part. The study had National Research Ethics approval and approval from the Merseycare NHS Trust R&D Office. Quality of life was assessed with the EQD12 which comprises 5 domains measuring health-related quality of life: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Depression was screened for with the Beck Depression Inventory13.
UK guidelines recommend for patients doing poorly “..ensuring medication is provided within evidence-based optimal levels, changing to another substitute medication, increasing key working or psychosocial interventions and increasing supervised consumption” 3. The recommended dosage for effective treatment is listed as in the range 60-120mg/day of methadone. At medical review, the plan was for the doctor to assess the non-responding patients, and propose raising methadone dose progressively until heroin use ceased, or a maximum dose of 120mg/day was reached; and requiring supervised consumption of methadone for patients persisting in heroin use.
Establishing the medical reviews in one of the two clinics was necessary for logistic reasons, but it also allowed an opportunity to assess the impact of the reviews, by comparing the outcomes of non-responders in the two clinics. If effective, it was proposed to extend this approach to the second ‘treatment as usual’ service. Referrals for medical review ceased in June 2011, and over the next three months staff feedback about the process was sought. In October 2011 a repeat audit of case notes including TOP results of all previously identified non-responders at both services was undertaken.
At follow-up data on the frequency of medical appointments in the preceding 6 months were also collected. In cases where people had left treatment, the TOP performed on exit from treatment was used. Those non-responders who had left treatment were identified and tabulated according to the reason for leaving treatment.
Flowchart 1: The audit and re-audit process
Ethics
The audit was approved by the local NHS Trust R&D Office. Funding was obtained to undertake the work by Mersey Care NHS Trust.
Analysis
Data was entered into SPSS version 18 (for windows). Summary statistics and standard hypothesis tests compared non responders in the intervention service to non responders in treatment as usual to ensure there were no statistically significant differences between the two groups at baseline. Chi-square and t-tests compared age, sex distribution, IMD scores, methadone dose and months in treatment this episode. Mann-Whitney U tests compared the number of TOP forms completed in each group during the previous 6 and 12 months. Regression analysis explored whether there was a relationship between attendance for supervised administration, self-reported quality of life and depression for non responders in the implementation group. Differences in baseline and at 9 month re audit methadone dose and heroin use were tabulated for each group. Mann-Whitney U-tests compared any differences between the two groups. Differences within each group were also compared using the Wilcoxon signed ranks test.
Results
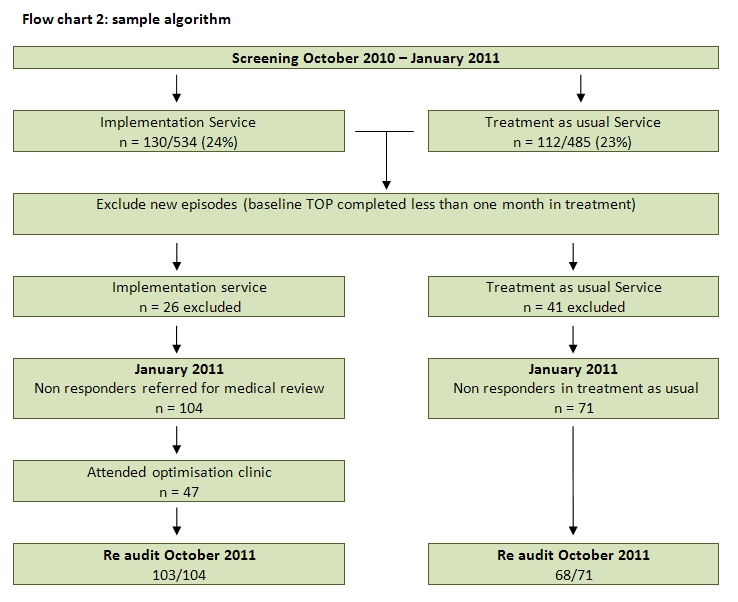
The implementation service managed 534 patients, of whom 130 (24%) were initially identified as non-responders, reporting heroin use on 8 or more days in the previous month at their last TOP interview. At the TAU service there were 485 patients, of whom 112 (23%) were identified as non-responders. Of the 242 non-responders in total, 67 (28%) were new to treatment, and were excluded. This is illustrated in the flowchart 2.
Flowchart 2: Sample Algorithm
Approximately 50% of the non-responders in each group reported daily heroin use at baseline. The two groups of non-responders did not differ significantly in terms of age, sex distribution, nor on the Index of Multiple deprivation scores (mean of 62 reflecting very severe social exclusion across both groups). Non responders in the implementation service had been in treatment a median of 18 months compared to 17 months for those in treatment as usual. Urine testing was performed infrequently in both services, but a result was available from the six months prior to baseline for 133 of the remaining 175 subjects. The urine tests results were broadly consistent with the patients self-report. Aspects of treatment at the two services differed, as shown in Table 1. At baseline, doses did not differ significantly, but the treatment as usual group was significantly less likely to have their methadone administration supervised, and had less frequent TOP monitoring.
Table 1 Profile of non-responders and their treatment at baseline
| Implementation | TAU | Total | |
| N | 104 | 71 | 175 |
| Mean age in years (min, max) | 42 (25,66) | 43 (23,63) | 42 (23,66) |
| Male (%) | 65 (63%) | 48 (68%) | 113 (65%) |
| Mean IMD Score (SD) | 62 (14.6) | 62 (14.7) | 62 (14.7) |
| Mean methadone dose in mg (SD) | 60 (17.8) | 60 (21.3) | 60 (20.3) |
| Median Months in this Rx episode (IQR) | 18 (20) | 17 (10) | 18 (14) |
| Any supervised doses | 56 (54%) | 22 (31%)* | 78 (45%) |
| Last TOPS > 6/12 ago | 15 (15%) | 29 (42%)** | 44 (25%) |
| *Pearson Chi square 9.995, df=2, p=0.007 **Mann-Whitney U =2654, p=0.002 | |||
Despite almost all non-responders being booked in for an appointment and given reminders at the implementation service, only 47 (45%) of the 104 identified attended at least one medical review. Keyworkers commented that the main reason for non-attendance was that clients were quite happy continuing heroin use and did not see stopping as something they wanted to do. When patients were told they would only receive their prescription renewal after attending, some patients chose to go without methadone and make contact a few days later, rather than attend an appointment. Among those who did attend, there was frequently resistance to increasing their methadone dose, and anger at the suggestion that medication administration should be supervised. Word of mouth spread through the service that doctors were proposing dose increases and more supervision. This increased resistance among patients, and appears to have generated some resistance among keyworkers, some of whom saw their role as advocates for the patients.
The attempt to implement change in one clinic appears to have had small effects in increasing average doses there, and having more patients seen by a doctor. Between baseline and 9 month re-audit (follow-up), mean methadone doses increased in the implementation group and fell in the TAU group, as shown in Table 2. There was a small and statistically significant increase in methadone dose in the implementation group compared to the TAU group. The difference in change in methadone dose between the two groups was statistically significant (Mann-Whitney U= 2745, p=0.002), but the mean dose increase (3mg) in the implementation group was small. In the 6 months prior to the collection of follow-up data, medical reviews in both services were infrequent; 36% of patients in the implementation group and 66% of patients in the TAU group had not seen a doctor in their OST service (Chi square =13.38, df=1, p=0.001).
In both groups, the reductions in heroin use over time were statistically significant (Wilcoxon signed ranks test p = <0.05), but the change in heroin use over time did not differ significantly between the two services (Mann-Whitney U 2832.5, p=0.7). The changes from baseline audit to 9 month re audit are shown in Table 2. Among the 47 patients who attended a medical review, the mean prescribed methadone dose rose from 58 to 66mg/day, but the number receiving supervised doses actually fell, from 23 at baseline to 20 at follow-up. Mean days of reported heroin use fell from 20 to 12 (6 patients reported abstinence) – changes almost identical to what was observed in the TAU group.
Table 2 Changes in dose and heroin use between baseline (T1) and follow-up/re audit (T2)
| Implementation | TAU | |||
| Time 1 | Time 2 | Time 1 | Time 2 | |
| N | 104 | 103 | 71 | 68 |
| Mean Self-report heroin days/28 (SD) | 19.9 (8.6) | 13.4 (10.8) | 19.6 (8.3) | 11.7 (10.8) |
| Reported daily heroin use | 52 (50%) | 33 (32%) | 25 (42%) | 17 (25%) |
| Heroin abstinence | - | 14 (14%) | - | 15 (22%) |
| Urine test positive morphine % | 88% | 76% | 85% | 70% |
| Mean daily methadone dose | 59.5 | 62.9 | 60.1 | 57 |
| Proportion self-report cocaine | 67% | 54% | 53% | 44% |
| Urine test cocaine positive | 66% | 57% | 58% | 45% |
29 non responders (28%) from the implementation service, and 27 (38%) from the TAU service had left the service between baseline and 9 month re audit. Most discharges (31/56) were transfers to another service as part of a local policy to move more people into treatment in primary care. Eight patients from the Implementation service dropped out of treatment, and 4 patients from the TAU service did so. Differences in the pattern of leaving the two services did not approach significance.
Table 3 Reason for discharge
| Reason | Implementation | TAU | Total |
| Transfer of Rx | 13 | 17 | 30 |
| Did not attend (DNA) | 8 (28%) | 4 (15%) | 12 |
| Elective Withdrawal | 3 | 3 | 6 |
| Deceased | 2 | 0 | 2 |
| Prison/drug diversion program | 3 | 3 | 6 |
| Total | 29 | 27 | 56 |
44 non responders who attended a medical review at the implementaion service completed questionnaires on health, quality of life, and depression. Ninety-six percent were not in education, employment or training (NEET). On the Beck Depression Inventory, 50% of respondents reported depression in the moderate to severe range. Regression analysis indicated that having to attend for supervised doses was associated with less depression measured on the BDI (r=-.332, p=0.039), and with better quality of life in terms of EDQ scale of self-care (r=-.598, p<0.001) and being able to undertake usual activities (r=-.605, p<0.001).
Discussion
Many people persisting in heroin use were receiving care that was out of line with guidelines – doses below 60mg, often with no supervised doses, and seldom attending for medical reviews. However, the attempt to systematically implement guidelines was not effective. Most patients did not attend, and many of those who did attend resisted changes. Although patients who attended received slightly higher doses, changes in heroin use in the subset who actually attended for review were no different to the changes observed in the TAU group.
Higher methadone doses, and patients having control over their doses, have been shown in a meta-analysis to be independently predictive of better outcomes14. One possible explanation for the failure to implement guidelines is that it may have been perceived as challenging clients’ control over their treatment. If so, it was a challenge easily defeated. Patients clearly had substantial control over their treatment, choosing whether to attend appointments, whether to accept higher doses, and whether to accept supervised doses. However, this degree of control over their treatment did not appear to be beneficial. “Non-responders” reported depression, disability and a poor quality of life.
Guidelines need to move beyond systematic reviews of effectiveness, to include evidence about implementing evidence in a real world setting15. Our conclusion is that the failure to implement guidelines was that the approach adopted was not congruent with clinic culture, which emphasised “support” rather than “structure”. “Structure” refers to both cognitive and behavioural elements of treatment. The cognitive elements are defined and agreed objectives, a sense of the direction and purpose of treatment. In all areas of mental health, clinical interactions are most useful if focused on specific performance goals related to the patient’s circumstances16. In the OST services studied, there appeared to be a focus on process and on supporting patients, rather than achieving outcomes.
Structure also includes behavioural elements - expectations and rules regarding attendance, and daily attendance for supervised administration. Interviews with UK patients in OST have indicated that they understand and value the role of supervision, not only in minimizing diversion and misuse, but in providing an activity for many people without social roles17. Consistent with the benefits of supervision, in the current audit more supervision was associated with less depression and less-poor quality of life.
This audit had several limitations. It did not attempt to measure the proportion of patients responding poorly to long-term methadone treatment, and it is possible that the true proportion may be higher than the 17% identified by key workers. Documentation of treatment outcomes, using TOP reports and UDS results, was unsystematic, limiting the number of patients in whom complete data was available. “Non-responders” self-reported heroin use to keyworkers, who administered the TOP questionnaire, and there may have been under-reporting. However, while this study may not have identified all non-responding patients, this does not invalidate the observation that attempting to implement guidelines was not successful.
Most importantly, the observations from these clinics may not be generalisable to other treatment settings. However, certain key data are available suggesting the treatment and outcomes observed in this study were not atypical. A report on national TOP monitoring noted patchy availability of follow-up data, and confirmed a high rate of persisting heroin use in treatment, with 38% of participants reporting abstinence from heroin18. Despite this high rate of heroin use, a recent survey reported a mean dose of 56mg of methadone in a national survey19. In this regard, the clinics in this report thus seem representative.
Medical staff appeared to have a peripheral role in delivery of OST in these clinics. Most non-responders did not have a medical review in 6 months – despite persisting heroin use, and self-reported depression. In the 1980s in the US, methadone treatment underwent a process labelled “demedicalisation”, marginalisation of the role of medical practitioners, and a loss of the sense that methadone was a medical treatment with clearly defined objectives and guidelines20. This contributed to a situation in which much methadone treatment in the US was out of line with research evidence21. The current audit suggests that a similar process of demedicalisation and deviation from evidence-based treatment has been occurring in some NHS services in the UK.
If these observations are representative of at least some treatment culture in the UK, they lend support to the criticisms made of methadone treatment in the new UK drug strategy1. To the extent that the recovery agenda challenges clinic culture and shifts the focus of treatment onto outcomes, it is a positive development.
However, many well-intentioned policies have unintended consequences, and there are well-based fears that the new policy promoting abstinence from OST as an objective of recovery will lead to an increase in overdose deaths3. This is specifically because of the risk of overdose deaths after leaving treatment. The reason for the increased risk of overdose after leaving treatment is that newly abstinent addicts who have reduced opioid tolerance, and a dose of heroin they previously used during periods of addiction becomes a potentially fatal dose once they are abstinent. This risk attaches to all forms of drug free treatment, as well as to patients who have left methadone. The critical issue is that lapses to heroin use, and relapses to dependent heroin use, are very common among newly-abstinent addicts. It is the high probability of relapse to heroin use which is the basis of long-term maintenance treatment – better to keep people safe and functioning normally, albeit while still taking a medication, than the risk of relapse and re-addiction, or relapse and fatal overdose. In the UK, implementation of the recovery agenda has included incentives to abstinence, and this is not consistent with evidence about the risk of relapse. If the recovery agenda can accommodate the evidence that indefinite maintenance as a valid option for many, perhaps most heroin users, then the evidence of this study is that far from being in contradiction, the recovery agenda may facilitate the implementation of evidence-based practice.
|
Acknowledgements Dr Faizal, Ms Healey and Dr Bell devised the study and supervised conduct of it. Ms Kennedy undertook data collection and with Ms Healey, data analysis. Dr Shah and Dr Faizal delivered clinical care, and Dr Shah assisted in data collection. Dr Bell wrote the paper. All authors commented on and edited the manuscript, and approved the final draft. Dr Bell has received research support and support to attend conferences from Reckittbenckiser PLC, and has received consultancy services for Reckittbenckiser. Dr Faizal has received support from Reckittbenckiser to attend a conference. Financial support for this project came from Merseycare NHS Trust. Apart from this, all authors have received no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work. Competing Interests Funding for this project was provided by Mersey Care NHS Trust. Author Details JAMES BELL, BA(Hons), MD, FRACP, FAChAM, South London and Maudsley NHS Foundation Trust, UK. CHRISTINE HEALEY BA (Hons), DipSW, MSc, MPhil, University of Liverpool, UK. FIONA KENNEDY BA (Hons), University of Liverpool, UK. MOHAMMAD FAIZAL, MBBS, MRCPsych, MBA, Clinical Director, Addictions, MerseyCare NHS Trust, UK. AADIL JAN SHAH, MBBs, MSc, MRCPsych, Consultant Psychiatrist, Cheshire and Wirral Partnership NHS Foundation Trust, UK. CORRESPONDENCE: DR JAMES BELL, 63-65 Denmark Hill, London SE5 8RS, UK. Email: James.bell@kcl.ac.uk |
References
- HM Government (2010) 'Drug Strategy 2010: Reducing demand, restricting supply, building recovery: supporting people to live a drug free life', in HM Government (ed.), (London).
- Department of Health (2007), 'Drug Misuse and Dependence: UK Guidelines on Clinical Management', in Department of Health (ed.), (London).
- Strang J, Hall W, Hickman M, et al (2010), 'Impact of supervision of methadone consumption on deaths related to methadone overdose (1993-2008): analyses using OD4 index in England and Scotland', BMJ, 341.
- Clausen T, Anchersen K, and Waal H (2008), 'Mortality prior to, during and after opioid maintenance treatment (OMT): A national prospective cross-registry study', Drug and Alcohol Dependence, 94 (1–3), 151-57
- Jürgens R, Ball A, and Verster, A (2009), 'Interventions to reduce HIV transmission related to injecting drug use in prison', The Lancet Infectious Diseases, 9 (1), 57-66
- Moffatt, S., Weatherburn, D., Donnelly, N. (2005), 'What caused the recent drop in property crime?' Crime and Justice Bulletin, 85.
- Duke, K (2006), 'Out of crime and into treatment? The criminalization of contemporary drug policy since tackling drugs together', Drugs: Education, Prevention & Policy, 13 (5), 409-15.
- Marsden, J, et al. (2008), 'Development of the treatment outcomes profile', Addiction, 103 (9), 1450-60
- 9 National Treatment Agency (2009), 'NTA Business Plan 2009-2010', (National Treatment Agency for Substance Misuse).
- Hickman, Matt, et al. (2011), 'Promoting recovery and preventing drug-related mortality: competing risks?' Journal of Public Health, 33 (3), 332-34
- Noble M, McLennan D, Wilkinson, K, et al (2008), 'The English Indices of Deprivation 2007', (London: Communities and Local Government)
- EuroQol (1990), 'EuroQol - a new facility for the measurement of health-related quality of life', Health Policy, 16 (3), 199-208
- Beck AT, Ward CH, Mendelson M, et al (1996), 'An inventory for measuring depression', Archives of General Psychiatry, 4, 561-71
- Bao, Yan-ping, et al. (2009) 'A Meta-Analysis of Retention in Methadone Maintenance by Dose and Dosing Strategy', The American Journal of Drug and Alcohol Abuse, 35 (1), 28-33
- NICE (2003) Moving beyond effectiveness in evidence synthesis: methodological issues in the synthesis of diverse sources of evidence. National Institute for Health and Clinical Excellence, London
- Moos, R. H. (2003), 'Addictive Disorders in context: principles and puzzles of effective treatment and recovery', Psychology of Addictive Behaviors, 17 (1), 28-33
- Neale, Joanne (1999), 'Drug users’ views of substitute prescribing conditions', International Journal of Drug Policy, 10 (3), 247-58
- Marsden J, Eastwood B, Bradbury C, et al (2009) Effectiveness of community treatments for heroin and crack cocaine addiction in England: a prospective, in-treatment cohort study. Lancet 374; 1262-70
- Strang, John, et al. (2007), 'Does prescribing for opiate addiction change after national guidelines? Methadone and buprenorphine prescribing to opiate addicts by general practitioners and hospital doctors in England, 1995–2005', Addiction, 102 (5), 761-70
- Rosenbaum, Marsha (1995), 'The demedicalization of methadone maintenance', Journal of Psychoactive Drugs, 27 (2), 145-49
- D'Aunno T, Vaughn T. E. (1992), 'Variations in methadone treatment practices: Results from a national study', JAMA: The Journal of the American Medical Association, 267 (2), 253-58

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




