Dysphagia Lusoria presenting with Pill-induced Oesophagitis - A case report with review of literature
Malhotra A, Kottam RD and Spira RS
Cite this article as: BJMP 2010;3(2):312
|
|
Abstract Extrinsic oesophageal compression from vascular structures usually remains asymptomatic. Occurrence of dysphagia is an uncommon problem. We present a rare case of dysphagia lusoria from right sided aortic arch presenting as pill-induced oesophagitis caused by a testosterone pill. A thorough literature review on both the conditions is then presented to address pathogenesis, diagnosis, and management. Keywords: Dysphagia Lusoria, Pill-induced oesophagitis, drug-induced oesophagitis |
Introduction
Oesophageal compression by a vascular structure resulting in dysphagia is uncommon. There have been multiple reports in the medical literature of almost every major vascular structure in the chest causing some degree of oesophageal compression and subsequent dysphagia(1, 2). In 1794, David Bayford, described a case of a 62 year-old lady having dysphagia due to an aberrant right subclavian artery. He coined the term “dysphagia lusus naturae”, which means “Freak of nature” (3).
Pill-induced esophagitis is associated with the ingestion of many pills and presents an uncommon cause of erosive oesophagitis (4). Multiple different classes of drugs have been described to be hazardous to the oesophageal mucosa and cause pill-induced oesophagitis (5, 6). Although uncommon in itself, dysphagia lusoria has not been described in literature to present as pill-induced oesophagitis. We present the first case of dysphagia lusoria causing pill-induced oesophagi's by testosterone pills in a young healthy man. Pubmed review of the English medical literature has been conducted to discuss the epidemiology, pathogenesis and management of this uncommon disorder.
Case Presentation:
A 26 year-old man with no significant past medical history presented with 5 days of dysphagia (for both solids and liquids), odynophagia and retrosternal chest discomfort. He admitted to having occasional difficulty swallowing for past 2-3 months for solids only. He denied any heartburn, cough, regurgitation, loss of appetite, weight loss, fever, chills, haematemesis or melaena. He denied tobacco or alcohol use. 2 weeks prior to presentation he had started taking testosterone pills for body-building. Physical examination was completely unremarkable.
A barium oesophagram showed extrinsic oblique compression of the oesophagus at the level of the carina as it passes through the aorta. CT scan and MRI of the chest revealed a right-sided aortic arch crossing posteriorly to the oesophagus with proximal oesophageal dilatation consistent with Dysphagia Lusoria. Endoscopy noted erosive oesophagitis/distinct ulceration extending from 18cm into a pulsatile area of narrowing at 20 cm with normal mucosa visualized distally.
Biopsies revealed oesophageal squamous mucosa with marked acute inflammation, reactive changes and no evidence of viral inclusions. Surgical management was discussed with the patient, but given the short duration of symptoms and the patient's stable weight, providing symptomatic relief with lifestyle changes, together with a trial of medications such as proton pump inhibitors were considered. At 2 weeks follow-up whilst taking proton pump inhibitors and having discontinued the testosterone pills, the patient experienced complete resolution of symptoms.
Epidemiology:
Dysphagia Lusoria: Moltz et al, found that lusorian artery has a prevalence of about 0.7% in the general population, based on the post-mortem findings(7). Also, out of 1629 patients who underwent endoscopy for various reasons, 0.4% had a finding of a lusorian artery in a report from Fockens et al(8). It has also been concluded based on the autopsy results and retrospective analysis of patients’ symptoms during life that about 60-70% of these patients remain asymptomatic (7). Coughing, dysphagia, thoracic pain, syncope and Horner's syndrome may develop, but usually present in old-age(9).
Pill-Induced Oesophagitis: The data on pill-induced oesophagitis is rather limited. A Swedish study found an incidence of 4 cases per 100,000 population/year(10). Wright found the incidence of drug-induced oesophageal injury to be 3.9/100,000(11). This may be underestimated and does not include subclinical or misdiagnosed cases. Also, cases are reported selectively, due to clustering of cases, newly implicated pills or rare complications. The incidence today is probably much higher due to increased use of prescription medications, widespread use of endoscopy and an ageing population. All these factors limit our ability to correctly assess the true epidemiology of this iatrogenic disorder.
Pathogenesis
Dysphagia Lusoria: During embryological development, the aortic sac gives rise to six aortic arches and with further development the arterial pattern is modified and the fourth arch persists on both sides and some vessels regress. In right arch anomaly, the left arch atrophies and disappears whereas the right arch persists. If both arches persist, they form a double arch or a vascular ring encircling the trachea and oesophagus (12).
Pill-induced oesophagitis: Several lines of evidence confirm that oesophageal mucosal injury is caused by prolonged contact with the drug contents(13, 14) .On clinical grounds, patients frequently report a sensation of a pill stuck in the oesophagus before the development of symptoms and the frequent occurrence of symptoms after improper pill ingestion. Endoscopically, the evidence includes occasional observation of pill fragments at the site of injury, sharp demarcation of the injury site from the normal tissue and the frequent localization of the injury to the areas of oesophageal hypomotility or anatomic narrowing(4, 15). Therefore factors predisposing to the drug-induced oesophageal injury can be divided into two main categories: patient or oesophageal factors (16, 17, 18,19,20,21) and drug or pharmaceutical factors as shown in tables 1 and 2 (13,14,22,23,24).
|
Old Age
Decreased Salivation
Pill intake in recumbent position
Lack of adequate fluid intake with the drug
Structural abnormalities of esophagus
Hypomobility of the esophagus
|
|
Chemical structure(sustained release pills, gelatinous surface)
Formal structure (capsule increases risk over the tablet)
Solubility
Simultaneous administration of multiple medications
|
Clinical Presentation
Dysphagia Lusoria: As previously mentioned the disorder remains asymptomatic in majority of the patients. Symptomatic adults usually present with dysphagia for solids, (91%), chest pain (20% or less). Less commonly, patients may have cough, thoracic pain or Horner’s syndrome (27,28). In infants, respiratory symptoms are the most predominant mode of clinical presentation. This is believed to be due to absence of tracheal rigidity, allowing for its compression with resulting stridor, wheezing, cyanosis etc (9) . Richter et al. reported average age of presentation to be 48 years (27). Various mechanisms to explain this delayed presentation have been proposed such as increased rigidity of the oesophagus, rigidity of the vessel wall due to atherosclerosis, aneurysm formation (especially Kommerell’s diverticulum), elongation of the aorta etc (9, 29,30) .
Pill-induced oesophagitis: Patients with pill-induced injury usually present with odynophagia, dysphagia and/or retrosternal chest pain(4) . Symptoms can occur after several days after starting a drug, but frequently occur after the first dose. (13) .Fever and haematemesis signifying a possible mediastinal extension can occur without chest pain(32,33). Pharyngitis due to the pill lodged in the hypopharynx has been reported(34).
Our case presents a typical example of asymptomatic Dysphagia Lusoria, who developed acute dysphagia, odynophagia and retrosternal chest discomfort immediately after the initiation of the offending agent; which is very typical of pill-induced oesophageal injury.
Diagnostic approach
Dysphagia Lusoria: The best method to diagnose an aberrant right subclavian artery presenting with difficulty swallowing is initially with a barium oesophagram followed by a CT or MRI scan. (27) .Angiography although considered gold standard for the diagnosis of vascular abnormalities is now largely supplanted by newer less invasive techniques such as CT or MR angiography. Upper endoscopy may reveal a pulsating compression of the posterior wall of the oesophagus as in our case(9, 27). Endoscopic ultrasound, especially with Doppler technology may be helpful to confirm the vascular nature of the abnormality(27). Oesophageal manometry usually shows non-specific findings. High peristaltic pressures have been reported in the proximal oesophagus above the level of the compression (9, 35).
Pill-induced oesophagitis: Barium studies can be normal, and slowing of barium column may be the only abnormality seen(31). Double contrast studies may however, increase the yield of a positive result(36). Kikendall et al. reported that endoscopy revealed the evidence of injury in all the patients (5) . Endoscopy most commonly reveals one or more discrete well demarcated ulcers with normal surrounding mucosa. Ulcers may range from pin-point to several centimetres in diameter(5). Biopsies, if performed, help to distinguish the condition from infection and neoplasia.
Our case shows a distinct oblique compression in the posterior wall of oesophagus on the barium study (fig 1) and classic findings on MR/CT with contrast which also excluded any other thoracic vascular abnormalities (fig 2-5). Endoscopic images of a shallow ulcer are shown in fig 6,7.
![]()

Figure 1- Barium esophagram depicting the extrinsic indentation of the esophagus as it crosses the aorta.
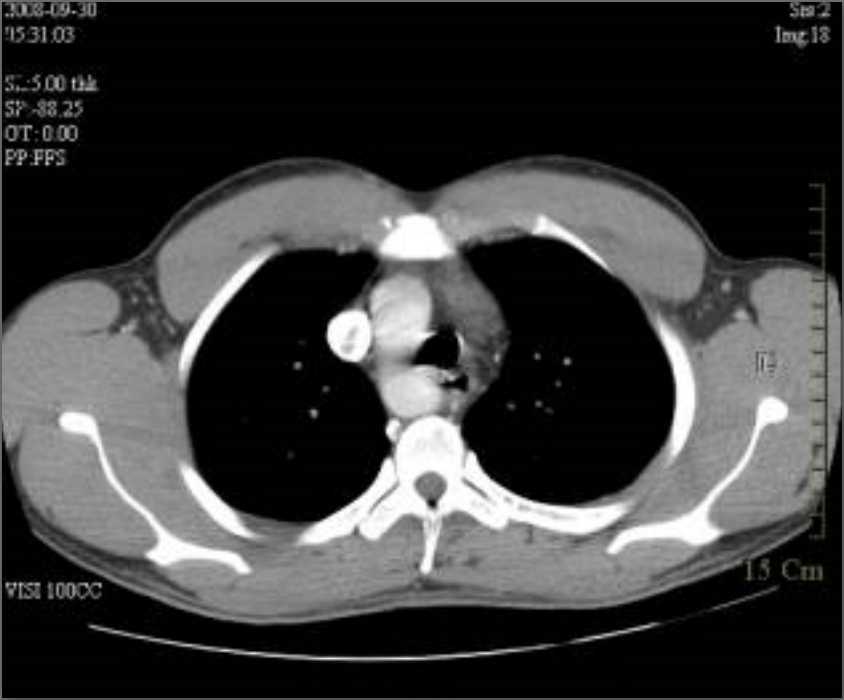
Figure 2- CT scan of the thorax demonstrating esophageal compression from a posteriorly placed aorta.

Figure 3- Magnetic resonance image showing esophageal compression with proximally dilated esophagus.
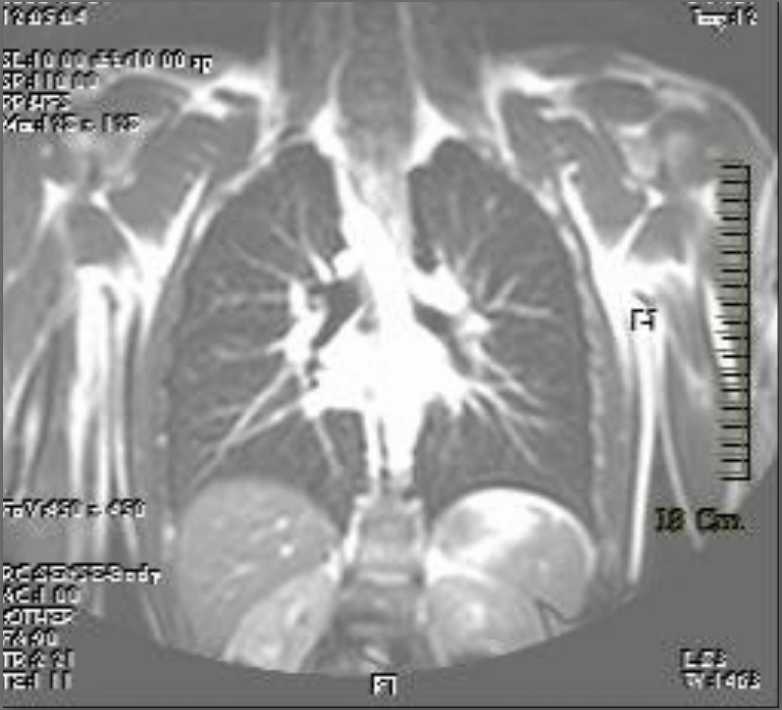
Figure 4- CT image showing the right sided origin of the aortic arch.
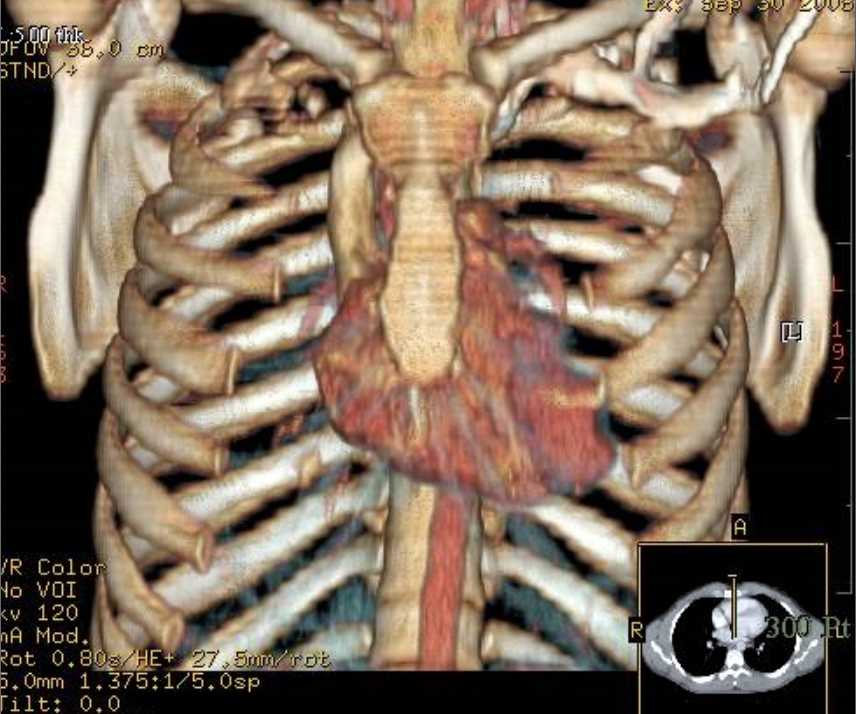
Figure 5- Three Dimensional image of the heart and the right sided approach of the arch.

Figure 6- Endoscopic view of esophageal inflammation at the site of compression.
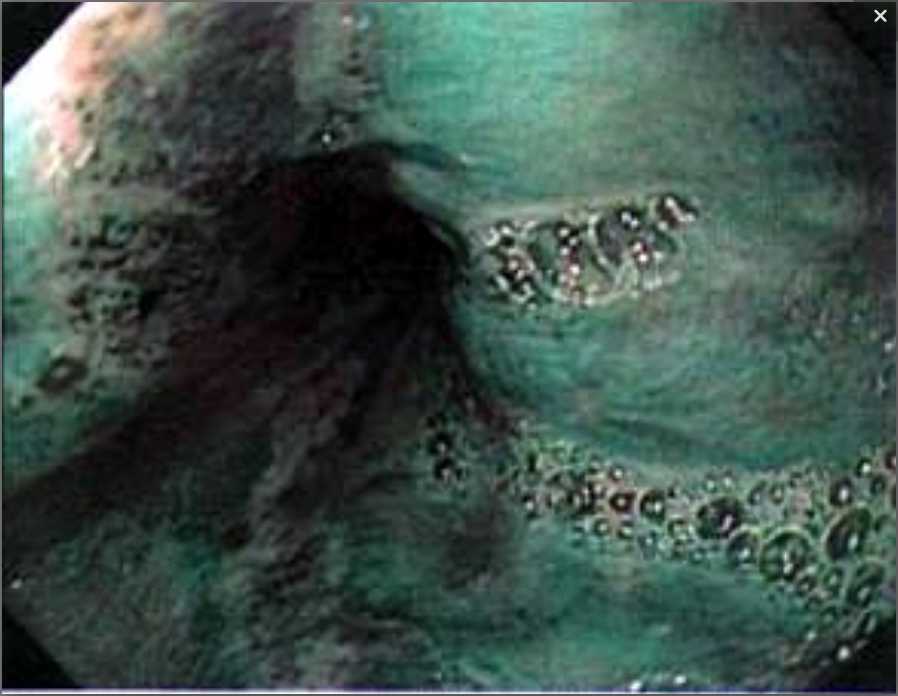
Figure 7- Endoscopic image of the esophageal injury using narrow band imaging.
Treatment
Dysphagia Lusoria: The treatment of patients with DL primarily depends upon the severity of symptoms. Mild to moderate cases are managed by lifestyle and dietary changes such as eating slower, chewing well, sipping liquids, weight reduction and reassurance as in our case.(9,27) Janssen et al also reported in a series of 6 patients that 3/6 improved with proton-pump inhibitor alone or in combination with the prokinetic drug cisapride (9) .Severe symptoms and failure of medical therapy may need surgical evaluation and treatment. Richter et al. reported 14/24 patients who underwent surgical repair of the aberrant vessel for DL(27) . Bogliolo et al proposed endoscopic dilation as a temporary alternative to relieve symptoms in patients who are poor surgical candidates (37) .
Pill-induced oesophagitis: Most uncomplicated cases of pill-induced oesophagitis may heal spontaneously, with resolution of symptoms in a few days to a few weeks. Withdrawal of the offending drug and avoidance of topically irritating foods such as citrus fruits, alcohol is imperative to aid healing (4, 13). Sucralfate, topical anaesthetics, and acid suppression are often used to aid in relief of pain(4, 15). Rarely, in severe cases, parenteral nutrition or endoscopic dilation of chronic strictures may be required. (15, 25)
Conclusion
Our case demonstrates a typical case of DL presenting with pill-induced oesophagitis who responded to conservative and acid suppressive therapy. Identifying the risk factors and adequate patient education is the key to prevention.
|
Competing Interests None Declared Author Details MALHOTRA A, Division of Gastroenterology, Seton Hall University of Health and Medical Sciences, South Orange, NJ KOTTAM RD, Division of Gastroenterology, Seton Hall University of Health and Medical Sciences, South Orange, NJ SPIRA RS, Division of Gastroenterology, Seton Hall University of Health and Medical Sciences, South Orange, NJ and Department of Medicine, Clinical Assistant Professor of Medicine, UMDNJ, Newark, NJ CORRESPONDENCE: RAGHU D KOTTAM, MD, Dept. of Gastroenterology, St.Michael’s Medical Center, 111 Central Avenue, Newark, NJ, 07102 Email: raghudk@yahoo.com |
References
1. Cappell M S.Endoscopic, radiographic, and manometric findings associated with cardiovascular dysphagia. Dig Dis Sci 1995; 40:166-76
2. Stagias J G, Ciarolla D, Campo S et al. Vascular compression of the esophagus: a manometric and radiologic study. Dig Dis Sci 1994; 39:782-6
3. Bickston S, Guarino P, Chowdhry. Education and imaging. Gastrointestinal: dysphagia lusoria. J Gatroenterol Hepatol.2008; 23(6): 989
4. Kikendall, JW. Pill Esophagitis J clin Gastroenterol 1999; 28(4), 298-305
5. Kikendal JW, Friedman AC, Morakinyo AO, et al: Pill-induced esophageal injury. Dig Dis Sci 1983; 28:174-182.
6. Mason SJ, O’Meara TF: Drug-induced esophagitis. J Clin Gastroenterol 1981; 3:115-120
7. Molz G, Burri B.aberrant subclavian artery (arteria lusoria): Sex differences in the prevalance of various forms of the malformations. Evaluation of 1378 observations. Virch Arch A Pathol Anat Histol 1978; 380:303-15
8. Fockens P, Kisman K, Tytgat GNJ.Endosonographic imaging of an aberrant right subclavian (lusorian) artery. Gastrointest Endosc 1996; 43:419
9. Janssen M, Baggen MGA, Veen HF et al, Dysphagia lusoria: clinical aspects, manometric findings, diagnosis and therapy, Am J Gastroenterol 200; 95:1411-1416
10. Carlborg B, Densert O. Medikamentella esofagusstrikturer, Lakartidningen 1978; 75: 4609-11
11. Wright V. The oesophagus. In: Walker P, Durie JR, Hamilton JA, et al, editors. Pediataric gastrointestinal disease: pathophysiology, diagnosis and management, vol. I. Philadelphia: BC Decker Inc, 1991:375-6
12. Lunde R, Sanders E, Hoskam JA. Right aortic arch symptomatic in adulthood. Neth J Med, 2002; 60(5): 212-5
13. Boyce HW. Drug-induced Esophageal Damage: diseases of medical progress. Gastrointest Endos 1998; 47:547-50
14. Boyce HW. Drug-induced Esophageal and Gastric Damage. In: Tytgat GNJ, VAN Blankenstein M, and editors. Current topics in gastroenterology and hepatology. New York: Georg Thieme Verlag, 1996:170-95
15. Jaspersen D, Drug-induced oesophageal Disorders, Pathogenesis, incidence, prevention and management. Drug safety 2000; 22(3): 237-49
16. Teplick JG, Teplick SK, and Ominsky SH et al: Esophagitis caused by oral medication. Radiology 1980. 134:23-25
17. Rosenthal T, Adar R, and Militiani S: Esophageal ulceration and oral potassium chloride ingestion. Chest 1974. 65:463-65
18. Walta DC, Giddens JD, Johnson LF, ET AL: localized proximal esophagitis secondary to ascorbic acid ingestion and esophageal motor disorder. Gastroenterology 1076. 70: 766-69
19. Burrington JD; Clinitest burns of the esophagus. Ann Thorac Surg 1975. 20:400-404
20. Evans KT, Roberts GM: where do all the tablets go? Lancet 2: 1976. 1237-1239
21. Humphries TJ, Castell DO: Pressure profile of esophageal peristalsis in normal humans as measured by the direct intraesophageal transducers. IS J Dig Dis 1977? 22: 641-645
22. Marvola M, Rajaniemi M, Marttila E. Effect of dosage form and formulation factors on the adherance of drugs to the oesophagus. J Pharm Sci 1983; 72: 1034-6
23. Channer KS, Virjee JP. The effect of size and shape of tablets on their oesophageal transit. J Clin Pharmacol 1986; 26:141-6
24. Hey H, Jorgensen F, Sorensen K, et al. Oesophageal transit of six commonly used tablets and capsules. BMJ 1982; 285:1717-9
25. Kikendall JW.Pill-induced esophageal injury. Gastroenterol Clin North Am1991; 20: 835-46
26. Kikendall JW.pill-induced injury. In: Castell DO, Richter JE, Eds. The esophagus, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999: 527-37
27. Levitt B, Richter JE. Dysphagia lusoria: a comprehensive review. Diseases of the Esophagus, 2007.20:455-460
28. Carrizo GJ, Marjani MA. Dysphagia lusoria caused by an aberrant right subclavian artery. Tex Heart Inst J 2004; 31:168-71
29. Menally PR, Rak K M. Dysphagia lusoria caused by the persistent right aortic arch with aberrant left subclavian artery and diverticulum of Kommerell.Dig Dis Sci 1992; 37:144-9
30. Kantarceken B, Bulbuloglu E, Yuksel M et al. Dysphagia lusorium in elderly, a case report. World J Gastro 2004; 10:2459-60
31. Coates AG, Nostrant TT, and Wilson JAP et al. Esophagitis caused by NSAID: case reports and review of the literature on Pill-induced esophageal injury. Southern Medical Journal 1986; 79(9): 1094-97
32. Pahakka HJ:Drug-induced corrosive injury of the esophagus.JLaryngol Otol 1978,92:927-31
33. William JG: drug induced oesophageal injury, Br Med J 2: 273,1979
34. Abbarah TR, Fredell JE, and Ellenz GB: Ulceration by the oral ferrous sulfate. JAMA 236:2370,1976
35. Berenzweig H, Baue A E. Dysphagia lusoria: report of a case and review of the diagnostic and surgical approach. Dig Dis Sci 1980; 25:630-6
36. Sakai H, Seki H, and Yoshida Y et al: Radiological study of drug-induced esophageal ulcer. Rinsho Hoshasen 1980,25:27-34
37.Bogliolo G, Ferrara M, Masoni L et al. Dysphagia lusoria: proposal of a new treatment. Surg Endosc 1987; 1:255-7

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




