Comparing the use of traditional sites and alternative sites puncture for determination of blood glucose by glucometer
Crisafulli Cristiano, Massimo Catanuso, Carmelo Di Gregorio, Adriana Di Gregorio, Gaetano Profeta and Antonino Di Guardo
Cite this article as: BJMP 2015;8(4):a835
|
|
Abstract Self-monitoring of blood glucose (SMBG) is important in evaluating the efficacy of prescribed anti-hyperglycaemic therapies and can help the patient better understand the importance of achieving glycaemic control. Pain related to puncture of the fingertip, needed for determination of blood glucose, can notably reduce compliance of patients using self-monitoring devices. The use of glycated haemoglobin, while providing a measure of glycaemic control over the past 2-3 months, is an average of pre- and post-prandial glycaemia and does not take into account glycaemic variability, which is an important cardiovascular risk factor that can be assessed by SMBG. The search for sites as an alternative to the fingertip that are associated with less pain and good reproducibility and accuracy of blood glucose measurements is an area of growing interest. The present study enrolled 5 general practitioners and 70 patients with diabetes and without diabetes-related or neurological/vascular complications that could alter pain perception. Traditional and periungual puncture sites were assessed. In contrast to the fingertip, no pain was perceived at the alternative site, while there was no significant difference in the values of blood glucose obtained using traditional and alternative sites. Abbreviations: SMBG - Auto Monitoring Glycaemic, HbA1c - Haemoglobin glycated, VAS - Visual Analogue Scale |
The increasing collaboration between diabetologists and general practitioners (GPs) (e.g. the IGEA project) has resulted in the GP taking a more relevant role in management of patients with diabetes. Just as measurement of arterial blood pressure has become an important tool in follow-up of patients with hypertension by the GP, SMBG has become a valuable tool to evaluate glycaemic control. In particular, self-monitoring of both blood pressure and glycaemia are important to assess the efficacy of prescribed therapies, and can help the patient to better understand the importance of control of blood pressure and blood glucose.
Several instruments for measurement of blood pressure have been validated by important medical societies involved in hypertension, and much effort has been given to compliance and patient comfort. However, less attention has been dedicated to glucometers. In particular, little consideration has been given to patient compliance, and SMBG is often perceived as an agonising experience. Moreover, hourly pre-visit glucose curves for glycaemic control, even if important, do not have the same value as a standard control over 2 to 3 months between visits. In addition, after an initial period of "enthusiasm" the fear and hassle of pricking oneself and the unpleasant feeling of pain often cause the patient to abandon SMBG.
A literature search on PubMed using the term “self-measurement of blood glucose (SMBG) and pain” retrieved only two publications, demonstrating a general lack of interest of the medical community. However, SMBG can be of important diagnostic-therapeutic value. Pain related to skin pricks on the fingertip, needed for determination of glucometric blood glucose, can significantly reduce compliance to SMBG, thus depriving the physician of a useful tool for monitoring the efficacy of anti-hyperglycaemic therapy and glycaemic control. Moreover, HbA1c has clear limitations, even if it provides a good idea of glycaemic control over the past 2-3 months, as it is a mean value of pre- and post-prandial blood glucose. It does not, therefore, measure glycaemic variability, which is an important cardiovascular risk factor. Thus, more research is needed into puncture sites as an alternative to the fingertip that are associated with less pain, which could favour greater use of SMBG.
Another problem of significant importance concerns the reproducibility and accuracy of blood glucose measurements. In the traditional method, blood samples for self-monitoring are taken from the fingertip of any finger using a lancing device with a semi-rigid prick (Figs. 1 and 2). The large blood vessels in the derma of the fingertip (Fig. 3) are lanced, and a drop of blood is obtained for the glucometer. All lances are optimised to prick the skin at a depth greater than 0.5 mm with a variability of ± 0.2 mm (Fig. 4).

Figure 1. The fingertip as a traditional site of puncture using a lancet.
Figure 2. Traditional method for self-monitoring of blood glucose.
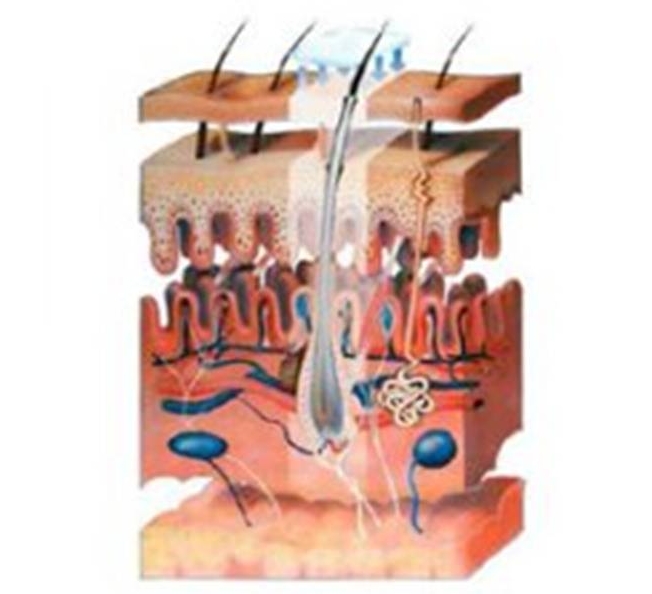
Figure 3. Vascularisation of derma.
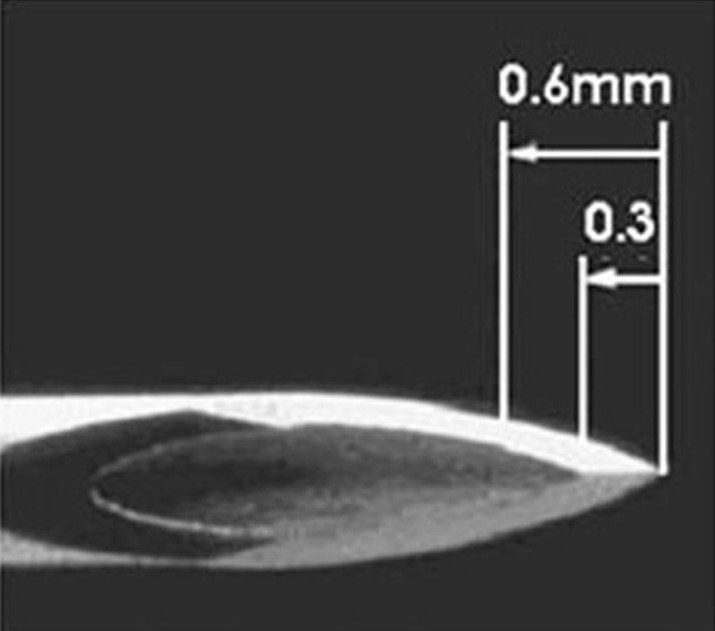
Figure 4. Traditional lancet.
Unfortunately, by pricking the fingertip at this depth, numerous tactile corpuscles in the dermis are also touched, causing the unpleasant sensation of pain. In a recent study by Koschinsky1 on around 1000 patients with type 1 (T1D) and type 2 diabetes (T2D), about one-half (51%) referred that they normally pricked themselves on the side of the fingertip because it is less painful. However, almost one-third (31%) used the centre of the fingertip, which is the site associated with the most pain. Other sites of puncture on the fingers are used much less frequently (5%), while 12% used other places on the body. It is also interesting to see how many times patients reused the lancet: 10% once, 19% for 2-4 times, 22% for 5-7 times, 25% for 8-10 times and 21% for more than 11 times. Pricking oneself 2 several times daily for years is not only troublesome for patients, but also leads to the formation of scars and callouses, and reduces fingertip perception and tactile sensitivity. Notwithstanding, alternative sites of puncture such as the arm, forearm and abdomen have not been evaluated in a systemic manner.
The objective of the present study is to compare alternative sites of puncture using a new semi-rigid lancet and determine if blood glucose values are similar to those obtained using traditional methods. A new puncture site was chosen, namely the area proximal to the nail bed of each finger. The sensation associated with puncture (with or without pain) was used to compare the two groups. Pain was assessed with a visual analogue scale (VAS). Blood glucose was measured in the morning after 12 hours of fasting.
Materials and methods
The present study enrolled 5 general practitioners and 70 patients with diabetes and without diabetes-related (micro-albuminuria, retinopathy, arterial disease of the lower limbs) complications. In addition, patients with diabetic neuropathy or neurological/vascular complications that could alter pain perception were excluded. The study population was composed of 20 women and 50 men with a mean age of 47.8 ± 15.3 years and a mean duration of diabetes of 11.4 ± 10.3 years; 34.3% had T1D and 65.7% had T2D. The study was carried out according to the standards of Good Clinical Practice and the Declaration of Helsinki. All patients provided signed informed consent for participation.
Semi-rigid lancets were provided by Terumo Corporation (Tokyo, Japan) and consisted in a 23-gauge needle that was remodelled to permit less painful puncture than a traditional lancet (Fig. 5). Punctures (nominal penetration from 0.2 to 0.6 mm) were made at a depth variation of ± 0.13 mm. In addition, a novel puncture site was used, namely the area proximal to the nail bed of each finger (Figs. 6-8). In this area of the finger, blood flow is abundant and it is easy to obtain a blood sample. Moreover, the area has fewer tactile and pain receptors than the fingertip, and thus when lanced less pain is produced.
Six fingers were used in a random fashion to evaluate puncture of the anterior part of the finger, the periungual zone and the lateral area of the fingertip (depth 0.2-0.6 mm), and compared to fingertip puncture at a depth of 0.6 mm. The sensation provoked by puncture (with or without pain) was used to compare groups. Pain was evaluated using a VAS ranging from ‘no pain’ to ‘worst pain imaginable’. The VAS is a unidimensional tool that quantifies the subjective sensation such as pain felt by the patient and considers physical, psychological and spiritual variables without distinguishing the impact of the different components.
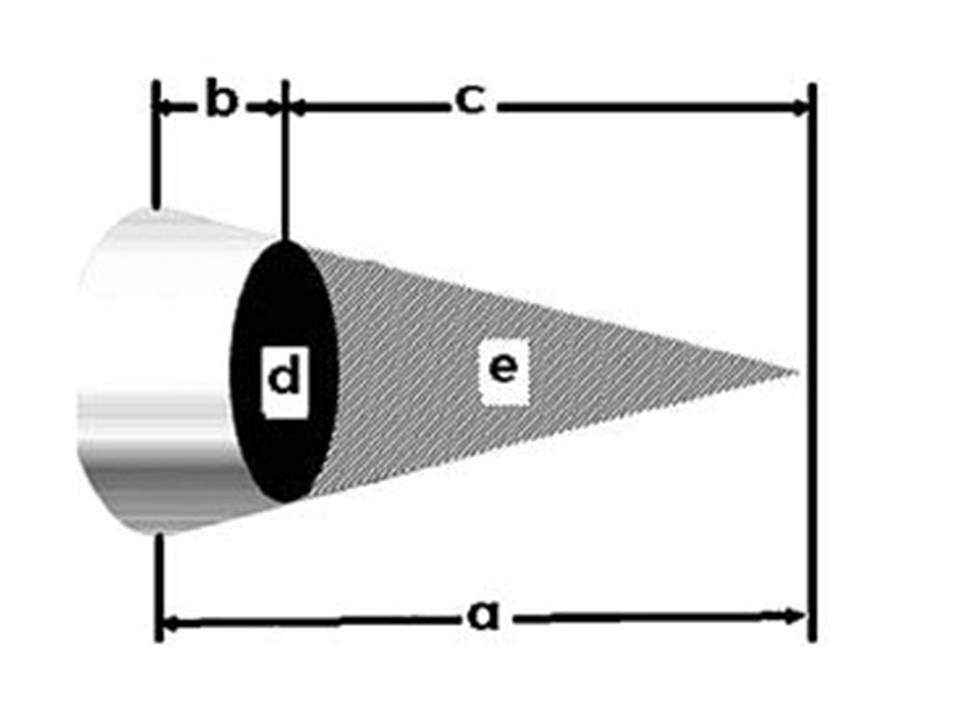
Figure 5. New lancet

Figure 6. Proximal lateral area of the nail bed as a new site of puncture.

Figure 7. Method of lancing.
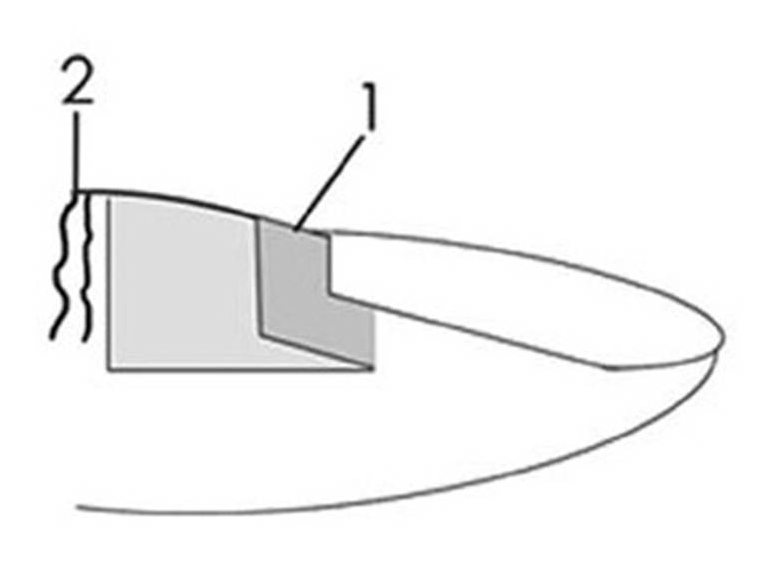
Figure 8. Site of lancing
Blood glucose was measured in the morning after 12 hours of fasting. The Fine Touch glucometer used was provided by Terumo Corporation (Tokyo, Japan). Statistical analysis was carried out using Fisher’s two-sided test. Differences in blood glucose with the two methods were analysed using Wilcoxon matched pairs signed ranks test. A P value <0.05 was considered statistically significant.
Results
Pain was not perceived in 90% and 94.28% of subjects punctured in the lateral area of the fingertip at a depth of 0.2 and 0.3 mm, respectively. At a depth of 0.4 mm, 67.14% of subjects did not perceive pain, while at 0.5 mm and 0.6 mm, 47.14% and 17.14% of subjects did not feel pain, respectively. There was no significant difference in pain considering punctures at 0.2 or 0.3 mm, while significant differences were seen between 0.2 and 0.4 mm (p <0.05), 0.5 mm (p <0.001) and 0.6 mm (p <0.001). All subjects who performed puncture in the central zone of the fingertip referred a painful sensation.
Using a periungual puncture site, pain was not referred by any subject, although a bothersome sensation was noted by some. The same results were obtained for all fingers used. Blood glucose levels obtained using traditional and alternative puncture sites were highly similar with no significant differences between groups (134.18 mg/dl ± 5.15 vs. 135.18 mg/dl ± 5.71 mg/dl; p = 0.5957).
Discussion
The present study evaluated the use of alternative puncture sites that are associated with less pain. These encouraging results undoubtedly warrant further investigation in a larger cohort, but nonetheless suggest that compliance with SMBG can be optimised. The use of the area close to the nail bed allowed high quality blood samples to be obtained for measurement of blood glucose, with an accuracy that was the same as that seen using the fingertip. The design of the lancet used herein was also associated with a lower perception of pain, which is composed of a hypodermic needle in a rigid casing that prevents accidental needle sticks both before and after use. Thanks to the needle point that was made using a triple-bevel cut, epidermal penetration is less traumatic and as a consequence less painful. This further favours rapid recovery of tactile function of patients with T2D. This allows the use of a larger transversal section using a puncture with less depth, and less involvement of nerves present in skin. In addition, the characteristics of the novel lancing device (Fine Touch, Terumo Corporation, Tokyo, Japan) allows adjusting the depth of puncture to the characteristics of each patient (e.g. in children, adolescents and adults).
The depth of penetration of the lancet can be varied from 0.3 to 1.8 mm with a self-incorporated selector; the maximum deviation of the lancing device in terms of depth is approximately 0.1 mm. Due to the possibility to select a minimal depth of only 0.3 mm, it can be used at alternative sites that allow a reduction in the frequency of samples taken from the fingertip. In theory, compared to traditional lancets, this would allow less perception of pain even at traditional sites as well as at periungual zones, and it was our intention to compare the different types of lancets to reinforce this idea. No puncture-related complications were reported, and another fundamental aspect that is not reported in other studies comparing traditional and alternative puncture sites is that no differences in blood glucose were observed.
In conclusion, it is our belief that a new type of finger lancet that decreases or eliminates pain associated with lancing merits additional consideration. Further studies are warranted on larger patient cohorts to confirm the present results. If validated, this would enable patients with diabetes - especially those who need to take several daily blood glucose samples - to perform SMBG with greater peace of mind and less distress.
|
Competing Interests None declared Author Details CRISAFULLI CRISTIANO, MASSIMO CATANUSO, CARMELO DI GREGORIO, ADRIANA DI GREGORIO, GAETANO PROFETA, ANTONINO DI GUARDO - Italian College of General Practitioners, Via del Pignoncino 9/11, Florence, Italy. CORRESPONDENCE: CRISTIANO CRISAFULLI, Via Livorno, 1 - 95127, Catania, Italy. Email: cricrisa@tin.it |
References
- Koschinsky T1, Jungheim K, Heinemann L. Glucose sensors and the alternate site testing-like phenomenon: relationship between rapid blood glucose changes and glucose sensor signals Diabetes Technol Ther. 2003;5(5):829-42
- Heinemann L. Finger Pricking and Pain: A Never Ending Story J Diabetes Sci Technol Vol 2, Issue 5, September 2008 p. 919-921

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




