Can Online Distance Learning improve access to learning in conflict zones? The Oxford Psychiatry in Iraq (OxPIQ) Experience
Yasir Hameed, Hasanen Al Taiar, Denis O'Leary & Lucy Kaynge
Cite this article as: BJMP 2018;11(2):a1114
|
|
Abstract Psychiatry trainees in Iraq face many challenges that limit their immediate access to training opportunities. These include limited opportunities to attend international conferences due to visa restrictions, reduced access to evidence-based practice and guidelines and less experience in conducting quality improvement projects and audits. There are also issues related to their training programmes, including lack of regular meetings with supervisors and fewer opportunities for case-based discussions. Clinical Psychiatry is thus a potential key affected clinical domain due to the above factors. Technological advances in the field of e-learning created concepts such as Technology-enhanced or Web-based learning (TEL or WBL). These developments enabled the formation of “virtual teams” using an online platform. These teams overcome logistical geographical and other barriers to enable professionals to connect and learn from each other. This paper includes an appraisal of the TEL, looking at its advantages and challenges in meeting the needs of learners and educators. Also, we describe how we incorporated evidence-based and good practice guidelines on TEL use in these circumstances to the design, delivery and early evaluation of the distance learning programme. In our conclusion, we add to these and draw attention to the use of established online platforms (Medicine Africa in this case) and the importance of involving Iraqi Training leads, trainees and institutions in identifying trainee learning needs and supporting existing training provisions. Keywords: Online learning, virtual learning teams, case-based discussion, learning theories.Abbreviations: Technology-enhanced or Web-based learning |
Background and rationale
Psychiatric trainees in Iraq face many challenges that limit their immediate access to improved training opportunities. These include limited access to classroom teaching, regular clinical supervision meetings and fewer opportunities to attend international conferences and placements. These challenges are more acute in those specialities with the greatest shortage of consultants (for example, forensic and child and adolescent psychiatry).
Furthermore, the fragile security situation in the capital and larger cities and the post-conflict disruption to educational institutions consequent to these difficulties makes it difficult for those in the UK and elsewhere to visit the country and support educators and training on the ground.
Against this background and as a medical educational team in the UK (Oxford University Medical Education Fellows, OUMEF) with an interest in developing training opportunities for peers and colleagues in Iraq, we set up the Oxford Psychiatry in Iraq (OxPIQ) Project, beginning with a project development team that included Medicine Africa, an experienced online distance learning platform.
So what is the role of TEL in the delivery of online distance learning targeted at medical professionals in these circumstances?
Meeting the Challenge – the role of TEL
The concept of Technology-enhanced Learning (TEL), or Web-based learning (WBL), defined as the use of information and communication technologies in teaching and learning 1, is a relatively new phenomenon. Nevertheless, there is a considerable body of evidence supporting the use of TEL in various clinical and non-clinical settings.
Mccutcheon et al. 2 systematically reviewed thirteen studies and found that ten of these studies concluded that online learning is as effective as traditional or classroom teaching, despite the limitations of some of these studies.
In a large meta-analysis, Means and colleagues 3 concluded that students using online teaching performed modestly better compared to students learning similar material using face-to-face teaching. Combining face-to-face and online teaching resulted in larger benefit compared to the use of face to face methods only.
TEL can address the learning limitations in classroom settings due to expanding curriculum coverage and limits on contact time between students and lecturers/trainers alike. It can contribute to better use of such face-to-face classroom contact through the facilitation of the flipped classroom approach. 4 In this approach (also called inverted instruction and upside-down teaching), students acquire the basic information of the lesson outside the class (usually using online materials) and then develop their knowledge further in the class by sharing their learning, interacting with other classmates and teacher, and discussing various aspects of the study topic.These advantages have enabled TEL to revolutionise distance learning at many levels – enabling greater access to education by overcoming geographical and time-zone boundaries.
An allied concept within distance TEL is the concept of virtual teams 5 where health professionals come together to teach and learn from each other independent of location. Of itself, this offers some advantages. These include the possibility of addressing speciality-specific training gaps through the incorporation of the relevant expertise within the team - and to the creation of what is termed “connectivism”. This term refers to the use of internet technologies to enhance learning through online peer networks 6 and the development of communities of practice. 7 The latter allows for workplace-based learning with trainees learning from more experienced practitioners and moving towards the same through greater competency acquisition.
In a similar vein, creating networks of professionals may help to establish more longer-lasting relationships of mutual benefit between the UK and Iraqi professionals (e.g. through collaboration on training programmes, conferences, etc.). Also, cross-cultural online learning has been shown to be very useful in improving language skills and cultural awareness of learners and educators. 8 With language translation technology, any language difficulties can also be overcome, especially if the educator can observe the learners’ responses to the translated text and offered the opportunity to give further explanations and clarifications when necessary. 9 Finally, as well as sharing knowledge and experience within groups, TEL enables opportunities for mentoring and coaching individuals. 10
For our purposes, these findings and opinions support the use of online learning as a suitable distance learning “add-on” to existing training opportunities in Iraq.
TEL and Learning Theories
Learning theorists suggest that experiential and constructive learning theories are most appropriate to learning in the clinical context. Both are possible with TEL (as well as being facilitative of behaviourist and cognitivist approaches).
For example, the virtual classroom environment can enhance the learning experience of the participants by improving their analytical skills by thinking through case formulation and management plans. 11 Participants in online learning could be assessed and receive the feedback immediately. Ideas can be shared, and there is no passive acquisition or transfer of knowledge as is the case with traditional lectures. These aspects have implications for the design of the educational sessions and are discussed below in the learning methods section.
Challenges of Online Distance Learning
There are many challenges associated with online distance learning. Firstly, there is the potential lack of the required technologies (internet access, laptops or desktop computers), the expenses of subscribing to these online learning templates, the need to have technical support, and similar technical and logistic issues. 12 These technical problems may impair access to and functioning of the virtual team. The choice of an experienced online platform must, therefore, be considered carefully.
Secondly, there may be ethical issues about the protection of patients’ confidentiality in these sessions, especially when there are different laws of privacy that are applied in the UK and Iraq. This will require knowledge of the relevant professional requirements by the tutor team for example.
Furthermore, the student-teacher relationship has traditionally been underpinned by direct face-to-face contact and being present at the same time and place. 11 Therefore, learners and educators might be less satisfied with online learning. For these reasons, the concept of blended learning (careful integration of online learning with face to face learning experience) has been developed to overcome the limitations of a standalone online or face to face learning and has been found effective and applicable in various settings. 13
Thirdly, any distance online learning programme must understand and support existing “local” training provision and arrangements, in the classroom and the workplace. This requires liaison and cooperation with the training providers and institutions on the ground.
For clinical training to be relevant, it needs to reflect the learning needs of trainees in the workplace – in keeping with adult learning principles and cognitive apprenticeship models of learning. 14 The latter includes the importance of clinical decision-making underscored by the higher levels of Bloom’s (1956) cognitive domain. 15 To this end, then appropriate learning and assessment methods are needed to enable effecting learning.
In other words, while necessary, TEL may be insufficient in enhancing learning outcomes if allied learning methods are not chosen appropriately. Also, in our view, TEL is not a substitute for bedside teaching.
Table 1 summarises this appraisal of online distance learning (using the online platform provided by MedicineAfrica).
Table 1 Strengths and limitation of using MedicineAfrica (web-based virtual classroom environment)
| Strengths | Limitations |
| Better use of the participants time and resources | Limited or lack of internet access |
| Overcome geographical barriers between two countries | Technical and logistic issues |
| Improve critical thinking and communication skills | Subscription expenses Appropriate choice of learning methods |
| Form long-standing professional networks | Ethical and legal issues (e.g., confidentiality) |
| Interactivity | Lack of direct face to face contact |
OxPIQ & Project Development Team
OxPIQ is a partnership between Medicine Africa and psychiatrist members of the Oxford University Medical Education Fellows, with experience of working in Iraq. The Oxford University Medical Education Fellows (http://OUMEF.org) is a group of trainees from across medical and surgical specialities with interest in medical education and training.
Medicine Africa (http://medicineafrica.com) is an innovative clinically targeted online platform developed in collaboration with King’s College London’s Centre for Global Health, within the King’s Somaliland Partnership. Built at low bandwidth, it enables collaboration between medical professionals in the UK and those in remote or fragile states to enhance education in various clinical specialities using online sessions (live courses and mentoring sessions). Please see Appendix 3 for a screenshot of one of the active sessions of OxPIQ.
Following the development of a project team, additional team members were added from the Subcommittee on Iraq of the Royal College of Psychiatrists (http://www.rcpsych.ac.uk/workinpsychiatry/internationalaffairsunit/iraqs...), thus completing the UK dimension.
The next step was to invite representation and support from the Iraqi Board of Psychiatry and the Medical Education Unit in Baghdad. These developments led to the formal launch of OxPIQ Partnership in March 2016. Later on, the many UK and Iraqi doctors joined the Partnership as tutors and learners.
The Virtual Learning Team: Trainees, Specialty Consultants & Tutors
Iraqi psychiatry trainees were then recruited, and their more pressing learning needs to be appraised based on their views and those of the Iraqi Board of Psychiatry supervisors. Learning needs to emerge included the management of older patients with dementia and functional disorders, assessment and management of children and adolescents (with autism and ADHD for example), forensic patients and those with drug and alcohol addiction. The team thus formed was composed of up to ten psychiatry trainees from Iraq and five senior psychiatrists/tutors each, from Iraq and the UK respectively. A schedule of fortnightly seminars was agreed and published on the learning platform. Case-based discussions were used as the main educational activity during these seminars.
Learning Methods and Processes
As noted earlier, the importance of experiential and constructivist learning methods are key to clinical education. Our literature appraisal revealed that they are essential elements of successful TEL in this context too. 16, 17 To these must be added learner engagement. 18
Virtual or online (anonymised) case-based discussions (CBDs) are valid and reliable learning tools. 16 They are interactive and centred around the students and their learning needs while a facilitator guides the process of learning. Learners are engaged through discussion of actual clinical cases, so preparing learners for real-life experience. 19 Also, expert facilitation and peer feedback to trainees promotes clinical knowledge and skills’ development. 20, 21
Effective small group teaching is characterised by four main strengths: flexibility, interaction, reflexivity and engagement. 22 Flexibility is when the teacher responds to the needs and learning of the students dynamically and helps them to explore wider pedagogic spaces. A higher degree of interactivity is usually seen in small group teaching compared to a larger group. Teachers are better able to continually engage in self-reflection and listen sensitively to students in a small group and observe the dynamics between the members of the group, leading therefore to better reflexivity. Engagement refers to encouraging the students to develop their academic identity and engage in lively debate about the various aspects of the topic discussed.
We aimed to replicate these characteristics. For example, a small group discussion allowed better interaction with each participant (interactivity); the presence of chat windows enables the facilitator to self-reflect on the process, monitor engagement and respond reflexively using questions and answers to stimulate interest and respond flexibly to individual trainee knowledge gaps. Tutors are encouraged to identify trainees’ learning needs and facilitate interactivity, and timely feedback as these are highly valued by the participants and help to keep them motivated and engaged. 18
For further reading in this area, we recommend Brindly and colleagues’ 23 ten strategies to increase students’ motivation towards and engagement with online learning (see table 2).
| Table 2- Strategies to increase engagement in online teaching (modified from Brindly and colleagues, 2009) 23 |
| 1. Transparency of expectations: Making the learning objectives very clear and relevant to the participants learning needs. The teachers must be open to the learners’ suggestions and must be willing to discuss the process and purpose of the educational activities.
2. Clear instructions: The educational activity, its timing, duration, and the technical aspects are described in detail to the participants. They should not be left to ‘try out things’ and must be guided explicitly. 3. Appropriateness of task for group work: For the online activity to succeed, individual versus group tasks should be differentiated. In our example, this may be done by asking the participants to do a particular task before the session (e.g., read about severe and enduring mental illness), and then to work together on producing a formulation for the case discussed. This will increase their motivation to be involved in various tasks. 4. Meaning-making/relevance: The case-based discussions (and any online activity) should have relevance for the participants and aim to enrich their experience in their clinical work. 5. The motivation for participation embedded in course design: It is essential that participants in the online activity understand that the success of the group and the course depend on the individual effort of each participant. 6. The readiness of learners for group work: This aspect describes the development of a sense of community through a professional relationship which leads to better collaborative work. 7. The timing of group formation: Before the participants join in the educational activity, it is preferable to have some discussions before the tutorial on their learning needs to allow a time for rapport to develop to enable better group activities. 8. Respect for the autonomy of learners: Joining and leaving the educational activity (and the whole online course) should be voluntary. No penalties should be attached to leaving the course. Learners should have the freedom to choose what aspects of the online course is relevant to them. 9. Monitoring and feedback: The tutor should monitor the progress of the participants, and timely feedback is given respectfully to enhance the engagement and motivation of the participants. Please see Appendix 1 (lesson plan) for more details on feedback and evaluation. 10. Sufficient time for the task: Participants should be given time to be actively involved in the session. This is particularly important in a distant learning session when issues related to sound quality or speed of internet connection may prevent some participants from engagement. |
The focus of the Lesson Plan Design
To these ends, the focus on the lesson design was on using problem-based learning methods (e.g. CBDs) within a small group setting (between 4-12 members) and a format that promoted learner engagement. A sample lesson plan is provided in Appendix 1.
In practical terms, tutorials were held fortnightly in term-time. All participants received an email notification to inform them of the session topic, and the tutor uploaded the slides from the session to the website beforehand. Participants logged-in to the site (http://medicineafrica.com) and interact with the tutor by voice (requiring only simple microphone equipment) and by writing in a chat window.
Evaluation and feedback gathering
The evaluation of the effectiveness of these sessions was reliant originally on trainees’ immediate reaction (table 3, level 1 evaluation, Kirkpatrick 24) using formal feedback tools provided online by MedicineAfrica. This feedback was shared with tutors and the Project Team. Please see Appendix 2 for the template used in collecting feedback after each session.
Subsequently, members of the project team approached trainee representatives, tutors and Iraqi Psychiatry Board leads separately for further feedback and appraisal of learning needs. Furthermore, some months after a tutorial we have asked trainees for evidence of learning across the higher levels of Kirkpatrick’s evaluation model.
Regular feedback from the Iraqi and UK participants has been positive. The sessions have been associated with improved clinical knowledge and skills of the Iraqi Psychiatry Trainees. Requests for certificates of tutorial participation have been agreed upon and provided by the project team addition, so supporting learners’ (and tutors) portfolio development.
Table 3 Kirkpatrick’s (1996) Levels of Training Assessment
| Level | How to assess |
| Level 1: Reaction (the participants feeling about the training | Feedback during and after the tutorial using the feedback questionnaire |
| Level 2: Learning (improving the participants’ knowledge) | Post-tutorial questionnaire and interviews |
| Level 3: Behaviour-also called Transfer (improving the participant's performance) | Direct or indirect observation and assessment of the skills and competencies of the trainees |
| Level 4: Results (cost-effectiveness, engagement, sustainability, adherence to evidence-based practices) | regular meetings between the participants, tutors, and stakeholders. |
Further cooperation
A surprising (and very welcome) outcome of the project was, through the facilitation and support of the Iraqi Board of Psychiatry, the introduction of educational workshops in Baghdad. These workshops were held in Medical City, Baghdad, in May 2017 and April 2018 and were facilitated by tutors (YH & H Al-T) from the OxPIQ Partnership. They covered targeted topics such as old age psychiatry, addiction, organic and forensic psychiatry. Trainees and senior psychiatrists from Iraq attended; their feedback showed how they valued the interactive nature of the teaching and use of CBDs as learning methods, resulting in high levels of engagement.
Conclusions
This paper describes the process of designing, delivering, and the early evaluation of an online distance TEL programme for mental health professionals based in the UK and Iraq.
TEL has had an important role in overcoming the geographical barriers and other challenges to developing training opportunities in Iraq and other developing countries. We are of the view that it could be used more often to connect professionals working in similar circumstances and with other disadvantaged groups, including refugee and asylum seekers. It is a flexible way of providing training to professionals working with those groups in relatively remote and resource-deprived environments.
Greenhalgh 25 suggests that three factors are needed for the success of online educational activity: ease of access, perceived usefulness of the activity to the learning requirements of the students, and the interactivity of the session. In our experience, these are important. Also, we believe that additional consideration should be given to (i) working with an experienced online platform provider; (ii) working with local educational institutions, trainers and learners to identify unmet learning needs and support existing learning opportunities/programmes; and (iii) adopting an iterative approach to feedback and evaluation.
Appendix 1: Example of a Lesson Plan
| Session title | Case-based discussion on management of severe and enduring mental illness. |
| Duration of session | 60 minutes |
| Tutor | A UK-based Psychiatrist |
| Learner group | Psychiatry Board Trainees and Senior Psychiatrists in Iraq and UK |
| Step 1– Learning outcomes | a) Describe the various stages in the management of the cases discussed during the session.
b) Enhance the participants learning using case-based discussion with peers and seniors in the UK and Iraq. c) Improve the presentation and discussion skills of the participants and their communication skills. d) Explore ethical, cultural, and social issues related to the management of mental disorders and improve cultural competency and awareness. |
| Step 2 – Learning Plan | Introduction to the online tutorial -10 minutes
a) Highlight the learning objectives of the tutorial b) Stimulate the thinking of the participants by asking about their current knowledge of the subject, whether they managed similar cases in their clinical work, and what are their learning needs. c) Outline the tutorial structure and further engage the participants by informing them about other details (e.g., if they can ask the question during or after the case presentation) 2. The tutorial in a case with severe and enduring mental disorder – 30 minutes a) Participants are encouraged to interact with the tutor who should be invited to keep the tutorial interactive. b) The case presented will provide an overview of the patient’s journey from the initial presentation, followed by the investigation, then treatment plans. Discussions of the differential diagnosis are important. c) The tutor will assess the knowledge of the participants by asking questions on the various aspects of the case presentation (e.g., what is your differential diagnosis for a patient presenting with auditory and visual hallucination? What investigations would you request?). 3. Recap and Q&A time- 20 minutes a) Tutor to give a summary of the main learning points from the tutorial and linking these to the learning outcomes presented at the beginning. b) Participants are given enough time to ask questions and to participate actively in the session. |
| Step 3 – Assessment | Before Lesson
Before the tutorial, the tutor should know the current educational curriculum of the participants and their learning outcomes in that subject. UK and Iraqi Psychiatry curriculum are different, and therefore knowing what is relevant is important. Stating the learning outcomes at the beginning of the tutorial will also help in the baseline assessment of the knowledge and skills of the participants. Pre-session questionnaires could be used as well (for example, asking questions on the prognosis of various mental disorders and comparing the participant’s knowledge before and after the session). After the lesson · Ongoing assessment during the tutorial using questions on various aspects related to the case presented. · Questions in the recap section at the end of the tutorial. · Post tutorial feedback forms will allow the participants to give their views about their learning needs and if they feel the tutorial was relevant to their learning outcomes. It is important to provide personalised feedback to the participants about their performance on these assessment tools as this will help them to identify gaps in their knowledge and improve their learning. 26 |
| Step 4 – Resources required | MedicineAfrica is free to join and designed to work well even with low bandwidth. Hence it won’t be affected by slow internet connections which are likely to be the case in developing countries.
Trainees and Tutors will need a computer (desktop or laptop) with an internet connection. No other resources are needed. Recommended readings could be disseminated by email to the trainees after the session. |
| Step 5 – Evaluation | Student evaluation
Gathering feedback is an essential step to influence the learning outcomes favourable and continue to improve the structure and content of the tutorials (After the tutorial, the participants will be asked to fill an electronic feedback form (please see Appendix 2). The form contains various questions with rating (from 1-5, ranging from strongly disagree to strongly agree) on various aspects of the tutorial. These include structure, organisation, the range of aids used and meeting of the learning outcomes. Also, direct feedback from the trainees, tutors, facilitators, and the stakeholders responsible for running the online learning platform is gathered to assess the effectiveness of these tutorials. Teacher evaluation Professionals invest a significant amount of time and efforts in these lessons, and it is imperative to assess how the tutorials could be improved to meet the needs of the trainees and keep them and the tutors motivated and interested. Tutors in these tutorials meet regularly using Skype to reflect on their teaching sessions and discuss ways of improving the delivery and quality of the tutorials. Mutual learning is another aspect that needs to be assessed (is the tutor also benefitting from these lessons, for example, by improving their cultural competencies or their teaching skills). |
Appendix 2: Feedback form to be completed by the participants after the session
| Session title | Case-based discussion on management of severe and enduring mental illness. |
| Speaker | |
| Date | |
| Content | The session was relevant to my training needs
Strongly disagree 1 2 3 4 5 Strongly agree |
| Organisation | Sufficient time was allowed for the session
Strongly disagree 1 2 3 4 5 Strongly agree |
| Presentation | The session was well presented
Strongly disagree 1 2 3 4 5 Strongly agree The session was delivered at the right pace Strongly disagree 1 2 3 4 5 Strongly agree The session was interactive and encouraged discussion/questions Strongly disagree 1 2 3 4 5 Strongly agree |
| Structure | The session was well organised and structured
Strongly disagree 1 2 3 4 5 Strongly agree The aims and objectives of the session were clear Strongly disagree 1 2 3 4 5 Strongly agree The aims and objectives of the session were met Strongly disagree 1 2 3 4 5 Strongly agree |
| Overall evaluation | Overall, I would rate this session as
Extremely poor 1 2 3 4 5 Extremely good |
Appendix 3: MedicineAfrica screenshot during an active session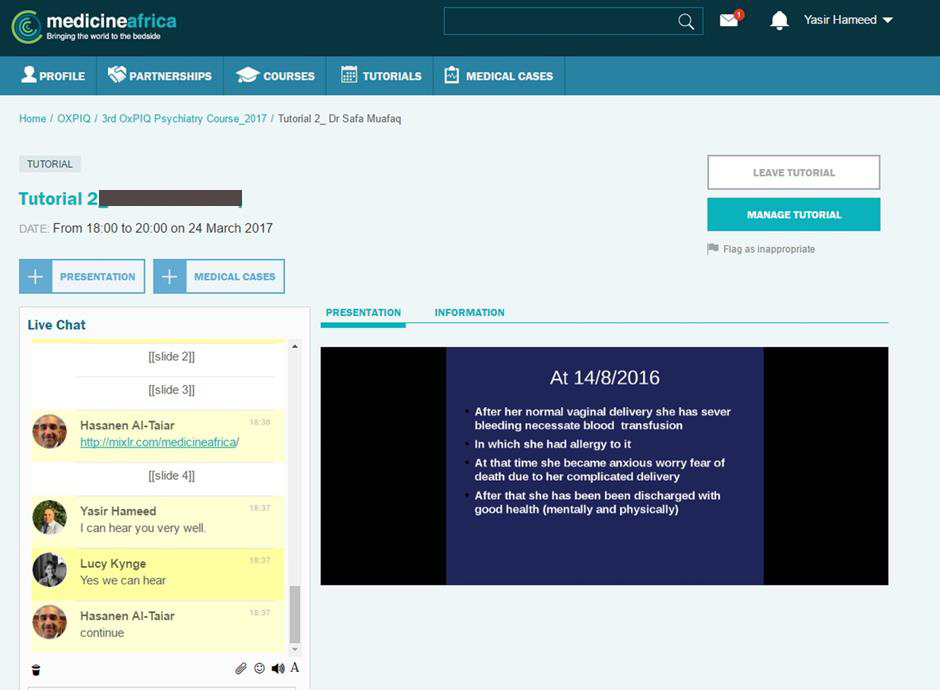
|
Acknowledgements The authors would like to acknowledge the contribution of Dr Nesif Al Hemiary, Head of the Iraqi Board of Psychiatry, Consultant Psychiatrist and Professor of Psychiatry, University of Baghdad for his invaluable support in organising the training workshops in Baghdad. The members of the Subcommittee on Iraq of the Royal College of Psychiatrists (https://www.rcpsych.ac.uk/members/internationalaffairsunit/iraqsubcom.aspx) and its chair, Dr Saleh Dhumad, also provided helpful advice and supported the OxPIQ activities. Competing Interests None declared Author Details YASIR HAMEED; MB ChB, MRCPsych, PgDip Clin Edu, FHEA; Honorary Senior Lecturer, Norwich Medical School University of East Anglia. UK. Consultant Psychiatrist, Norfolk and Suffolk NHS Foundation Trust. UK. HASANEN AL TAIAR; MRCPsych, SFHEA; Consultant Forensic Psychiatrist, Oxford, UK. DENIS O’LEARY; MRCPsych, MD, MEd, SFHEA; Honorary Clinical Tutor (Postgraduate Medicine), Medical Science Division, University of Oxford, UK. LUCY KYNGE, Project Manager, Medicine Africa. CORRESPONDENCE: YASIR HAMEED, Consultant Psychiatrist, Norfolk and Suffolk NHS Foundation Trust, UK. Email: yasirmhm@yahoo.com |
References
- Kirkwood A, Price L. Technology-enhanced learning and teaching in higher education: what is ‘enhanced’ and how do we know? A critical literature review. Learning, Media & Technology. 2014; 39(1): 6-36.
- McCutcheon K, Lohan M, Traynor M, et al. A systematic review evaluating the impact of online or blended learning vs. face-to-face learning of clinical skills in undergraduate nurse education. Journal Of Advanced Nursing 2015; (2): 255-270.
- Means B, Toyama Y, Murphy R, et al. Evaluation of Evidence-Based Practices in Online Learning: A Meta-Analysis and Review of Online Learning Studies. US Department Of Education in 2009.
- Crews T, Butterfield J. Data for Flipped Classroom Design: Using Student Feedback to Identify the Best Components from Online and Face-to-Face Classes. Higher Education Studies 2014; 4(3): 38-47.
- Malhotra A, Majchrzak A, Rosen B. Leading Virtual Teams. Academy Of Management Perspectives 2007; 21(1): 60-70.
- Siemens, G. Connectivism: A learning theory for the digital age. International Journal of Instructional Technology and Distance Learning 2005; 2(1): 3-10.
- Wenger, E. Communities of practice: Learning, meaning and identity. Cambridge, UK: Cambridge University Press, 1998.
- Cifuentes, L. and Shih, Y. Teaching and Learning Online. Journal of Research on Computing in Education 2001; 33(4): 456-474.
- Bruce, T., Byrne, F. and Kemp, L. Using Skype to support remote clinical supervision for health professionals delivering a sustained maternal early childhood programme: a phenomenographical study. Contemporary Nurse 2018; 54(1):4-12.
- Ensher, E., Heun, C. and Blanchard, A. Online mentoring and computer-mediated communication: New directions in research. Journal of Vocational Behavior 2003; 63(2): 264-288.
- Riley JB, Austin JW, Holt DW, et al. Internet-based virtual classroom, and educational management software enhances students’ didactic and clinical experiences in perfusion education experiences. Journal of Extra-corporeal Technology 2004; 36:235–239.
- Chudoba, K. M., Wynn, E., Lu, M., & Watson-Manheim, M. B. How virtual are we? Measuring virtuality and understanding its impact in a global organisation. Information Systems Journal 2005; 15(4): 279-306
- Garrison, D. and Kanuka, H. Blended learning: Uncovering its transformative potential in higher education. The Internet and Higher Education 2004; 7(2): 95-105.
- Knowles MS and Associates. Andragogy in action: applying modern principles of adult learning. San Francisco: Jossey-Bass, 1984.
- Bloom BS, Engelhart MD, Furst EJ, et al. Taxonomy of educational objectives: the classification of educational goals. Handbook I: Cognitive domain. New York: David McKay, 1956.
- Bullock, A., & Webb, K. Technology in postgraduate medical education: a dynamic influence on learning? Postgraduate Medical Journal 2015; 91(1081): 646-650.
- Flynn, L., Jalali, A., & Moreau, K. A. Learning theory and its application to the use of social media in medical education. Postgraduate Medical Journal 2015; 91(1080): 556-560.
- Boston, W., Diaz, S. R., Gibson, A. M., Ice, P., Richardson, J., & Swan, K. An Exploration of the Relationship between Indicators of the Community of Inquiry Framework and Retention in Online Programs. Journal of Asynchronous Learning Networks 2009; 13(3): 67-83.
- Yasin I., T. The Impact of Small Group Case-based Learning on Traditional Pharmacology Teaching. Sultan Qaboos University Medical Journal: SQUMJ 2013; 13 (1): 115-120.
- Thistlethwaite J, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Medical Teacher 2012; 34(6): e421-e444.
- Williamson, J. L., & Osborne, A. J. Critical Analysis of Case-Based Discussions. British Journal Of Medical Practitioners 2012; 5(2): 1-4.
- Mills, D. & Alexander, P. Small group teaching: a toolkit for learning. The Higher Education Academy, 2013. [Accessed on 09 September 2018] https://www.heacademy.ac.uk/system/files/resources/small_group_teaching_1.pdf
- Brindly, J. E., Walti, C., Blaschke, L. M. Creating Effective Collaborative Learning Groups in an Online Environment, 2009. [Accessed on 09 September 2018] http://www.irrodl.org/index.php/irrodl/article/view/675/1271
- Kirkpatrick, D. Great Ideas Revisited. Techniques for Evaluating Training Programs. Revisiting Kirkpatrick's Four-Level Model. Training And Development 1996; 50(1): 54-59.
- Greenhalgh T, Wong G, Pawson R. Internet-based medical education: a realist review of what works, for whom and in what circumstances. BMC Medical Education 2010; 10 (1): 12.
- Kopp, V., Stark, R., & Fischer, M. R. Fostering diagnostic knowledge through computer-supported, case-based worked examples: effects of erroneous examples and feedback. Medical Education 2008; 42(8): 823-829.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




