Diagnosis and Management of Stable COPD
Katerina M Achilleos and Duncan J Powrie
Cite this article as: BJMP 2011;4(3):a427
|
Chronic obstructive pulmonary disease (COPD) is a debilitating condition resulting in significant morbidity and mortality. It is the fifth leading cause of death in the UK 1, estimated to be the third by 2020 2.
Definition:
- COPD is a preventable and treatable disease with some extra-pulmonary effects that may contribute to the severity in individual patients Its pulmonary component is characterised by airflow limitation that is progressive and not fully reversible. There is an abnormal inflammatory response of the lung to noxious gases and particles, most commonly cigarette smoke 3.
- Airflow obstruction is defined as post-bronchodilator FEV1/FVC ratio (where FEV1 is the forced expiratory volume in one second and FVC is the forced vital capacity) of less than 0.7 If FEV1 is ≥ 80% predicted, a diagnosis of COPD should only be made in the presence of respiratory symptoms 4.
Incidence/ Prevalence:
Within the UK it is estimated that 3 million people are affected with COPD 4. However, only 900,000 are diagnosed -4An estimated two million people who have COPD remain undiagnosed 4.
Causes:
90% of cases are smoking related 4, particularly those with >20 pack year smoking histories 5. Environmental and occupational factors can also play a role, including exposure to biomass fuels such as: coal, straw, animal dung, wood and crop residue which are used to cook in some countries and heat poorly ventilated homes COPD occurs in 10-20% of smokers, suggesting there is an element of genetic susceptibility 2-3, 5.
Diagnosis:
To make a diagnosis of COPD an obstructive deficit must be demonstrated on spirometry in patients over the age of 35 years with risk factors (mainly smoking) and signs and symptoms of the disease 4.
Signs and Symptoms:
- Progressive dyspnoea on exertion
- Chronic cough
- Chronic sputum production
- Wheeze
- Frequency of exacerbations – particularly during winter months 4
- Functional status – bearing in mind gradual progression of disability, effort intolerance and fatigue.
-
Features suggestive of Cor pulmonale 5:
- Peripheral oedema
- Elevated jugular venous pressure
- Hepatomegaly
- Right ventricular heave
- Tricuspid regurgitation
Investigations/ Tests to consider:
-
Post-bronchodilator Spirometry – essential in confirming the diagnosis of COPD.
- Demonstrating an obstructive picture.
- FEV1 is used to assess the progression and severity of COPD, but correlates poorly with the degree of dyspnoea 3-6. (Table 1)
-
Pulmonary functions tests – Markers suggesting the presence of emphysema include:
- Reduced TLCO and KCO due to a reduced surface area for gaseous exchange 5.
- Raised Total lung capacity, residual volume and functional residual capacity due to air trapping 5.
-
Chest radiograph – Is not required for the diagnosis, but is recommended to exclude other conditions such as interstitial lung disease, pleural effusions or pneumothorax. It may demonstrate features of the condition, such as 3, 5:
- Hyperinflated lung fields
- Flattened diaphragms
- Bullous changes, particularly at the apices
-
BODE index prognostic indicator – This is grading system shown to be better than FEV1 at predicting the risk of hospitalisation and death in patients with COPD. Patients are scored between 0 and 10, with higher scores having an increased risk of death. It encompasses 3, 5-7: (Table 2)
- BMI
- Airflow Obstruction – taking into account the FEV1
- Dyspnoea – in accordance with the Medical Research Council (MRC) scale 5.
- Exercise capacity – measured by the distance walked in 6 minutes. (Table 3)
Table 1. Severity of airflow obstruction 4
| Stage | Severity post-bronchodilator | FEV1 (%) Predicted | Comments |
| 1 | Mild | ≥ 80% | Only diagnosed in the presence of symptoms |
| 2 | Moderate | 50- 79% | Managed within the community |
| 3 | Severe | 30-49% |
TLCO usually Low Hospitalization may be needed only with exacerbations |
| 4 | Very Severe | <30% | Or FEV1 <50% with respiratory failure |
Table 2. BODE Index 3, 5-8
| 1 | 2 | 3 | ||
| FEV1 Predicted (%) | ≥ 65 | 50- 64 | 36- 49 | ≤ 35 |
| Distance walked in 6 minutes (meters) | ≥ 350 | 250- 349 | 150- 249 | ≤ 149 |
| MRC dyspnoea scale | 0-1 | 2 | 3 | 4 |
| BMI | ≥ 21 | ≤ 21 |
Table 3. Medical research council (MRC) Dyspnoea scale 5, 8
| 1 | Dyspnoeic only on strenuous activity |
| 2 | Dyspnoeic on walking up a slight incline or when hurrying |
| 3 | Walks slower than contemporaries on the flat, or has to stop for breath, or has to stop for breath when walking at own pace |
| 4 | Stops for breath on walking 100m or after a few minutes on walking on the flat |
| 5 | Breathless on minimal exertion e.g. dressing/ undressing. To breathless to leave the house |
Differential Diagnosis:
-
Asthma – the most important differential diagnosis to consider.
- This is steroid and bronchodilator responsive
- Indicative of reversible airway obstruction.
- It is not associated with smoking.
- Patients with asthma may exhibit 3, 9: chronic non-productive cough, variability in breathlessness, diurnal /day-to-day variation, nocturnal wheeze and dyspnoea
- However both conditions may coexist creating diagnostic uncertainty.
-
Alpha1 antitrypsin deficiency is an autosomal dominant condition associated with an increased risk of developing emphysema at an early age 3, 5, 9.
- It can occur in non-smokers
- Can be asymptomatic and thus under-diagnosed with an estimated 1 in 2000-5000 individuals being affected 5.
- The disease is worse in smokers
- COPD can develop in patients < 35years of age
- It is associated with liver cirrhosis.
- All patients with COPD should be screened.
- Emphasis should be made to avoid smoking, including passive smoking.
-
Other conditions to consider include:
- Bronchiectasis
- Interstitial lung disease
- Cardiac failure.
Treatment:
Goals of management include:
- Early and accurate diagnosis
- Improve symptoms and quality of life
- Reduce the number of exacerbations
- Improve mortality
Non-pharmacological management:
- Smoking cessation – an accurate smoking history should be obtained, including the number of pack years smoked. All current smokers with COPD should be encouraged to stop at every opportunity, and offered smoking cessation advice. Advising the patient alone will help a certain proportion to stop, whilst referral to smoking cessation services has been shown to further increase in quit rates. There are a range of nicotine and other pharmacological therapies available such as Bupropion (Zyban®) and Varenicline (Champix®) 3-4, 7, 8.
- Vaccinations – A once off Pneumococcal and annual Influenza vaccine should be offered.
-
Pulmonary rehabilitation – Should be offered to patients who have had a recent exacerbation requiring hospitalisation and those that have an MRC score of ≥ 3, but are still able to mobilise and thus have the potential for further rehabilitation. It is not suitable for those patients that are immobile or limited in their mobility due to symptoms of unstable angina or a recent cardiac event. Benefits are seen in terms of reduced hospital admission, improved quality of life and exercise tolerance Commitment to the programme should be relayed to the patient, and each programme should be tailored to their individual needs. This usually includes 3-5:
- Disease education – which can improve the ability to manage their illness.
- Exercise – tailored programmes to prevent de-conditioning and improve functional exercise capacity, dyspnoea and quality of life 4. This includes strength and endurance training of upper limbs and respiratory muscles Benefits may be seen even after 6 months.
- Physiotherapy – to teach active cycle breathing techniques or to use positive expiratory pressure masks in patients with excessive sputum production.
- Nutritional support – in the form of supplementation or dietician advice in patients with a suboptimal BMI. A low BMI is associated with increased mortality as it is associated with poor exercise capacity, reduced diaphragmatic mass and impaired pulmonary status. Alternatively, weight loss is recommended in patients who are in the obese range.
- Psychological – Assessment for support at home, introduction of patients to day centres, assessing for features of depression and anxiety, and aiding in the obtainment of a car disability badges may require referral to occupational therapy and social services.
- Travel advice – Patients who are planning air travel and have FEV1 <50%, Sa02 < 93%, or are on long term oxygen therapy (LTOT) should undergo formal assessment -4Patients with bullous disease should be informed that they are at increased risk of pneumothorax during high altitude flights 4.
Pharmacological management:
-
Bronchodilators – Provide long term benefit in reducing dyspnoea. This is not reflected in improvements in FEV1 as it may not show reversibility 4.
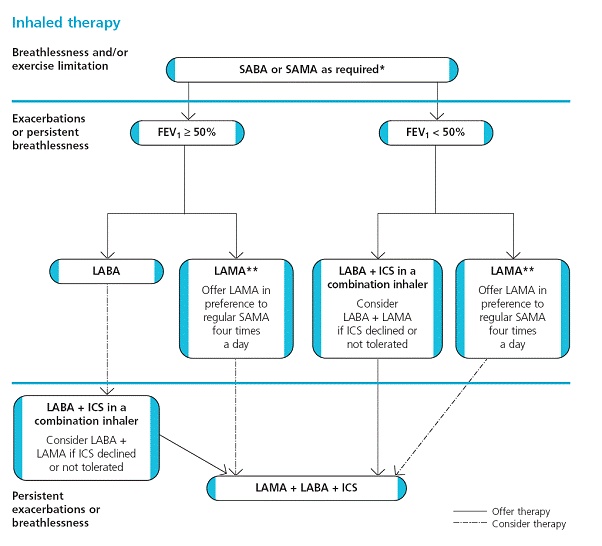
- Start with an inhaled SABA (short-acting beta2-agonist) or a SAMA (short-acting muscarinic antagonist) on an as required basis for symptomatic relief. If symptoms remain despite regular SABA therapy (i.e. four times a day), then treatment will need to be stepped up.
- If symptoms persist or if the patient is having recurrent exacerbations add in a LABA (long-acting beta2 agonist) or a LAMA (long acting muscarinic antagonist).
- If symptoms continue, add in a LAMA if already on a LABA (or vice versa).
- If FEV1 <50% add in an inhaled corticosteroid (ICS). This can be offered as a combination inhaler.
Inhaled therapy should offer sufficient bronchodilator response. A spacer can be used for those with poor technique. Nebulisers are reserved for patients who demonstrate respiratory distress despite maximal inhaled therapy, and for those that show an improvement in symptoms or exertional capacity 4.
Diagram 1: Summary of step-by-step management 4
- Corticosteroids – A short course of oral steroids may be used during exacerbations. A maintenance course however is not recommended Any patients on long term steroids should be weaned off.
- Mucolytic agents – May be considered in patients with a chronic cough who have difficulty expectorating. They should only be continued if symptomatic benefit is evident, otherwise they can be stopped. There is no evidence to show that they reduce the exacerbation frequency.
- Theophylline – Should only be offered in people that are unable to use inhaled therapy or after trials of SA and LA bronchodilators 4. The same generic brand should be prescribed as individual brands will have different efficacy. It is usually used as an adjunct to beta2-agonists and muscarinic antagonists. Interactions with macrolides and fluroquinolones and other drugs are also common, and as such the theophylline dose should be reduced if interactions are known. Caution should be taken in prescribing theophylline in the polypharmacy patient 3, 5. Little evidence has been shown to support theophylline usage in COPD (compared to asthma), however it is used for its anti-inflammatory effects As such levels are only performed if toxicity is suspected and should not be adjusted if in the sub-therapeutic range.
-
Oxygen therapy – Patients should be assessed for long-term oxygen therapy (LTOT) if they exhibit 4:
- Severe airflow obstruction
- Features of Cor pulmonale
- Hypoxaemia (Sa02 ≤ 90%)
- Cyanosis
- Polycythaemia
Patients with stable COPD who are receiving maximum medical therapy are assessed by measuring arterial blood gases taken on two separate occasions at least 3 weeks apart. To meet the criteria patients must have 4:
- A Pa02 < 7.3 kPa when stable, or
-
A Pa02 >7.3 but < 8.0 kPa when stable and:
- Pulmonary hypertension or
- Peripheral oedema or
- Secondary polycythaemia or
- Nocturnal hypoxaemia
LTOT should be used for a minimum of 15L per day, including during sleep 3-4.
Patients who continue to smoke should be made aware of the serious risk of facial injuries due to the highly flammable nature of oxygen.
When to refer:
Referrals for specialist advice or specialist investigations may be appropriate at any stage of the disease.
Other possible reasons for referral 4
| § Diagnostic uncertainty | § Suspected severe COPD |
| § Onset of Cor pulmonale | § Rapid decline in FEV1 |
| § Assessment for LTOT, home nebulisers or oral corticosteroid therapy | § Symptoms that do not correlate to lung function deficit |
| § Pulmonary rehabilitation assessment | § Frequent infective exacerbations |
| § Family history of alpha-1-antitrypsin deficiency | § Haemoptysis |
| § Onset of symptoms < 40 years | § Bullous lung disease |
| § Assessment for lung volume reduction surgery/ lung transplantation | § Dysfunctional breathing |
Follow-up:
Patients with stable mild-moderate COPD should be reviewed by their general practitioner at least once a year and those with severe COPD twice yearly.
At each visit 4:
- An opportunity should be taken to ask about their current smoking status and the desire to stop.
- Assessment of adequate control of symptom: dyspnoea, exercise tolerance and the estimated number of exacerbations per year.
- Assessment of inhaler technique.
- To assess the effects/side effects of each drug treatment.
- The need for pulmonary rehabilitation.
For those patients with very severe airflow obstruction (FEV1 < 30%), the above still remains, in addition to the assessment of 4:
- Features of Cor pulmonale
- Nutritional status
- The need for LTOT
- Signs of depression
- The need for occupational therapy and social services input
- Referral to specialist and their services
-
Measurements of:
- FEV1 and FVC
- BMI
- MRC dyspnoea scale
- Sa02 via pulse oximetry
Those patients requiring long term non-invasive ventilation will be reviewed by a specialist on a regular basis.
Patient Information:
§ www.patient.co.uk/health/Chronic-Obstructive-Pulmonary-Disease.htm
§ www.lunguk.org/you-and-your-lungs/conditions-and-diseases/copd
§ http://smokefree.nhs.uk/ways-to-quit
|
Competing Interests None declared Author Details KATERINA M ACHILLEOS, MBBS BSc (Hons), Southend University Hospital, Prittlewell chase, Westcliff-on-sea, SS0 0RY DUNCAN J POWRIE, MB ChB, Consultant Respiratory Physician, Heart and chest clinic, Southend University Hospital, Prittlewell chase, Westcliff-on-sea, SS0 0RY CORRESPONDENCE: KATERINA M ACHILLEOS, ST1 Respiratory Medicine, Southend University Hospital, Prittlewell chase, Westcliff-on-sea, SS0 0RY Email: katerina.achilleos@southend.nhs.uk |
References
1. National statistics (2006) Health Statistics Quarterly 29.
2. European Respiratory society (2003) European White Lung Book.
3. Global Strategy for Diagnosis, Management, and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines 2010.
4. Chronic obstructive pulmonary disease. Management of chronic obstructive pulmonary disease in adults in primary and secondary care. NICE guidelines 2010.
5. Chapman S, Robinson G, Straddling J, West S. Oxford handbook of respiratory medicine, 2e, Oxford university press, 2009
6. Celli BR. Update on the management of COPD. Chest 2008;133:1451-1462.
7. Celli BR, et al. The Body-Mass Index, Airflow Obstruction, Dyspnea, and Exercise Capacity Index in Chronic Obstructive Pulmonary Disease. NEJM 2004; 350: 1005-12.
8. Todd DC et al. Approach to chronic obstructive pulmonary disease in primary care. Can Fam Physician 2008; 54:706-11.
9. Celli BR, MacNee W et al. Standards for the diagnosis and treatment of patients with COPD. A summary of the ATS/ESR position paper.Eur Respir J 2004; 23: 932–946
10. Barnes PJ. Theophylline for COPD. Thorax 2006; 61: 742-743.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




