Disseminated Nocardiosis (nocardia farcinica) in Myasthenia Gravis: An Antimicrobial Dilemma
Raja Shariff REF & Sapuan S
Cite this article as: BJMP 2020;13(1):a001
|
|
Abstract Introduction: Nocardiosis commonly occurs in immunocompromised patients. We report a case of disseminated nocardiosis in a Myasthenia Gravis (MG) patient, and how antimicrobial selection was complex. Case Report: A 68-year old woman, with myasthenia gravis, a pre-existing stable subdural haematoma and history of azathioprine-related myelosuppression, presented to us following a week of diarrhea and lethargy. Her inpatient stay was complicated by dyspnoea and bilateral consolidation on chest radiography. Blood cultures grew nocardia farcinica. Computed Tomography (CT) of her thorax, abdomen and pelvis revealed bilateral lung consolidation and a sigmoid colon collection. Unfortunately, initiation of first-line antimicrobials in this patient proved to be difficult as she suffered from trimethoprim/sulfamethoxazole related pancytopenia, and was limited to non-amakicin, non-fluoroquinolone therapy, to avoid MG exacerbation. She was eventually commenced on concurrent co-amoxiclav and meropenem, alongside having her sigmoid abscess drained. Discussion: Although nocardiosis is treatable, pre-existing MG and myelosuppression led to complex decision making. Use of prolonged intravenous antibiotics alongside surgical drainage of collections can improve prognosis, although mortality rates in disseminated nocardiosis remain high. Conclusion: Nocardiosis poses a unique challenge in the MG population due to limitations in suitable antibiotics, and decision making on management should ideally be multi-disciplinary as seen in our case. Keywords: myasthenia gravis, disseminated nocardiosis, nocardia farcinica, case reportAbbreviations: myasthenia gravis (MG), computed tomography (CT), central nervous system (CNS) |
Introduction
Nocardia sp. are aerobic, gram-positive microorganisms found mainly in soil and stagnant water. Nocardiosis commonly occur in immunocompromised patients, is often multi-systemic and easily mistaken for tuberculosis when involving the lungs 1 2. We report a complex case of disseminated nocardiosis in a patient already suffering from Myasthenia Gravis (MG) and azathioprine-induced myelosuppression, in which selection of antimicrobials and management planning became complex.
Case Report
A 68-year old lady, known to have generalized MG for 12 years, presented to our centre following a week history of diarrhea and lethargy. She describes having loose stools, up to 8 times per day, chills and rigors, but denied per rectal bleeding or melaena. The patient was, on regular oral prednisolone (50mg a day). She had recently ceased her azathioprine 4 months prior due to severe anaemia, linked to myelosuppression following a bone marrow aspiration test revealing markedly reduced erythropoiesis, normal oesophageo-gastro-dudodenoscopy and colonosocopy, and having normal thiopurine methyltransferase levels prior to azathioprine initiation. The patient had several admissions in that 4 months due to her anaemia, requiring packed cell transfusions, and had recently sustained an interhemispheric subdural bleed two weeks prior following a mechanical fall. At the time, hemoglobin and platelet levels had returned within normal range. Clinical examination was unremarkable and her vitals on arrival included an oxygen saturation of 98% on room air with a normal chest radiography on arrival (Figure 1a). The patient was subsequently treated for infective gastroenteritis, and was started on metronidazole.
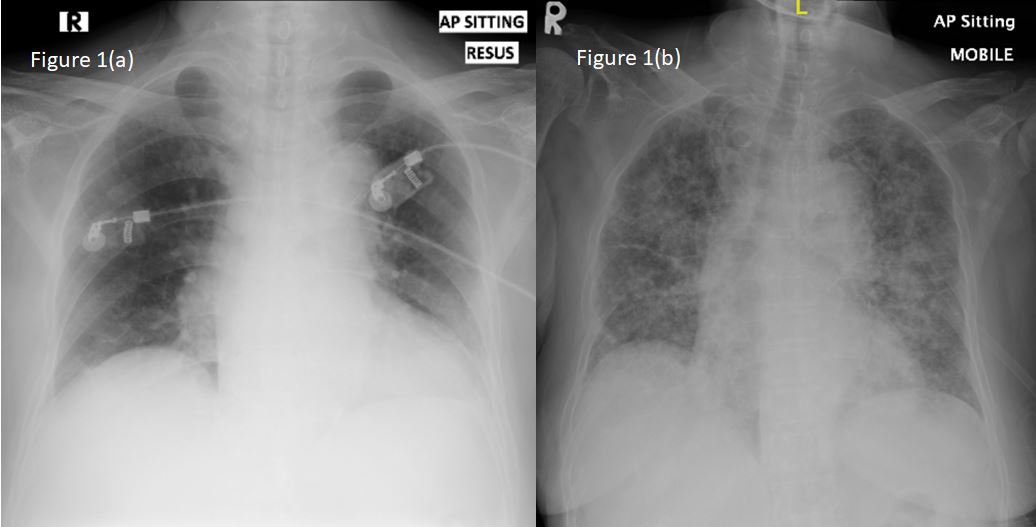
Figure 1: Chest radiography on (a) initial presentation and (b) 48-hours into admission, showing newly developed diffuse bilateral consolidation.
Unfortunately, 48 hours into her inpatient stay, the patient developed acute dyspnoea in which her oxygen saturation dropped to 77% under room air and examination revealed diffuse, coarse crepitations bilaterally. A repeat chest radiograph confirmed diffuse consolidation bilaterally (Figure 1b). She was subsequently treated for a hospital-acquired pneumonia, and had her antibiotics swapped to intravenous ceftriaxone. Unfortunately, the patient showed little improvement on the ward, which prompted further investigation. Her blood cultures revealed presence of nocardia farcinica which was resistant to ceftriaxone. In view of being immunosuppressed, a computed tomography (CT) imaging of the brain, thorax, abdomen and pelvis (Figure 2) was performed. Imaging showed extensive bilateral lung consolidation and reticulonodular opacities, predominantly in upper lobes. There was also evidence of sigmoid colon diverticulitis with a rim-enhancing collection adjacent to the posterior aspect of the proximal-to-mid sigmoid colon (2.9 x 2.6 x 2.6 cm).
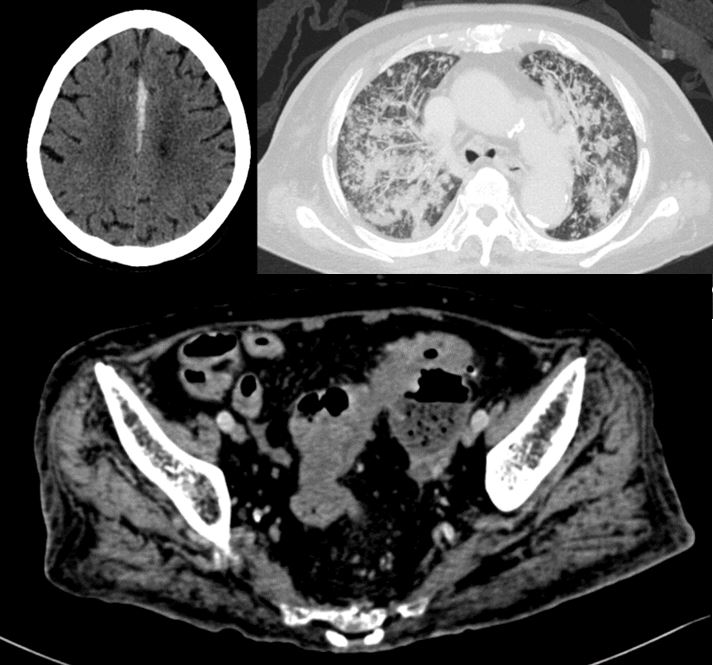
Figure 2: Computed tomography (CT) imaging of (a) the brain, revealing inter-hemispheric hyperdensity consistent with a subdural haematoma, (b) the thorax, revealing extensive bilateral lung consolidation and reticulonodular opacities, predominantly in upper lobes, and (c) abdomen, showing sigmoid colon diverticulitis with a rim-enhancing collection adjacent to the posterior aspect of the proximal-to-mid sigmoid colon (2.9 x 2.6 x 2.6 cm).
Following consultation with our Infectious Disease team, the patient was treated for likely disseminated nocardiosis using intravenous trimethoprim/sulfamethoxazole as a recommended first line therapy. Unfortunately, following 72 hours of trimethoprim/sulfamethoxazole administration, the patient developed severe pancytopenia (haemoglobin 63 g/L, white cell count 2.0 x 109/L and platelets 33 x 109/L) requiring packed red cell and platelet transfusions, as well as immediate cessation of trimethoprim/sulfamethoxazole. Further decisions on antimicrobial proved difficult as it was noted that other effective alternatives against nocardiosis, including amikacin and fluoroquinolones may potentially exacerbate MG symptoms. Furthermore linezolid, another possible alternative, could potentially exacerbate her thrombocytopenia and worsen the pre-existing subdural haematoma. Thus, a decision was made to commence co-amoxiclav and meropenem concurrently despite neither being first-line therapy. The patient subsequently had an uneventful CT-guided drainage of the sigmoid abscess, with the assistance of our General Surgical colleagues, and was kept on prolonged intravenous antibiotic therapy for 3 months. Following improvement in clinical state, she was allowed discharge from hospital with ongoing oral co-amoxiclav and linezolid with regular bloods tests to monitor for myelosuppression as an outpatient, which has not occurred till this date. With support from clinical and radiological improvement, we aim for 12 months of therapy.
Discussion
Various cases of nocardia sp bacteraemia have been reported, in which immune system dysfunction was primarily due to chronic glucocorticoid therapy 1 3 4. A retrospective review of 40 patients from a Chinese tertiary hospital revealed that half of patient with nocardiosis were on corticosteroids prior to infection onset 5. An even larger case series reported up to 94% of pulmonary nocardial infection being linked to use of immunosuppressants 6.
Management of nocardiosis can be challenging. Often, imipenem, trimethoprim/sulfamethoxazole, amikacin or a combination of these antibiotics are recommended, with treatment duration being guided by clinical and radiological improvement often extending up to a year 7. Bactericidal agents including carbapenems and amikacin are often recommended alongside trimethoprim/sulfamethoxazole in cases of disseminated nocardiosis to ensure greater success in treatment 7, 8. The use of amikacin however should be cautioned in cases of MG, and reports have described management using linezolid as an alternative 1, 9.
In our patient, the risk of worsening pancytopenia as illustrated following trimethoprim/sulfamethoxazole administration led to hesitance in using linezolid. Furthermore, the consequences of thrombocytopenia would have been devastating for the patient due to having residual subdural hematoma. Thus, the choice of antibiotics was limited to that of second-line agents including co-amoxiclav and meropenem on top of surgical drainage of existing abscesses, which has also been shown to be beneficial 1 5. However, it should be noted that the risk of pancytopenia remains to be multifactorial in our patient, ranging from pre-exisitng myelosuppression to ongoing sepsis and initiation of culprit medications
Mortality of nocardiosis infections ranges depending on organ involved, rates being under 40% in cases of pulmonary spread, and up to 100% when disseminated to the central nervous system (CNS) 6. Unfortunately, nocardia farcinica, the subtype reported in our case, has been shown to be more resistant to antimicrobials and carries a greater risk of dissemination to the CNS, a point being greatly considered as our centre continues to manage the patient 10.
Conclusion
Nocardiosis, although not uncommon in immunocompromised individuals, poses a unique challenge in the MG population due to limitations in suitable antibiotics. Our case highlights the importance of a multi-disciplinary approach, involving various specialties including the infectious disease, neurology, general surgical and microbiology to ensure successful management of such complex cases.
|
Acknowledgements The authors would like to acknowledge Universiti Teknologi MARA (UiTM) for supporting the submission of the following article. Competing Interests None declared Author Details RAJA SHARIFF REF, MRCP, Universiti Teknologi Mara Sungai Buloh, Selangor, Malaysia. SAPUAN S, MMED, Hospital Sungai Buloh, Selangor, Malaysia. CORRESPONDENCE: RAJA SHARIFF REF, MRCP, Universiti Teknologi Mara Sungai Buloh, Jalan Hospital, 47000, Sungai Buloh, Selangor, Malaysia. Email: rajaezman@gmail.com |
References
- El-Herte RI, Kan SS, Araj GF, Chami H & Gharzuddine W. First Report of Nocardia Asiatica Presenting as an Anterior Mediastinal Mass in a Patient with Myasthenia Gravis: A Case Report and Review of the Literature. Case Reports in Infectious Diseases 2012; 2012, Article ID 325767.
- Garcia RR, Bhanot N, Min Z. A mimic’s imitator: a cavitary pneumonia in a myasthenic patient with history of tuberculosis. BMJ case reports 2015, bcr2015210264. doi:10.1136/bcr-2015-210264.
- Uneda A, Suzuki K, Okubo S, Hirashita K, Yunoki M, et al. Brain abscess caused by Nocardia asiatica. Surg Neurol Int 2016; 7(74): 1-4.
- Jeong JH, Moon SM, Park PW, Ahn JY, Kim KH, et al. Multiple Brain Abscesses Caused by Nocardia asiatica in a Patient With Systemic Lupus Erythematosus: The First Case Report and Literature Review. Ann Lab Med 2017; 37: 459-461.
- Yang M, Xu M, Wei W, Gao H, Zhangi X, et al. Clinical findings of 40 patients with nocardiosis: A retrospective analysis in a tertiary hospital. Experimental and Therapeutic Medicine 2014; 8: 25-30.
- Martnez TR, Menedez VR, Reyes CS, Santos DM, Vallés TJM, Modesto AM, et al. Pulmonary norcadiosis: Risk factors and outcomes. Respirology 2007; 12: 394-400.
- Ambrosioni J, Lew D & Garbino J. Norcadiosis: Updated clinical review and experience at a tertiary center. Infection 2010; 38: 89-97.
- Brown-Elliott BA, Brown JM, Conville PS & Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev 2006; 19: 259–282.
- Kosuke T, Miki N, Masaki Y, Yasufumi M, Hayato T, et al. Disseminated Nocardia farcinica infection in a patient with myasthenia gravis successfully treated by linezolid: a case report and literature review. Journal of infection and chemotherapy 2012; 18(3): 390-394.
- Anagnostou T, Arvanitis M, Kourkoumpetis TK, Desalermos A, Carneiro HA, et al. Nocardiosis of the central nervous system: Experience from a general hospital and review of 84 cases from the literature. Medicine 2014; 93: 19 32.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




