Gopall Jayprakash, Cheng Yong and Wang Yanqing
Abstract
Introduction: Schwannoma is a peripheral nerve sheath tumour and commonly occurs on the head, neck and trunk. Giant schwannoma is rarely located in the retroperitoneum, the pelvis and rarer in the mesorectum.
Case presentation: A 36 year old Asian male patient presented with a lower abdominal mass since 2 months, urgency of defecation since 6 months, erectile dysfunction for more than 3 years.
Conclusion: We report this patient with a mesorectal schwannoma because of its giant size, rare location, vague symptoms and diagnostic dilemma.
Abbreviations: HIFU - high intensity focused ultrasound, CT – Computer Tomography, MRI – Magnetic Resonance Imaging, FNAC – Fine Needle Aspirate Cytology
|
Introduction
Schwannoma (neurilemmoma) is a peripheral nerve sheath tumour and commonly occurs on the head, neck and trunk. Giant schwannoma is rarely located in the retroperitoneum and the pelvis but rarer in the mesorectum. The majority of symptoms caused by the tumour are due to its mass effect. Surgical resection is enough to treat the tumour. Schwannoma is usually a benign tumour. Its malignant transformation is usually very rare. We report a 36 year old male patient with a giant mesorectal schwannoma who presented with vague symptoms.
Case Report
A 36 year old male patient presented with a lower abdominal mass since 2 months, urgency of defecation since 6 months and erectile dysfunction for more than 3 years. There was no history of urinary disturbances. General physical examination did not reveal any abnormality. Abdominal examination showed a non tender, firm, fixed mass with well defined borders over the suprapubic region which was extending into the pelvis. No organomegaly was detected. On rectal examination a hard, immobile mass was felt 5 cm away from the anal verge and lying anterior to the rectum.
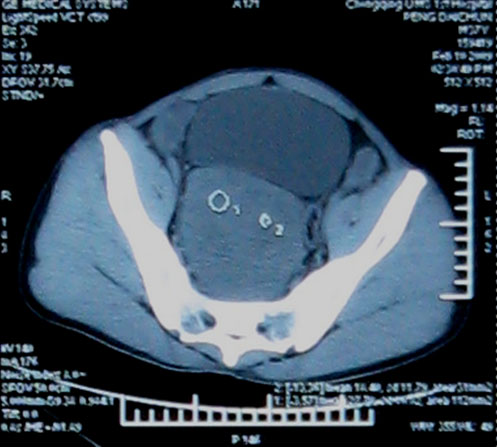
His urine analysis, routine hematological investigations and renal function test were within normal limits. Total bilirubin was raised to 24.9 µmol/l (3.42-20.52 µmol/l), direct bilirubin was also elevated 8.2 µmol/l (0-6.8 µmol/l) while all other results were within normal range. The patient was positively screened for Hepatitis B and Syphilis. CT scan (figure 1) of abdomen revealed a large soft tissue mass measuring 10x11 cm in the pelvis. It was a well defined mass without any infiltration to the following structures: sigmoid, rectum, prostate gland, the bladder and the sacral bone.
Figure 1 shows a large soft tissue mass measuring 10x11 cm which compresses the rectum.
FNAC of the mass which was taken 3 cm from the anal verge showed isolated fibrotic tumor.
The patient was advised for HIFU therapy (high intensity focused ultrasound) in view of eventual surgery. In HIFU therapy, the ultrasound beams are focused on the diseased tissue and due to the significant energy deposition at the focus, temperature within the tissue rises to 65° to 85°C, destroying the diseased tissue by coagulation necrosis and hence facilitating the dissection of the mass during surgery. After HIFU therapy, the patient no longer complained of urgency of defecation. But there was no significant change in the size of the mass after a rectal examination.
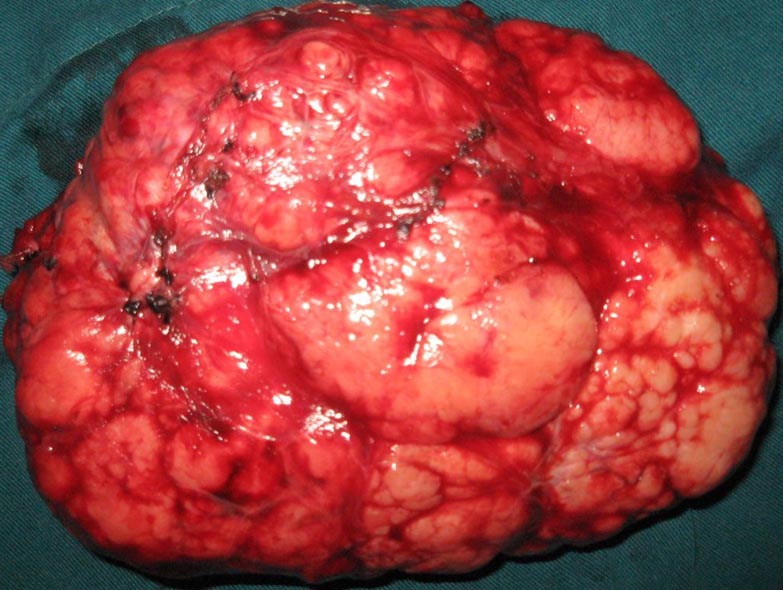
Hence, explorative laparotomy was carried out. The abdomen was opened through the lower midline incision. A huge mesorectal mass of 15x11x8 cm (figure 2), was identified on the right side of the rectum and behind the prostate gland extending upwards, without any posterior infiltration into the sacral bone. Complete excision of the mass was achieved by blunt dissection and the mass was sent for histopathological examination. The operation was uneventful.
Figure 2 shows the complete excision of a well encapsulated mass of 15x11x8 cm. The external surface of the mass was gray-white and smooth.
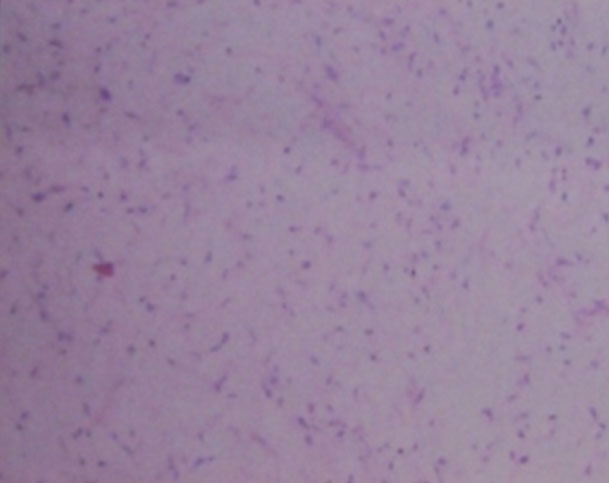
Figure 3: Histology showing typical pallisading arrangement of spindle cells (Antoni-A/Verocay Body) and less cellular myxoid areas (Antoni-B)
Discussion
Schwannoma (Neurilemmoma) is a benign neoplasm arising from the myelinated nerve sheaths. Malignant schwannoma despite their name, never arise from malignant degeneration of schwannomas. Instead they occur from transformation of a plexiform neurofibromatosis. This fact provides the basis for their association with neurofibromatosis1.
Schwannomas are frequently present in patients aged 20 to 50 years with a male predominance. They comprise 5% of all benign soft tissue tumors and have a predilection for the head and neck2, 3, 4 and flexor surfaces of the upper and lower extremities5. Pelvic schwannoma is rare and accounts for less than 1% of all benign schwannomas6. The rarity of this tumor and the lack of clinical manifestations make a pre-surgical diagnosis very difficult.
These tumors slowly increase in size before becoming symptomatic. Clinical signs or symptoms manifest themselves only by the compression or infiltration of adjacent organs. Therefore, detection is often accidental.
Schwannoma typically appears as a solitary, well encapsulated, firm and smooth-surfaced round mass. In large tumors (>8-10 cm), a degenerative pattern (cystic areas, calcifications, interstitial fibrosis, and hyalinization) is commonly found that identifies the “ancient” variant7. Histologically, typical schwannomas are composed of inter mixed Antoni A components (cellular and arranged in short bundles or interlacing fascicles) and Antoni B areas (less cellular and organized with more myxoid components).Schwannomas show uniform and intense staining for S 100 protein8.
Malignant transformation is very rare and controversial9. Malignant schwannomas are large in size and highly aggressive tumours. They are painful, and may cause many different symptoms depending on the location and size. They infiltrate into the adjacent structures and metastasize to distant sites. Histologically, the nuclear palisading may be a striking feature. There will be perineural and intraneural spread of tumour, lesional proliferation, or herniation into the lumina of the vessels10.
A combination of clinical, pathological and immuno-histochemial studies help to make the diagnosis.
However preoperative diagnosis of schwannomas is not easy owing to the difficulty in finding imaging features (with Ultrasonography, CT, or MRI) that enable the discrimination of schwannomas from other soft tissue tumors (fibrosarcoma or liposarcoma) and benign forms from malignant ones11. Schwannomas can frequently be misdiagnosed as psoas abscesses, pancreatic cysts, neoplasms, adnexal masses, adrenal, kidney or hepatic tumors, as reported in the literature12, 13, 14. Yet, radiological imaging is helpful in therapeutic planning, as it gives information about the tumor’s size, location, and possible invasion of other structures. Fine-needle aspiration biopsy may theoretically be useful if Schwann cells are found in the sample, but the tissue specimen collected for diagnosis is often inadequate and may be misleading because of cellular pleomorphism in degenerated areas which might be interpreted as consistent with malignancy15.
Hughes MJ et al11, in their largest radiological series of abdominal or pelvic schwannomas, showed that a smooth well defined border, ovoid or spherical shape and location in the pre sacral region or lower retro peritoneum at the pelvic brim, are frequent findings in primary abdominal or pelvic schwannomas ; 11 of 13 cases showed all these features. Evidence of degeneration was common, with 8 schwannomas showing cystic change and 3 showing areas of calcification. The cystic schwannomas tended to be larger, with a mean diameter of 10.5cm.
It is difficult to make an accurate pre operative diagnosis. The treatment depends solely on surgery. Malignant schwannomas are insensitive to chemotherapy and radiation, resulting in poor prognosis16.
Conclusion
Schwannoma is a benign encapsulating neoplasm with an overall low incidence, occurring mostly in the head, neck and trunk regions. Giant schwannoma is rarely located in the retroperitoneum, the pelvis and rarer in the mesorectum.
Schwannomas pose a difficult diagnostic challenge. Radiological findings are often non-specific. Ultrasonography can differentiate between solid and cystic tumours. CT can be helpful in determining the size, location, local involvement and distant spread. MRI provides similarly useful information as CT, but yields better visualization of the tumour. FNAC is not often helpful because the tissue architectural information required is not obtainable from cytological specimen. The only gold standard diagnostic investigation is histology of either biopsy or excised specimen.
Surgical excision has remained the mainstay of treatment. Although benign, large and incompletely excised lesions are capable of recurrence, malignant change is exceedingly rare.
Competing Interests
None declared
Author Details
<p>GOPALL JAYPRAKASH-General Surgery department, The First Affiliated Hospital, Chongqing Medical University, Chongqing 400016, China.<br />
CHENG YONG-Associate Professor, Department of General Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.<br />
WANG YANQING-Professor, Department of General Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.</p>
CORRESPONDENCE: CHENG YONG, Associate Prof, Department of General Surgery, The First Affiliated hospital, Chongqing University of medical science, Chongqing 400016, China.
Email: vishall_76@yahoo.com |
References
1.Rai BR1, Chaudhary D1, Thapa P. Ancient cystic pelvic schwannoma presenting as a right iliac fossa mass. Kathmandu University Medical Journal (2005) Vol. 3, No. 3, Issue 11, 285-288.2.Jayaraj SM, Levine T, Frosh AC. Ancient schwannoma masquerading as parotid pleomorphic adenoma. J Laryngol Otol 1997; 111:1088–1090. 3.Ogren FP, Wisecarver JL, Lydiatt DD. Ancient neurilemmoma of the infratemporal fossa: a case report. Head Neck 1991; 13:243–246. 4.Dayan D, Buchner A, Hirschberg A. Ancient neurilemmoma (schwannoma) of the oral cavity. J Craniomaxillofac Surg 1989; 17: 280–282. 5. Graviet S, Sinclair G, Kajani N. Ancient Schwannoma of the foot. J Foot Ankle Surg 1995; 34:46–50. 6.Ng KJ, Sherif A, McClinton S. Giant ancient schwannoma of the urinary bladder presenting as a pelvic mass. Br J Urol 1993; 72:513–514. 7.Peter T Chan, Sankalp Tripathi , Su E Low. Ancient schwannoma of the scrotum. BMC Urology 2007, 7:1doi:10.1186/1471-2490-7-1 8.S.W. Weiss and J.R. Goldblum. Benign tumours of peripheral nerves. In: S.W. Weiss and J.R. Goldblum. Editors, Enzinger & Weiss’s soft tissue tumours. Mosby, Messouri, USA (2001): 1146-68. 9.Rasbridge SA, Browse NL, Tighe JR. Malignant nerve sheath tumor arising in benign ancient schwannoma. Histopathology 1989; 14:525–528. 10. J. Nakashima, M. Ueno, K. Nakamura. Differential diagnosis of primary benign and malignant retroperitoneal tumours. Int J Urol 1997; 4: 441-46. 11. Hughes MJ, Thomas JM, Fisher C. Imaging features of retroperitoneal and pelvic schwannomas. Clin Radiol. 2005:60:886-893. 12. Kishi Y, Kajiwara S, Seta S. Retroperitoneal schwannoma misdiagnosed as a psoas abscess: report of a case. Surg Today.2002; 32:849-852. 13. Ibraheim M, Ikomi A, Khan F. A pelvic retroperitoneal schwannoma mimicking an ovarian dermoid cyst in pregnancy. J Obstet Gynaecol. 2005; 25:620-621. 14. Duran B, Guvenal T, Yildiz E. An unusual cause of adnexal mass: fallopian tube schwannoma. Gynecol Oncol. 2004; 92:343-346. 15. Daneshmand S, Youssefzadeh D, Chamie K, et al. Benign retroperitoneal schwannoma: a case series and review of the literature. Urology. 2003; 62:993-997. 16. Qiang Li, Chuntao Gao, Jonathan T. Analysis of 82 cases of retroperitoneal schwannoma. ANZ Journal of surgery 2007; 77 (4); 237-40.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.