Content and Timing of Inpatient Discharge Summaries at the Mount
Abhishek Shastri, Santosh Bangar, Shoshanah Waldman, Elham Esfahani and Nick Brindle
Cite this article as: BJMP 2014;7(3):a726
|
|
Abstract Aim: The discharge summary is a vital component of patient care. It is a means by which information is conveyed to clinicians and community mental health team who will be involved in follow-up patient care. This calls for accuracy as well as completeness of information as these are vital components that can directly impact patient care. Timing of discharge letter/summary reaching the follow-up physician, general practitioner or community mental health team, from point of discharge can also play a key role in patient management. This audit looks at the content and timing of discharge summaries from The Mount, Old Age Psychiatry hospital as to whether it adheres to the local Trust guidelines. Methods: Discharge summaries from electronic database were reviewed. In cycle 1 of the audit, adherence to local Trust guidelines in relation to the content, accuracy and timing of discharge summaries were studied. In the follow-up audit cycle, changes in clinical practice brought about following recommendations were studied. Results: Recommendations and feedback were found to be effective in significantly improving adherence to inclusion of family history (p<0.001), social history (p<0.001), premorbid history (p=0.036), progress and treatment during hospital stay (p=0.049) in the discharge summary. Significant decrease was observed in inclusion of follow-up arrangements (p=0.007). Other significant improvements included lesser spelling errors (p<0.001), dictation (p<0.001) and typing (p<0.001) of discharge letter within 5 working days of discharge of patient. Conclusions: This study adds to importance of accuracy and timing of discharge summaries to ensure good medical practice and continuity of care. It also establishes scope for improvement and recommendations that can further improve clinical practice. Furthermore, key decisions on patient care can be made by follow-up health professionals, at the earliest and with the help of appropriate information. |
Introduction
The discharge summary is an integral part of continuing patient care. Apart from containing vital information regarding current admission, it also conveys key findings and plans to clinicians who will be taking over the care of the patient. This would mean communicating important information about patients to ensure appropriate and safe follow-up management. Studies involving discharge summaries have looked into role of communication from secondary to primary care and have highlighted the importance of accuracy and quality of information,1 errors2 and general practitioner (GP) preference.3 Systematic reviews have found low availability (12-34%) of discharge summary during first visit post-discharge as well as wide variations in content of discharge summaries thereby directly affecting patient management.4,5 The timing of discharge summary completion and reaching the follow-up physician is therefore of prime importance wherein this has been also found to influence and reduce the risk of rehospitalisation.6 The content necessary for a ‘good’ or ‘high-quality’ discharge summary has been studied via surveys. The inclusion of important data such as diagnosis, discharge drugs, complications, laboratory results and follow-up plans have been considered to be important clinical information by hospital physicians and GPs.7
Hospital discharge summaries can be hand-written, dictated or in electronic format. These formats have their benefits and downfalls. Hand-written summaries have been found to be well-accepted by primary care physicians although involve the factor of legibility.8 A randomised-controlled trial found no difference between electronic and dictated discharge summaries for primary care physician satisfaction.9 Although the use of electronic discharge summaries has significantly improved both the content and timing of discharge summaries reaching follow-up physician or healthcare staff,10 they have been found to contain higher number of errors in patient progress, additional diagnosis and free-text components.11
This audit examined the timing and content of discharge summaries at The Mount and whether they met local Trust standards. A follow-on audit was conducted to study the impact of recommendations that had been put forward at the end of Cycle 1 of the audit.
Aim and Objectives
Aim
Cycle 1: To study the content, accuracy and timing of discharge summaries at The Mount, Old Age Psychiatry hospital.
Cycle 2: To examine changes in clinical practice following recommendations from Cycle 1 of audit involving content and timing of discharge summaries from The Mount.
Objectives
Cycle 1: To ascertain whether Trust guidelines regarding content of discharge summaries are met and also whether the timeline guidance is being maintained.
Cycle 2: To examine adherence to the Trust guidelines as well as to study the changes brought about by recommendations at the end of Cycle 1.
Criteria/ Standards
Trust guidelines state:
- Discharge summaries must be typed and sent in 5 working days post-discharge from hospital.
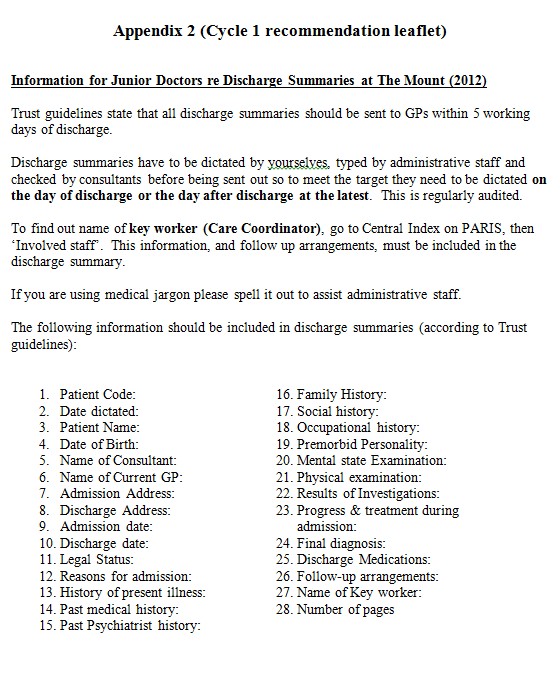
- They must include the following information (Box 1):
Box 1 Trust guidelines for inclusion of information in discharge summaries
|
Method
Audit Sample
Patients admitted and discharged from Ward 3 & 4 of The Mount, between 01.04.2011 to 31.10.2011. A total of 103 patient discharge summaries were therefore analysed in Cycle 1 of the study. For cycle 2, the audit sample comprised of patients admitted and discharged from Ward 3 & 4 of The Mount, between 01.04.2012 to 31.10.2012. A total of 97 patient discharge summaries were therefore analysed in this part of the study.
Data Collection
Data was collected using an anonymous data collection tool (Appendix 1) which was designed according to Trust guidelines. Administrative staff provided the clinical audit leads with list of patients discharged during the study dates. The electronic patient record system of the Trust (PARIS: Patient Record Information System) was used to study the discharge summary letters. Data collection was performed under the supervision of consultant responsible for the audit, between November 2011 and January 2012 for cycle 1 and for cycle 2 data collection was performed between October 2013 and November 2013. Patient confidentiality and anonymity was maintained.
Data Analysis
Qualitative data was gathered, coded and collated on to a Microsoft Excel spread sheet. The data collected was reviewed by the authors to ensure each aspect of data collection tool was filled. The data was analysed by the Clinical Audits Facilitator at the Trust Clinical Audit Support Team and placed into a report format for dissemination.
Results
The number of discharge summaries analysed in Cycle 1 and 2 of this study was 103 and 97 respectively.
Data were collected using the data collection tool (appendix 1). Dates of discharge, dictation and typing were recorded. Date of typing was used as a proxy of date sent to GP since there was no record of this. Seven days were permitted for discharges to be sent (equivalent to 5 working days). Discharge summaries were read and it was recorded if each stipulated heading from the Trust guidelines was present. No comment was made on quality of information; only consideration was whether information was present or absent.
Compliance with each point from the above categories is shown in the following series of tables and comparison is made between the studies in Cycles 1 and 2 (Table 1-4). The statistical significance of the differences found in the two audit cycles was evaluated using chi-square tests.
| Table 1 Presence of information on discharge summary according to Trust guidelines | |||
| Criteria | Adherence % 2011 (n=103) | Adherence % 2013 (n=97) | Statistical significance |
| Patient code | 100% (n=103) | 97% (n=94) | p=0.721 |
| Date dictated | 72% (n=74) | 98% (n=95) | p<0.001 |
| Patient Name | 100% (n=103) | 100% (n=97) | No change |
| Date of birth | 97% (n=100) | 100% (n=97) | p=0.090 |
| Name of consultant | 98% (n=101) | 99% (n=96) | p=0.596 |
| Name of current GP | 98% (n=101) | 98% (n=95) | No change |
| Admission address | 98% (n=101) | 100% (n=97) | p=0.167 |
| Discharge address | 98% (n=101) | 100% (n=97) | p=0.167 |
| Admission date | 97% (n=100) | 100% (n=97) | p=0.090 |
| Discharge date | 97% (n=100) | 99% (n=96) | p=0.342 |
| Legal status | 99% (n=102) | 98% (n=95) | p=0.525 |
| Reasons for admission | 98% (n=101) | 98% (n=95) | No change |
| History of present illness | 100% (n=103) | 99% (n=96) | p=0.301 |
| Past medical history | 89% (n=92) | 95% (n=92) | p=0.150 |
| Past psychiatric history | 95% (n=98) | 98% (n=95) | p=0.282 |
| Family history | 19% (n=20) | 86% (n=83) | p<0.001 |
| Social history | 56% (n=58) | 89% (n=86) | p<0.001 |
| Occupational history | 67% (n=69) | 68% (n=66) | p=0.873 |
| Premorbid history | 37% (n=38) | 52% (n=50) | p=0.036 |
| Mental health examination | 95% (n=98) | 93% (n=90) | p=0.482 |
| Physical examination | 86% (n=89) | 92% (n=89) | p=0.227 |
| Results of investigations | 84% (n=87) | 78% (n=76) | p=0.265 |
| Progress & treatment during admission | 96% (n=99) | 100% (n=97) | p=0.049 |
| Final diagnosis | 92% (n=95) | 97% (n=94) | p=0.147 |
| Discharge medications | 98% (n=101) | 97% (n=94) | p=0.602 |
| Follow-up arrangements | 86% (n=89) | 79% (n=77) | p=0.007 |
| Name of key worker | 64% (n=66) | 56% (n=54) | p=0.225 |
| Number of pages | 0% (n=0) | 0% (n=0) | No change |
| Are there any spelling/typing errors in the list of medications? | 90% (n=8) | 98% (n=2) | p=0.064 |
| Are there any spelling/typing errors in the diagnosis and medical terminology? | 78% (n=21) | 99% (n=1) | p<0.001 |
Table 1: The presence of information mentioned in the Trust guidelines is analysed. The percentage adherence in cycle 1 is compared with findings from cycle 2. Significant increase in inclusion of family history, social history, follow-up arrangements and date of dictation is observed. A healthy increase is also observed in inclusion of premorbid history and progression and treatment during admission. A significant reduction in spelling/typing errors is also seen. The decrease in inclusion of name of key worker, discharge medications, mental health examination and results of investigation amongst others is also noted. GP, general practitioner.
The comparison of findings from Cycle 1 and 2 establish a significant increase in adherence to family history (p<0.001), social history (p<0.001), premorbid history (p=0.036) as well as progress and treatment during hospital stay (p=0.049) components of the discharge summary. There was also a significant increase in inclusion of date of dictation of discharge summaries (p<0.001). Increase in adherence to most of the components of discharge summaries was observed. However, there was significant decrease in inclusion of follow-up arrangements (p=0.007) as well as a decrease in inclusion of name of key-worker assigned to patient (from 64% in cycle 1 to 56% in cycle 2; p=0.0225). A significant decrease in spelling/typing errors in diagnosis or medical jargon was observed (p<0.001).
Timing of Discharge Summaries
| Table 2 Time taken between discharge of patient and dictation of letter | |||
| Days | Adherence % 2011 (n=74) | Adherence % 2013 (n=94) | Statistical significance |
| 0-7 | 30% (n=22) | 73% (n=69) | p<0.001 |
| 8-15 | 24% (n=18) | 22% (n=21) | p=0.762 |
| 16-22 | 18% (n=13) | 4% (n=4) | p=0.004 |
| 23+ | 29% (n=21) | 0% (n=0) | p<0.001 |
Table 2: The time taken between discharge of patient and dictation of letter is analysed. A significant increase is observed in the dictation of letter as per Trust guidelines (within 5 working days).
| Table 3 Time taken between dictation and typing of discharge letter | |||
| Days | Adherence % 2011(n=75) | Adherence % 2013 (n=94) | Statistical significance |
| 0-5 | 84% (n=63) | 73% (n=69) | p<0.001 |
| 6-11 | 7% (n=5) | 24% (n=23) | p=0.192 |
| 12+ | 9% (n=7) | 2% (n=2) | p<0.001 |
Table 3: The time taken between dictation of letter and typing of discharge letter is analysed. A significant decrease is observed in the time taken for typing of letter within 5 days of dictation of letter.
| Table 4 Time take between discharge and typing of discharge letter | |||
| Days | Adherence % 2011 (n=100) | Adherence % 2013 (n=96) | Statistical significance |
| 0-7 | 18% (n=18) | 52% (n=50) | p<0.001 |
| 8-15 | 32% (n=32) | 34% (n=33) | p=0.724 |
| 16+ | 60% (n=60) | 14% (n=13) | p<0.001 |
Table 4: The time taken between discharge of patient and typing of discharge letter is analysed. A significant increase is observed in the early typing of discharge letter from the date of discharge of patient.
The number of discharge summaries being dictated and typed within 7 days of discharge was significantly increased (p<0.001) and a significant decrease in discharge letters being dictated more than 2 weeks (p=0.004) or 3 weeks (p<0.001) of patient being discharged was observed. The time taken between dictation of letter and it being typed up was also found to have dropped, with 73% being done within 7 days, significant decrease (p<0.001) being observed since the first cycle. Furthermore, a significant increase is observed in early (less than 7 days) typing of discharge letter since patient being discharged (p<0.001).
Discussion:
The discharge summary is a very important means to communicate medical (both physical and psychiatric) and nursing interventions to the GP or community mental health team. This in turn helps in making invaluable decisions to patient care in the community. Hence, it is worth spending time on doing a good discharge letter which includes relevant information. A timely discharge letter can also be very useful in this regard.
At the end of Cycle 1 of the audit, recommendations that were made included (Appendix 2):
- Disseminating information amongst all junior doctors, consultants and administrative staff on each ward to include the above mentioned headings in accordance with Trust guidelines.
- Information was also provided regarding finding out Name of Keyworker in PARIS system.
- A specific note was also placed regarding to spell out medical terminologies that would assist in the typing of discharge summaries by administrative staff.
From the results, it is evident that the content of the discharge summary has largely been maintained. In other words, good practice was maintained and recommendations from previous audit were implemented in most spheres of discharge letters. However, despite the recommendation of finding out name of key-worker from PARIS system, there was a decrease (from 64% in first cycle to 56% in second cycle) in its inclusion (p=0.225). Thus, training in usage of information technology system is essential. Providing appropriate instruction and training to junior doctors has been found to be useful in improving the quality of discharge summaries.12 Therefore, it might be beneficial to include instructions or guidelines for appropriate discharge summaries at local Trust or departmental inductions. This will help junior doctors in ensuring completion of accurate and succinct discharge summaries that will aid in patient management.
There was a reduction in documentation of discharge medication, follow up arrangement, mental state examination and physical health investigation carried out as an in-patient. This certainly needs improving as these are the relevant areas to facilitate smooth transition of care in the community and follow-up arrangement. With regard to the timing of the discharge summary, this was found to have significantly improved from the previous audit cycle. For example, the timing between discharge and dictation (within 7 days) has increased from 30% to 73% and almost all discharge summaries are dictated no later than 3 weeks. The possible reasons for delays in dictation could be ongoing workload, availability of medical staff and of the medical notes, as these are sometimes requested by the Intermediate Community Service (ICS) team. There was a slight drop in the time between dictation and typing (from 84% to 73%), which could possibly due to availability of administrative staff, dictation tapes or medical notes and proof reading by medical staff. Significant increase was observed in inclusion of date of dictation of discharge summaries which will be a useful component for future audits. A significant decrease in spelling/typing errors in diagnosis or medical terminologies was observed. Furthermore, there was significant increase in inclusion of family history, social history, premorbid history as well as information on progress and treatment during hospital in the discharge summary. Therefore, timely audit and feedback can be very useful in improvement of discharge summaries and patient care.
Recommendations & Actions:
- Raise awareness amongst senior house officers (SHO’s) and other doctors in the Trust regarding recording of pre-morbid history, occupational history, name of keyworker as this was only done in 52%, 62%, 56% cases respectively. This could be done by disseminating findings from this audit amongst SHO’s and other doctors of Trust through hand-outs to wards as well as through local teaching session.
- Remove number of pages from the list of sub-headings needed in discharge summary as this is dependent on typing and not necessarily possible to estimate while dictating discharge summary. However, it is an important part of discharge summary. Therefore, send information with audit findings to medical secretaries informing the need to keep number of pages in the discharge summary.
- Consider adding a section on documentation of risk assessment should be included in the discharge summary as well as ‘early relapse signature’ which would enable early intervention in the community to avoid inpatient admission. This could be included in the discharge summary. This would involve liaising with consultants and the responsible person for making/printing discharge summaries for Trust.

|
Acknowledgements Dr Zoe Clough and Dr Alex Nalson for their help in data collection for Cycle 1 of this study. Dominik Klinikowski, Clinical Audit Facilitator at Leeds & York Partnership NHS Foundation Trust. Competing Interests None declared Author Details ABHISHEK SHASTRI, MBBS, PGDIP PSYCHIATRY, MPHIL, Foundation House Officer 2, The Mount, Leeds & York Partnership NHS Foundation Trust, Leeds, UK. SANTOSH BANGAR, MBBS, DPM, MD(Psychiatry), PGDip Clin Psy, MRCPsych (UK), ST 5 in Old Age Psychiatry, The Mount, Leeds & York Partnership NHS Foundation Trust, Leeds, UK. SHOSHANAH WALDMAN MBChB, BA, Core Trainee in Psychiatry, The Mount, Leeds & York Partnership NHS Foundation Trust, Leeds, UK. ELHAM ESFAHANI, MBBS, Core Trainee in Psychiatry, The Mount, Leeds & York Partnership NHS Foundation Trust, Leeds, UK. NICK BRINDLE, BSc (Hons), MB, ChB, MRCP (UK), MRCPsych (UK), Consultant Old Age Psychiatrist, The Mount, Leeds & York Partnership NHS Foundation Trust, Leeds, UK. CORRESPONDENCE: Dr Santosh Bangar, ST 5, Old Age Psychiatry, The Mount, 44 Hyde Terrace, Leeds LS2 9LN, United Kingdom. Email: santosh.bangar@nhs.net |
References
- Kazmi SMB. Quality of Electronic Discharge Summaries at Newham University Hospital: An Audit. Br J Med Pract 2008; 1:30-32.
- Crossan I Curtis D, Ong YL. Audit of psychiatric discharge summaries: completing the cycle. Psychiat Bull 2004; 28:329–331.
- Serfontein J, Dodwell D, Patel P. Psychiatric discharge summaries: what do general practitioners want? Mental Health in Fam Med 2011; 8:167-171.
- Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007; 297:831-841.
- Knai C, Doering N, Panteli D, et al. A systematic review of research on discharge summaries in Europe. Eur J Pub Health. 2013; 23: doi:10.1093/eurpub/ckt126.042.
- van Walraven C, Seth R, Austin PC, et al. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Int Med 2002; 17:186-192.
- van Walraven C, Rokosh E. What is necessary for high-quality discharge summaries? Am J Med Quality 1999; 14:160-169.
- Paterson JM, Allega RL. Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group. Can Fam Phy 1999; 45:2893-2899.
- Maslove DM, Leiter RE, Griesman J, et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Int Med 2009; 24:995-1001.
- O’Leary KJ, Liebovitz DM, Feinglass J, et al. Creating a better discharge summary: improvement in quality and timeliness using an electronic discharge summary. J Hosp Med 2009; 4:219-225.
- Callen JL, Alderton M, McIntosh J. Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Informatics 2008; 77:613-620.
- Myers JS, Jaipaul CK, Kogan JR, et al. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med 2006; 81 (suppl 10): s5-S8.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




