Changing trends in acute upper GI bleeding a single-centre study in the western region of Saudi Arabia
Ibrahim Masoodi, Hesham AlQurashi & Mohammad Al Sofiyani
Cite this article as: BJMP 2019;12(3):a019
|
|
Abstract Background: Despite advancements in pharmacological and endoscopic management, upper GI bleeding continues to be a major medical emergency. Objective: This study aimed at identifying the etiological profile of upper GI bleeding in the western region of Saudi Arabia .The results were compared with previous Saudi Arabian data on upper GI bleeding. Methodology: In this retrospective study data on upper GI bleeding was analyzed at King Abdul Aziz specialist hospital Taif Saudi Arabia, a tertiary care centre in the western region of Saudi Arabia from January 2015 to December 2017. Results: A total of 120 (76 males) patients with acute upper GI bleeding were enrolled. The mean age of the study cohort was 58.4± 18.7. Hemetemesis was the most common presentation of upper GI bleeding. Variceal bleed (HCV Cirrhosis , Child-Turcotte-Pugh class A or B) was the most common aetiology (45.0%) of upper GI bleeding followed by duodenal ulcer (20.0%).Upper GI bleeding due to drug-induced and gastric ulcer were (5.0%) each. Endotherapy [EVL for portal hypertension bleeds, (gold probe endoscopic sclerotherapy ,heater probe for peptic ulcer bleeds)] was given to 72 (60%) patients. Bleeding recurrence of 1.2% was noted in this study. The mean hospital stay was 4.1±2 days and mean blood transfusion requirement was 2±1units. Conclusion: There is a decline in the prevalence of UGI bleeding due to duodenal ulcers in Saudi Arabia. Portal hypertension due to HCV related CLD was the most frequent cause of UGI bleeding in this study. Keywords: Gastrointestinal bleeding, chronic liver disease, peptic ulcer, duodenal ulcer, Rockall score. |
Introduction
Acute upper gastrointestinal bleeding presenting as either hematemesis or melena or both is an important medical emergency. The etiological spectrum of upper gastrointestinal bleeding (UGIB) varies from region to region1. Various endoscopic therapy for patients with signs of recent haemorrhage in peptic ulcer have changed the outlook of UGIB management. An addition of proton pump therapy to non-variceal UGIB has further reduced hospital stay, recurrent bleeding and need for surgery2. Another milestone in the decline of UGIB has been eradication of H pylori. Globally, the prevalence of H. Pylori infection has decreased due to better hygiene, early diagnosis and eradication3. These factors have contributed to the changing trends in UGIB. The patients with UGIB have 50% incidence of H. pylori infection positivity and re-bleeding occurs in 7-16 % of the total cases1. Once frequent UGIB due to peptic ulcer have now declined all over the globe as demonstrated by various researchers 4,5,6. Unfortunately, despite advancement in endoscopic and pharmacological treatment, the mortality in UGI bleeding ranges between 3 and 14%7. Particularly, patients with UGI bleeding due to the duodenal ulcer are known to be more prone to death as demonstrated by Quan et al8. The advanced age and patients admitted in hospital with comorbidity are at an increased risk of re-bleeding and mortality. Re-bleeding and mortality rates are higher among patients with variceal bleeds and invariably 50-60% of patients with cirrhosis have variceal bleeding1. This warrants a careful approach in the management of UGI bleed. To predict the re-bleeding rates in a given case of UGI bleeding various clinical and endoscopic models have been developed from time to time. Of these – Rockall score, combining clinical (Age, shock, presence of co-morbid diseases) and endoscopic findings have proved quite valuable in the prediction of hospital admission duration and mortality rate9. The reason for the feasibility of Rockall score is that it depends mainly on simple clinical data and after an endoscopic procedure the score becomes more practical 9. The Rockall score divides patients into 4 subgroups according to their clinical data to estimate death and re-bleeding tendency. While comparing Rockall score, Blatchford scores at first assessment, and the Addenbrooke score it was concluded that Rockall score has an accuracy of 98% in predicting death, and was sensitive in 86.4% of cases in predicting re-bleeding10. Hence we calculated Rockall score in our study cohort and assessed various prognostic factors including changing trends over the past decades.
Methods
Study design
This retrospective study was conducted from January 2015 to December 2017 at King Abdul Aziz Specialist hospital Taif, a tertiary care centre in the western region of Saudi Arabia. The data was collected from case files and electronic medical records. The data about age, comorbid diseases, presence of shock, endoscopic intervention, hospital stay duration, the requirement for blood transfusion, surgery were collected to measure the outcome of UGI bleeding.
Depending upon hemodynamic status upper GI bleeding patients were managed either in the intensive care unit (ICU) or high dependency unit of the hospital. Blood transfusion had been given to maintain Hb levels above 8gm/dl. Platelets transfusions if the platelet counts were < 70,000 and fresh frozen plasma when INR was deranged in chronic liver disease patients.
The recurrent bleeding was defined by hematemesis, melena, or both, with either shock
(pulse rate>100 beats/min, systolic blood pressure< 100mmHg accompanied by cold sweats, pallor, oliguria) or a decrease in haemoglobin concentration of 2 g/dL over 24 hours.
Re-endoscopy, if needed, was used only to confirm recurrent bleeding.
The timing of UGI endoscopy after admission was recorded in each patient. The details of stigmata of recent haemorrhage (spurting vessels, active bleeding in an ulcer, a visible vessel, or a clot over the ulcer that could not be dislodged upon gentle washing with water delivered through the endoscope channel). Rockall score was calculated in all patients.
Patients with variceal bleeding were primarily managed with octreotide infusion ,antibiotics and endoscopic variceal ligation (EVL) or endoscopic sclerotherapy (EST) depending upon the situation. All patients were followed for rebleeding clinically and by haemoglobin levels during their hospital stay. Patients who remained hemodynamically stable for 72 hours were discharged.
After the fifth day, patients positive for H. pylori on CLO test during endoscopy received triple therapy (Capsule Amoxicillin 1gm twice daily and Tab. Clarithromycin 500 mg twice daily for 2 weeks. Tab. Es omeprazole 20mgdaily twice daily was continued for 4weeks. The patients who were H. pylori-negative received Tab. Esomeprazole 20 mg twice daily for 4 weeks.
Inclusion criteria:
- Patients with confirmed upper GI bleeding (variceal and non-variceal) were enrolled in this study.
- The variceal bleeding due to portal hypertension included both cirrhotic & non-cirrhotic patients.
Exclusion criteria:
- Patients with terminal cancer.
- Patients with upper GI bleeding where endoscopy had not been done due to any reason and Rockall score could not be calculated.
- Patients with persistent shock necessitating emergency surgery, as a life-saving procedure.
Statistical methodology:
Data were statistically described in terms of frequencies (number of cases) and valid percentages for categorical variables. Mean and the standard deviation was used to describe parametric numerical variables while the median and inter-quartile range were used for non-parametric variables. Spearman's rho test was used for testing the correlation between the non-parametric numerical variable (Rockall score) and patients’ age. All statistical calculations were done using computer program IBM SPSS (Statistical Package for the Social Science; IBM Corp, Armonk, NY, USA) release 21 for Microsoft Windows.
Results
A total of 120 participants (76 males,63.3%) with a mean± SD age of 58. 4± 18. 7 years, were included in this study. The Rockall score showed a median (IQR) value of 3 which indicates a low to moderate risk of bleeding recurrence and death.
Majority of the study cohort [n=88(74%)] were Saudi nationals and [32(6.7%)] patients were from other nations. All patients had received an initial resuscitation as per the UGIB protocol of the hospital. Of 120 patients, 30 patients (25%) had undergone endoscopy immediately after admission in the intensive care of the hospital due to hemodynamic instability. Fourteen patients (11.7%) had undergone endoscopy within 6 hours of hospital admission and 63% patients had undergone endoscopy within 24 hours of hospital admission. The details are shown in figure 1.
The Rockall score was calculated for all patients based on their age, presence of shock, comorbidities, diagnosis and major stigmata of recent haemorrhage. The details are shown in table 1.
Table 1: Parameters of Rockall score in the non-variceal bleeds
| Percentage | Frequency | Category | Parameter |
| 52 | 43.3 | <60=0 |
Age |
| 16 | 13.3 | >80=2 | |
| 52 | 43.3 | 60- 79= 1 | |
| 120 | 100.0 | Total | |
| 80 | 66.7 | No shock=0 |
Shock |
| 40 | 33.3 | Tachycardia: Pulse ≥100, Systolic BP ≥100= 1 | |
| 120 | 100.0 | Total | |
| 70 | 58.3 | Any co-morbidities except renal failure, liver failure, and/ or disseminated malignancy=2 |
Co-morbidities |
| 50 | 41.7 | No major comorbidity= 0 | |
| 120 | 100.0 | Total | |
| 116 | 96.7 | All other diagnoses= 1 |
Diagnosis |
| 4 | 3.3 | upper GIT malignancy= 2 | |
| 120 | 100.0 | Total | |
| 26 | 21.7 | Adherent clot=3 ,ooze=2 vessel=2 spurting vessel=0 |
Major stigmata of recent hemorrhage |
| 100.0 | Total |
It was observed that 46(38.3%) patients had undergone endoscopic variceal ligation (EVL) , and 20(16.7%) patients endoscopic sclerotherapy (EST) .
Heater probe had been used in 5.0% and Gold probe in 5.0% of patients with signs of recent haemorrhage (SRH) . Nevertheless, 48(40.0%) patients had no features of SRH therefore they had not received any endotherapy. Instead they had been managed with IV proton pump inhibitors as per the protocol and supportive treatment.
The data on final EGD diagnosis are shown in table 2.
Table 2: The Most Frequent EGD Diagnoses
| Diagnosis | Frequency | Percent |
| CLD with PHT | 54 | 45.0 |
| Duodenal ulcer | 24 | 20 |
| Drug induced GI bleed | 20 | 16.67 |
| Gastric ulcer | 10 | 8.3 |
| Hemorrhagic gastritis | 8 | 6.67 |
| GI Malignancy | 4 | 3.3 |
| Total | 120 |
(CLD: Chronic liver diseases, GI: Gastro intestinal, EGD: oesophagogastroduodenoscopy, PHT: Portal hypertension)
None of the study cohort patients had undergone surgery to control his or her UGI bleeding and there was no mortality due to UGIB recorded during this period.
In order to test the correlation between Rockall score and age, spearman rho correlation test was carried out and data showed a significant (p<0. 001) moderate positive relationship (correlation coefficient=0. 553) between age and Rockall score of included patients. This means a lower tendency for recurrent bleeding and a lower mortality rate among younger patients.
Discussion
The results of our study showed that hematemesis was the most frequent presenting symptom of UGI bleeding. These results are similar to the study by Minakari et al 11, however, majority of the patients in the above-mentioned study had a peptic ulcer as the commonest aetiology. Contrary to their results portal hypertension outnumbered the peptic ulcer disease as shown in Table 2 in this study. UGI endoscopy had been carried out immediately after admission in 25% of the patients due to ongoing bleeding and the majority of patients had UGI endoscopic examination within 24hrs as shown in Fig1.
Figure 1: Timing of Esophagogastroduodenoscopy (EGD) after hospital admission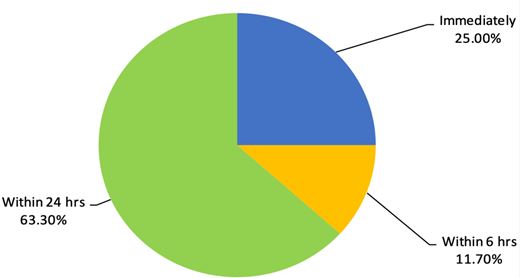
While assessing the endoscopy timing especially among variceal bleeding Hsu YC et al 12 concluded that the delayed endoscopy for more than 15 hours , high MELD score, failure of the first endoscopy and hematemesis were independent risk factors for in-hospital mortality in cirrhotic patients with acute variceal haemorrhage. The cirrhotic patients in our study cohort were either Child-Turcotte-Pugh class A or B and none of the patients had hepatic encephalopathy on presentation. After endoscopic therapy, they were managed with standard treatment for variceal bleeding.
The prevalence of H. pylori positivity among UGI bleeding in this study was 60% and all positive patients had been given standard eradication therapy. Data from a different Saudi Arabian centre revealed H. pylori prevalence to the tune of 70% affecting predominantly females in patients with peptic ulcer disease13 but authors had not studied it’s prevalence in UGI bleeding.
This study demonstrated rebleeding in 16 (13. 33%) patients who were re-endoscoped and bleeding was controlled by various endotherapies. In this study re-bleeding was found to be more frequent among older patients with comorbidities. Rebleeding was also common among patients with history of NSAID intake and presence of oesophagal varices which is following literature14. While comparing present results with previous data we observed that previously the commonest cause of UGI bleeding was a duodenal ulcer it is the variceal bleeding due to cirrhosis (HCV) now. We also compared the results of the current study with previous studies across different parts of the globe14,15,16. Duodenal ulcer previously used to be the most frequent cause and invariably various surgical methods like vagotomy etc were used to control bleeding prior to PPI era. However, with the advent of PPI and H pylori eradication the frequency of UGI bleeding due to peptic ulcer have declined.
We recorded only 120 patients with UGI bleeding over three years at our centre nevertheless, this may not reflect the true incidence in the region as it was the data from a single centre only. But the overall incidence of UGI bleeding has decreased over the past decades all over the globe. The study by Loperfido et al17 compared the incidence of 587 patients with UGIB between 1983-1985 and 2002-2004 period. The authors observed that UGI bleeding decreased from 112.5 to 89.8 per 100,000/y. The peptic ulcer incidence also decreased to the half between the two studied periods. In the above-mentioned study it was also revealed that frequency of ulcer bleeding decreased by 41.6% in people younger than 70 years. There has been an obvious change in the trend of UGI bleeding in Saudi Arabia over the past 23 years like other regions of the globe. The number of patients with UGI bleeding has decreased and aetiology of UGI bleeding has also shifted from an ulcer to variceal one.
In a large study, published in 1995 ,the data on 1246 patients over 14 years Al Karawi et al18 observed that duodenal ulcer was the most common cause of UGI bleeding followed by varices. The bleeding rates per annum in their study was 89 cases per annum while this study recorded only 40 admissions of active UGI bleeding per annum. Further, the variceal bleeding outnumbered the duodenal ulcer bleeding contrary to their results connoting a changing trend in Saudi Arabia. The data from southern region of Saudi Arabia also showed variceal bleeding to be the commonest cause of UGI bleeding 19.
In yet another study from Riyadh central hospital, it was revealed that most of the patients with UGI bleeding were having oesophagal varices20. Non cirrhotic portal hypertension (NCPH) was documented in 8 patients in the current study and all were hailing from Egypt which is an endemic region for schistosomiasis and NCPH. The predominant cause of portal hypertension was Chronic liver disease due to chronic HCV in this study. While studying the pattern of liver disease in Saudi Arabia Fashir B et al20 have demonstrated HCV to be the commonest cause of CLD in this part of the globe. This reflects that meticulous screening and treatment of chronic HCV can go a long way in the reduction of UGIB in the region. Having said this it may not be out of place to mention that keeping in view the global epidemic of obesity variceal bleeding due to CLD following NASH may steep up in coming years and become the important cause of UGIB. This highlights a red alert to curb the menace of obesity all over the globe and halt the increasing trend of variceal bleeding in future.
Regarding the trend of gastric ulceration, UGI bleeding has now shifted from H. Pylori infection to the massive use of medications such as NSAIDs or steroids, all over the world16 especially among older people. We demonstrated drug-induced UGI bleeding in 20(16%) patients in this study as shown in table 2. Further the use of warfarin is estimated to increase as the population ages and atrial fibrillation , other cardiovascular ailments are increasing steadily. In a study by McGowan et al22 Tablet Warfarin was an independent predictor of major bleeding after the percutaneous coronary intervention (PCI) in patients receiving dual antiplatelet therapy.
Another most common diseases in the elderly population is Rheumatoid arthritis (RA) . Rheumatoid arthritis is considered as a comorbid disease in the Rockall score and increases the scale for mortality and hemorrhagic shock. The wide use of NSAIDs in RA patients steeps the incidence of peptic ulcers and its complications including UGIB23. This risk is significantly elevated when SSRI medications in combination with NSAIDs are prescribed to allay anxiety and depression in these chronic disorders. The physicians prescribing these medications together should exercise caution and discuss this risk of UGIB with patients24.
UGI bleeding due to malignancies were noted in 4 patients in our study cohort which is similar to the data shown in the southern region of Saudi Arabia19.
In this study, about 12-16% of the patients were diagnosed with either gastric ulcer or hemorrhagic gastritis. The data from Arar, the northern Saudi Arabian city , revealed prevalence of gastric ulcer to be twice as common as duodenal ulcer. The authors of this study observed that the use of NSAIDs, H. Pylori infection and stress were among the most relevant reasons for developing peptic ulcer disease , however authors in their study didn’t study bleeding complications of peptic ulcer disease25.
Conclusion
Based on discussed results, it can be concluded that the frequency of UGI bleeding has declined and peptic ulcer is no longer the most predominant cause of UGI bleeding in Saudi Arabia. Instead, variceal bleeding outnumbers other causes of UGIB. This changing trend now demands that to prevent variceal bleeding we need to focus on the management of chronic HBV, HCV and NASH. Further all medications especially NSAIDs must be cautiously used particularly in elderly people. A step further would be to control hypertension and subsequent atrial fibrillation so that drug-induced UGI bleeding are reduced in future.
|
Competing Interests None declared Author Details IBRAHIM MASOODI, College of Medicine, Taif University, KSA. HESHAM ALQURASHI, King Abdul Aziz specialist Hospital, Taif, KSA. MOHAMMAD AL SOFIYANI, King Abdul Aziz specialist Hospital, Taif, KSA. CORRESPONDENCE: Ibrahim Masoodi, Associate Professor, College of Medicine, Taif University, KSA. Email: ibrahimmasoodi@yahoo.co.in |
References
- Leerdam V. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22(2) :209-24
- Javid G, Masoodi I, Zargar SA, Khan BA, et alOmeprazole as adjuvant therapy to endoscopic combination injection sclerotherapy for treating bleeding peptic ulcer. Am J Med. 2001 Sep;111(4) :280-4.
- Frugis S, Czeczko NG, Malafaia O, Parada et al Prevalence of Helicobacter pylori ten years ago compared to the current prevalence in patients undergoing upper endoscopy Arq Bras Cir Dig. 2016 Jul-Sep;29(3) :151-154.
- Jiang M, Chen P, Gao Q: Systematic Review and Net-Work Meta-Analysis of Upper Gastrointestinal Hemorrhage Interventions. Cell Physiol Biochem 2016;39:2477-2491.
- Roberts-Thomson IC. Rise and fall of peptic ulceration: a disease of civilization?. JGH. 2018;33(7) : 1321-1326
- Malmi H. Peptic ulcer disease incidence, associated morbidity and mortality. Helsinki university hospital. 2018
- Van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22(2) :209-24.
- Quan, S. , Frolkis, A. , Milne, K, et al. Upper-gastrointestinal bleeding secondary to peptic ulcer disease: Incidence and outcomes. WJG, 2014; 20(46) , 17568–17577.
- Wang CY, Qin jJ, Wang J, Sun CY, Cao T, Zhu DD. Rockall score in predicting outcomes of elderly patients with acute upper gastrointestinal bleeding. world journal gastroenterol. 2013; 19(22) : 3466–3472.
- Dworzynski K, Pollit V, Kelsey A, Higgins B, Palmer K; Guideline Development Group. Management of acute upper gastrointestinal bleeding: summary of NICE guidance. BMJ. 2012 Jun 13;344:e3412.
- Minakari M, Badihian S, Jalalpour P, Sebghatollahi V. Etiology and outcome in patients with upper gastrointestinal bleeding: Study on 4747 patients in the central region of Iran. J Gastroenterol Hepatol. 2017 Apr;32(4) :789-796
- Hsu YC, Chung CS, Tseng CH, Lin TL, Liou JM, Wu MS, Hu FC, Wang HP. Delayed endoscopy as a risk factor for in-hospital mortality in cirrhotic patients withacute variceal hemorrhage. J Gastroenterol Hepatol. 2009 Jul;24(7) :1294-9.
- Karima TM, Bukhari SZ, Ghais MA, Fatani MI, Hussain WM. Prevalence of helicobacter pylori infection in patients with peptic ulcer diseases. Saudi med j. 2006; 27(5) :621-6.
- Gutermann IK, Niggemeier V, Zimmerli LU, Holzer BM, Battegay E, Scharl M. Gastrointestinal bleeding and anticoagulant or antiplatelet drugs: systematic search for clinical practice guidelines. Wang. H HWA, ed. Medicine. 2015;94(1)
- Tielleman T, Bujanda D, Cryer B. . Epidemiology and risk factors for upper gastrointestinal bleeding. Gastrointest Endosc Clin N Am 2015; 25:415–28.
- Kuipers EJ. PPI for prevention and treatment of peptic ulcer. The lancet. Feb. 2018; 3(4) :214-215.
- Loperfido S1, Baldo V, Piovesana E, Bellina L, Rossi K, Groppo M,et al. Changing trends in acute upper-GI bleeding: a population-based study. Gastrointest Endosc. 2009 Aug;70(2) :212-24.
- Al Karawi MA, Ghandour Z, Mohamed Ael S. Causes of upper gastrointestinal bleeding: Experience at a major hospital in Riyadh. Ann Saudi Med. 1995 Nov;15(6) :606-8.
- Ahmed ME, al-Knaway B, al-Wabel AH, Malik GM, Foli AK. Acute upper gastrointestinal bleeding in southern Saudi Arabia. J R Coll Physicians Lond. 1997 Jan-Feb;31(1) :62-4.
- Al-mofarreh M, Facharzt Y, Fakunle M,Al-moagel A, Facharzt. Upper gastrointestinal bleeding among Saudis: etiology and prevalence the Riyadh central hospital experience. ASM. 1991;11(5) .
- Fashir B, Sivasubramaniam V, Al Momen S, Assaf H. Pattern of liver disease in a Saudi patient population: A decade of experience at security forces hospital, Riyadh, KSA. SJG. 1996;2(1) :50-52.
- McGowan C, Lee G, DeCaro M, Ruggiero N,et al. Risk of majorbleeding with concomitant dual antiplatelet therapy after percutaneous coronaryintervention in patients receiving long-term warfarin therapy. Pharmacotherapy. 2007 May;27(5) :691-6.
- Koff RS. Prevention on NSAIDS induced gastric ulcer. Gastroenterology. 1989; 97(4) :1054
- Anglin R, Yuan Y, Moayyedi P, Tse F, Armstrong D, Leontiadis GI. Risk of uppergastrointestinal bleeding with selective serotonin reuptake inhibitors with orwithout concurrent nonsteroidal anti-inflammatory use: a systematic review andmeta-analysis. Am J Gastroenterol. 2014 Jun;109(6) :811-9.
- Albaqawi A, Abo El-Fetoh N, Alanazi R, Alanazi N, Alrayya S, Alanazi A, et al. Profile of peptic ulcer disease and its risk factors in Arar, northern Saudi Arabia. Electron physician. 2017.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




