Effects of Lornoxicam on the Haemodynamic and Catecholamine Response to Laryngoscopy and Tracheal Intubation
M. Daabiss, M. Hashish, R. AlOtaibi and R. AlDafterdar
Cite this article as: BJMP 2010;3(3):a328
|
|
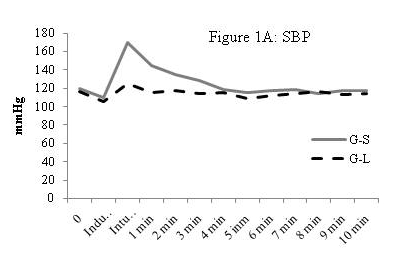
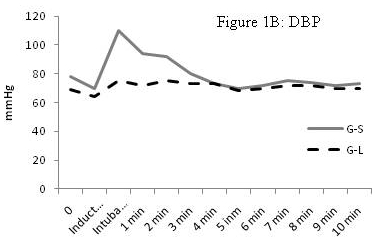
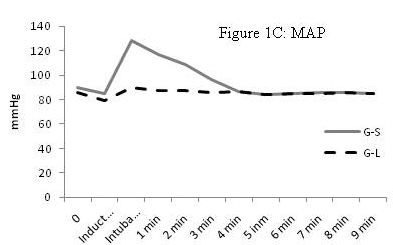
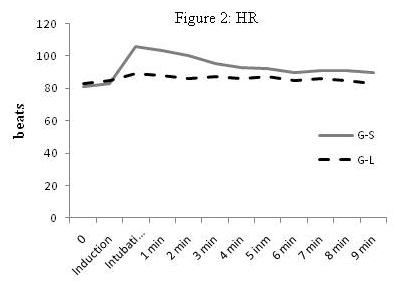
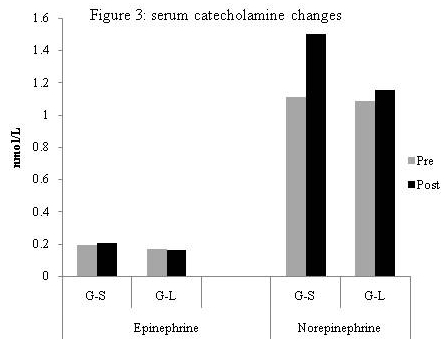
Abstract Background and objectives: Laryngoscopy and tracheal intubation are associated with haemodynamic responses which might increase morbidity and mortality in some patients. Lornoxicam is a non-steroidal anti-inflammatory drug, which when added to fentanyl successfully attenuated the pressor response of intubation. The aim of this study was to evaluate the effect of lornoxicam individually on the haemodynamic response and serum catecholamine levels following laryngoscopy and tracheal intubation. Methods: Fifty adult patients scheduled for general anaesthesia with endotracheal intubation were enrolled in this randomised, double-blind placebo-controlled study. They were divided into two equal groups to receive intravenously either lornoxicam 16 mg or placebo, half an hour before surgery. Systolic, Diastolic and mean arterial pressure and heart rate were recorded before and after the induction of anaesthesia, and every minute after intubation for 10 minutes. Serum catecholamine levels were measured before induction and 1 minute after intubation. Results: After induction, there was a significant decrease in blood pressure in both groups.In the control group, a significant increase in serum catecholamine levels 1 minute after intubation as well as a significant increase in the haemodynamic parameters was observed in the first 3 minutes after tracheal intubation (P <0.05). Conclusion: Lornoxicam 16 mg attenuates the pressor response to laryngoscopy and intubation of the trachea. Keywords: Tracheal intubation, cardiovascular responses, Laryngoscopy, Lornoxicam, anaesthesia. |
Introduction
|
|
Group S (Saline)
|
Group L (Lornoxicam)
|
|
No. of patients
|
25
|
25
|
|
Sex (female/male)
|
10/15
|
12/13
|
|
Age (yrs)
|
31.5 ± 5.6
|
33.1 ± 4.4
|
|
ASA (I/II)
|
19/6
|
20/5
|
|
Weight (Kg)
|
69.7 ± 4.2
|
66.9 ± 6.7
|
|
Height (cm)
|
167.9 ± 8.6
|
170.2 ± 4.5
|
|
Duration of laryngoscopy and intubation (sec)
|
14.9 (1.7)
|
16.2 (1.2)
|
|
HR/ minute
|
80.13±8.69
|
81.87±11.62
|
|
MAP mmHg
|
89.97±10.1
|
85.83±9.23
|
|
Systolic BP mmHg
|
120.2±11.2
|
117.44±17.1
|
|
Diastolic BP mmHg
|
78.7±9.91
|
73.13±12.42
|
|
|
Group S
(Saline)
|
Group L
(Lornoxicam)
|
P
|
|
After induction
|
85.15±10.76
|
83.32±8.44
|
.062
|
|
0 minute after intubation
|
106±14.3
|
88.17±8.89
|
.000*
|
|
1 minute
|
101.71±11.15
|
86.92±9.11
|
.000*
|
|
2 minute
|
97.39±12.07
|
84.88±10.36
|
.019*
|
|
3 minute
|
95.48±12.95
|
81±9.91
|
.036*
|
|
|
Group S
(Saline)
|
Group L
(Lornoxicam)
|
P
|
|
After induction
|
84.65±8.3
|
79.77±9.92
|
.055
|
|
0 minute after intubation
|
129±16.54
|
91.73±10.7
|
.000*
|
|
1 minute
|
119.95±18.2
|
86.01±8.99
|
.000*
|
|
2 minute
|
105.33±13.15
|
83.62±10.63
|
.008*
|
|
3 minute
|
96.1±10.11
|
83.47±8.8
|
.024*
|
|
|
Group S
(Saline)
|
Group L
(Lornoxicam)
|
P
|
|
After induction
|
107.38±11.71
|
102.25±12.89
|
.069
|
|
0 minute after intubation
|
169.27±18.29
|
117.35±13.5
|
.0001*
|
|
1 minute
|
141.53±15.51
|
113.68±12.91
|
.005*
|
|
2 minute
|
128 ±11.2
|
115.39±14.17
|
.014*
|
|
3 minute
|
122.99±12.56
|
111.67±14.8
|
.037*
|
|
|
Group S
(Saline)
|
Group L
(Lornoxicam)
|
P
|
|
After induction
|
72.49±8.79
|
68.99±8.1
|
.085
|
|
0 minute after intubation
|
109.53±14.22
|
78.48±8.51
|
.000*
|
|
1 minute
|
92.18±10.63
|
74 ±7.75
|
.007*
|
|
2 minute
|
89.77 ±11.34
|
78.12±7.98
|
.02*
|
|
3 minute
|
81.45±8.8
|
73.6±8.21
|
.043*
|
|
|
|
Group S
(Saline)
|
Group L
(Lornoxicam)
|
P
|
|
Epinephrine
|
Pre intubation
|
.195±.119
|
.179±.104
|
.085
|
|
|
1 min postintubation
|
.206±.112
|
.181±.087
|
.038*
|
|
Norepinephrine
|
Pre intubation
|
1.11±.633
|
1.098±.51
|
.059
|
|
|
1 min postintubation
|
1.499±.903
|
1.107±.524
|
.000*
|
In our study, lornoxicam attenuated the pressor response to laryngoscopy and tracheal intubation; SBP, DBP, MAP and HR were significantly lower in L group compared to S group in the first 3 min after intubation. This may be attributable to the analgesic action of lornoxicam mediated through the antiprostaglandin effect of COX inhibition, the release of endogenous dynorphin and β-endorphin 14, a decrease in peripheral and central prostaglandin production, 16 as well as it exerting some of its analgesic activity via the central nervous system 17.
In agreement with our results, Bruder and colleagues 18 reported that laryngoscopy and intubation violate the patient's protective airway reflexes with marked reflex changes in the cardiovascular system and lead to an average increase in blood pressure by 40-50% and a 20% increase in heart rate. Kihara and colleagues 19, when comparing the haemodynamic response to direct laryngoscopy with the intubating laryngeal mask and the Trachlight device, reported that the HR increased compared with preoperative baseline values in all groups. Moreover, both systolic and diastolic pressure increased after tracheal intubation for 2 mins. with the highest values in the hypertensive group receiving direct laryngoscopy.
In a previous study done by Riad and Moussa 7, i.v. administration of 8 mg lornoxicam half an hour before surgery added to fentanyl 1 µg Kg-1 during induction of anaesthesia was found to attenuate the haemodynamic response to laryngoscopy and tracheal intubation in the elderly. However, it was unclear whether this was attributed to the drug's narcotic effect. Therefore, our study was designed to evaluate the use of lornoxicam individually, in a single i.v. administration of 16 mg lornoxicam half an hour before surgery. Lornoxicam 8 mg was not used as it was proven to have an inadequate analgesic effect 15.
There have been a few studies which have measured catecholamine levels after intubation. Our results are consistent with those of Russell et al 2 and Shribman et al 20 who reported significant elevations in serum levels of norepinephrine and epinephrine following laryngoscopy and tracheal intubation. Hassan and colleagues 21 concluded that during laryngoscopy and endotracheal intubation, placing the tube through the cords and inflating the cuff in the infraglottic region contributes significantly to sympathoadrenal response caused by supraglottic stimulation.
When assessing techniques to ameliorate the cardiovascular responses to intubation; the drugs used to induce anaesthesia may influence the results. We induced anaesthesia with propofol which produces hypotension. This may compensate in part for the cardiovascular changes attributable to laryngoscopy and tracheal intubation. This could be considered a limitation of the present study. The omission of opioids during the induction of anaesthesia in healthy young patients should not be a concern.
In conclusion, pretreatment with lornoxicam in the doses given in this study, attenuates the pressor response to laryngoscopy and the intubation of the trachea.
|
Competing Interests None declared Author Details M. Daabiss, Riyadh Armed Forces Hospital, Department of Anesthesia, KSA M. Hashish, Armed Forces Hospital King Abdulaziz Airbase Hospital Dhahran, Department of Anesthesia, KSA R. AlOtaibi, Riyadh Armed Forces Hospital, Department of Anesthesia R. AlDafterdar, Riyadh Armed Forces Hospital, Department of Laboratory, Riyadh, KSA CORRESPONDENCE: Mohamed Daabiss Department of Anesthesia, Riyadh Armed Forces Hospital Mail box: 7897-D186 Riyadh 11159 Saudi Arabia Email: madaabiss@yahoo.com |
References
1.Reid LC, Brace DE. Irritation of the respiratory tract and its reflex effect upon heart. Surg Gynaec & Obst; 1940; 70: 157-62. (s)
2.Russell WJ, MorrIs RG, FrewIn DB, Drew SE. Changes in plasma catecholamine concentration during endotracheal intubation. Br J Anaesth; 1981, 53:837-9.3.Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth 1996; 8: 63–79.4.Fassoulaki A and Kaniaris P. Intranasal administration of nitroglycerin attenuates the pressor response to laryngoscopy and intubation of the trachea. Br J Anaesth 1983; 55:49–525.Vucevic M, Purdy GM, Ellis FR. Esmolol hydrochloride for management of the cardiovascular stress responses to laryngoscopy and tracheal intubation. Br J Anaesth 1992; 68:529–306.Anila D. Malde, Vineet Sarode, Attenuation of the Hemodynamic Response to Endotracheal Intubation: Fentanyl versus Lignocaine. The Internet J Anesthesiol 2007; 12 (1).7.McCormack K. The evolving NSAID: focus on Lornoxicam. Pain Rev 1999; 6 (4), 262-78.8.Riad W, Moussa A. Lornoxicam attenuates the hemodynamic responses to laryngoscopy and tracheal intubation in the elderly. Eur J Anaesthiol 2008; 25: 732–6.9.Ankier SI, Brimelow AE, Crome P, Johnston A, Warrington SJ, Turner P, Ferber HP. Chlortenoxicam pharmacokinetics in young and elderly human volunteers. Postgrad Med J 1988; 64: 752–754.10. Holly JMP, Makin HLJ. The estimation of catecholamines in human plasma: a review. Anal Biochem 1983; 128: 257–74.11. Zhao H, Ye TH, Gong ZY, Xue Y, Xue ZG, Huang WQ. Application of lornoxicam to patient-controlled analgesia in patients undergoing abdominal surgeries. Chin Med Sci J 2005; 20: 59-62.12. Norholt ES., Pedersen S, Larsen U. Pain control after dental surgery: a double blind, randomized trial of lornoxicam versus morphine. Pain 1996; 67: 335-43.13. Balanika M., Tsitsika M., Wilczynski W. The use of lornoxicam-mepridine combination for postoperative analgesia. Eur J Anaesthiol 2000;17, 771-8.14. Staunstrup H, Ovesen J, Larsen T. Efficacy and tolerability of lornoxicam versus tramadol in postoperative pain. J Clin Pharmacol 1999; 39: 834-41.15. Daabiss M, Al-Sherbiny M, Al-Otaibi R, El-Nimar R. Analgesia in day-case ENT surgery: The efficacy of lornoxicam. Br J Med Practitioner 2009; 2(3); 46-50.16. Hitzenberger G, Radhofer-Welte S, Takacs F, Rosenow D. pharmacokinetics of lornoxicam in man. Postgrad Med J. 1990; 66(Suppl 4): S22-7.17. Buritova J, Besson JM. Dose-related anti-inflammatory analgesic effects of lornoxicam: a spinal c-Fos protein study in the rat. Inflamm Res 1998;47 (1), 18-25.18. Bruder N, Granthil C, Ortega D. Consequences and prevention methods of hemodynamic changes during laryngoscopy and intubation. Ann Fr Anaesth Reanim 1992; 11(1):57-71.19. Kihara S, Brimacombe J, Yaguchi Y, Watanabe S, Taguchi N, Komatsuzaki T. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg 2003; 96: 890–895.20. Shribman AJ, Smith G, Achola kJ. Cardiovascular and catecholamine response to laryngoscopy with and without endotracheal intubation. Br J Anaesth; 1987, 59:295-9.21. Hassan, HG, El-Sharkawy, Renk H, Mansour G, Fouda A. Haemodynamic and catecholamine responses to laryngoscopy with Vs without endotracheal intubation. Acta Anaesthesiol Scand 1991; 35: 442.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




