Burnout among psychiatrists after COVID-19 pandemic
Hong Doan, Ben Harmon-Jones & M Aamer Sarfraz
Cite this article as: BJMP 2021;14(2):a012
|
|
Abstract The concept of burnout has been frequently used to explain stress experienced by healthcare workers. Physicians are at a greater risk due to their high job-related stress. Psychiatry, however, presents a unique range of stressors not encountered in other medical specialties. COVID-19 pandemic caused a huge increase in the pressure on mental health services in the U.K. but limited research has been carried out about its psychological effects on psychiatrists. We carried out a cross-sectional survey of all doctors working in a large county-wide mental health trust in England. Our response rate was 42% (106 out of 254), and we found a burnout rate of 44% among them. We also found that screen time for 2/3 of the respondents had increased by 4 hours, and 41% were dissatisfied with remote consultations and the care they had provided during the pandemic. Poorer patient outcomes in our study could partly be due to job-related difficulties during the pandemic as approx. 62% of our cohort felt that face masks affected their rapport with patients. We believe our findings are significant but lack a pre-COVID survey for validation and need further examination though larger multi-site studies. Keywords: Burnout, pandemic, stressor, psychiatristsAbbreviations: COVID-19, NHS |
INTRODUCTION
The concept of burnout has been used to describe emotional and psychological stress among healthcare workers in response to work-related stressors1. Maslach et al2 have defined burnout as a triad of characteristics: emotional exhaustion, depersonalisation (such as objectifying and treating patients indifferently) and lack of feelings of personal accomplishment. Since high time-pressure, high job- stress and excessive workload with poor support are among significant factors that contribute to burnout, physicians are at a greater risk of suffering from it as compared to the general population3.
Burnout affects approx. half of the doctors in the U.S. and in Western Europe working across multiple specialties including in family medicine and internal medicine4,5. Likewise, burnout is universally prevalent among healthcare workers from low and middle-income countries6.
Psychiatry presents specific range of stressors not encountered concurrently in other medical specialties, such as treating chronically ill patients, potentially difficult therapeutic relationships, threat of patient suicide/self-harm and stigma associated with this field of medicine7. Therefore, it is not surprising to discover that approx. 37% of psychiatric trainees working across 22 countries suffered from severe burnout8.
The COVID-19 pandemic resulted in a national lockdown in the U.K. with travel restrictions and unprecedented pressure on an already stretched healthcare system. Healthcare workers were, therefore, faced with extraordinary difficulties including increased working hours, heavy workload, staff shortages and lack of resources. A recent systematic review showed that a startling 40% of medical workers experienced acute stress disorder following COVID-19 pandemic, with burnout prevalent among 29% of them9.
During to the pandemic, there has been a huge increase in the pressure on mental health related admissions to hospitals10. A number of causative stressors may have instigated further strain on mental health workers, including bereavement, unemployment, and isolation, resulting in increased psychological morbidity11. Under such circumstances, ensuring the wellbeing of healthcare workers is of paramount importance to maintain a resilient healthcare system. However, limited research has been carried out so far on the effects of pandemics on psychiatrists and other frontline healthcare workers.
Following two surges of COVID-19 pandemic, we proposed to ascertain the frequency of burnout among doctors working in a large mental health trust in Southeast England, with a secondary aim of exploring possible contributory factors.
METHODOLOGY
We carried out a cross-sectional survey of all doctors working in a county-wide mental health Trust in England. Using the NHS Mail, a link to complete the online survey was sent to all doctors working at different experience levels and across a number of psychiatric specialties.
The survey was based on The Maslach Burnout Inventory12, which is considered to be a gold standard in assessing burnout among healthcare workforce. It consists of 22 questions, divided into domains that assess emotional exhaustion, depersonalisation and personal accomplishment based on a 7-point scale, ranging from “never” to “every day”. Scores for these domains range from 0 to 54, 0 to 30, and 0 to 48, respectively. High scores on the EE (≥ 30) and DP (≥ 12) subscales or a low score on the PA subscale (≤ 30) were considered highly suggestive of burnout symptoms.
The anonymised survey contained questions related to demographics, 22 questions as derived from the Maslach Burnout Inventory, and 14 other questions exploring specific work-related stressors regarding the COVID-19 pandemic. Responses to the questions were analysed and categorised into themes to allow further analysis and discussion.
RESULTS
Our response rate was 42% as 106 out of 254 doctors filled the questionnaire. Not all participants answered all questions, and response numbers for each question are indicated where applicable in the respective tables. There was an even distribution between trainees and consultants, but less representation from speciality doctors, which was expected due to their fewer numbers. Where gender was equally split, we found that age was relatively evenly distributed in our sample.
Figure 1: Participant demographics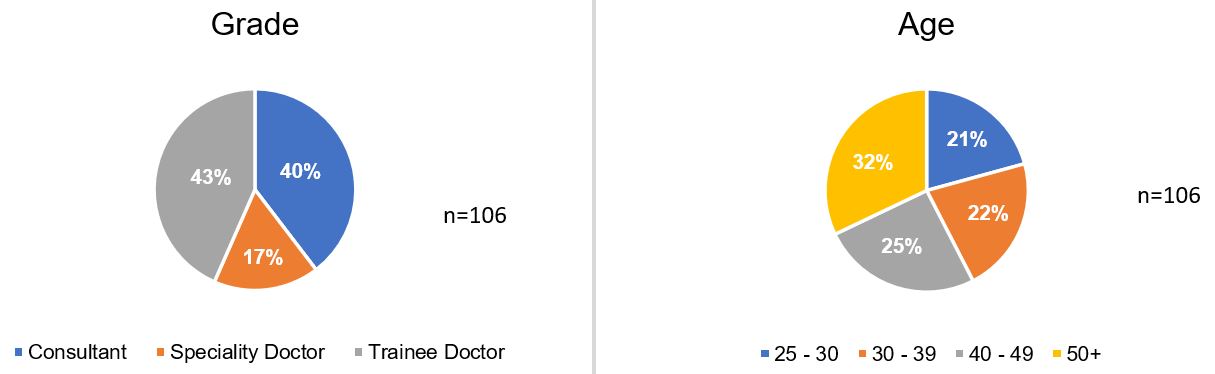
Regarding the Maslach Burnout Inventory questions, higher aggregates in emotional exhaustion and depersonalisation subscales indicate higher chance of burnout. When comparing these two subscales, the levels of emotional exhaustion were higher than that of depersonalisation. Conversely, in the personal accomplishment subscale, more common occurrences indicate a lower chance of burnout.
Table 1: Maslach Burnout Inventory Results
| Question | Possible responses | n | ||||||
| Never | A few times/ year | Once/ month | A few times/ month | Once/ week | A few times/ week | Every day | ||
| I feel emotionally drained by my work | 7.6% (8) | 23.8% (25) | 10.5% (11) | 27.6% (29) | 6.7% (7) | 20% (21) | 3.8% (4) | 105 |
| Working with people all day long requires a great deal of effort | 11.3% (12) | 23.6% (25) | 11.3% (12) | 26.4% (28) | 5.7% (6) | 16.0% (17) | 5.7% (6) | 106 |
| I feel like my work is breaking me down | 20.0% (21) | 39.0% (41) | 9.6% (10) | 18.1% (19) | 1.9% (2) | 9.6% (10) | 1.9% (2) | 105 |
| I feel frustrated by my work | 16.2% (17) | 33.3% (35) | 10.5% (11) | 21.9% (23) | 5.7% (6) | 10.5% (11) | 1.9% (2) | 105 |
| I feel I work too hard at my job | 12.4% (13) | 21.0% (22) | 8.6% (9) | 25.7% (27) | 5.7% (6) | 17.1% (18) | 9.5% (10) | 105 |
| It stresses me too much to work in direct contact with people | 46.2% (49) | 28.3% (30) | 9.4% (10) | 7.5% (8) | 0.9% (1) | 4.7% (5) | 2.8% (3) | 106 |
| I feel like I’m at the end of my tether | 42.9% (45) | 33.3% (35) | 4.8% (5) | 6.7% (7) | 2.9% (3) | 7.6% (8) | 1.9% (2) | 105 |
| I feel I deal with my team/colleagues impersonally, as if they are objects | 70.8% (75) | 19.8% (21) | 4.6% (5) | 2.8% (3) | 0.9% (1) | 0.0% (0) | 0.9% (1) | 106 |
| I feel tired when I get up in the morning and have to face another day at work | 15.1% (16) | 36.8% (39) | 13.2% (14) | 11.3% (12) | 1.9% (2) | 17.0% (18) | 4.6% (5) | 106 |
| I have the impression that my team/colleagues make me responsible for some of their problems | 41.0% (43) | 21.9% (23) | 10.5% (11) | 20% (21) | 0.0% (0) | 4.8% (5) | 1.9% (2) | 105 |
| I am at the end of my patience at the end of my work day | 31.7% (33) | 36.5% (38) | 5.8% (6) | 11.5% (12) | 3.8% (4) | 9.6% (10) | 0.9% (1) | 104 |
| I really don’t care about what happens to some of my team/colleagues | 85.7% (90) | 6.7% (7) | 1.9% (2) | 1.9% (2) | 1.9% (2) | 0.9% (1) | 0.9% (1) | 105 |
| I have become more insensitive to people in the workplace | 67.0% (71) | 22.4% (24) | 2.8% (3) | 3.8% (4) | 0.9% (1) | 2.8% (3) | 0.0% (0) | 106 |
| I’m afraid that this job is making me uncaring | 62.3% (66) | 25.5% (27) | 2.8% (3) | 1.9% (2) | 3.8% (4) | 1.9% (2) | 1.9% (2) | 106 |
| I accomplish many worthwhile things in this job | 2.9% (3) | 8.6% (9) | 6.7% (7) | 15.2% (16) | 6.7% (7) | 25.7% (27) | 34.3% (36) | 105 |
| I feel full of energy | 4.7% (5) | 6.6% (7) | 8.5% (9) | 20.8% (22) | 8.5% (9) | 33.0% (35) | 17.9% (19) | 106 |
| I am easily able to understand what my team/colleagues feel | 0.9% (1) | 2.8% (3) | 3.8% (4) | 13.2% (14) | 8.5% (9) | 34.0% (36) | 36.8% (39) | 106 |
| I look after my team/colleagues problems very effectively | 0.9% (1) | 1.9% (2) | 5.8% (6) | 12.5% (13) | 7.7% (8) | 44.2% (46) | 26.9% (28) | 104 |
| In my work, I handle emotional problems very calmly | 0.9% (1) | 4.8% (5) | 1.9% (2) | 2.9% (3) | 13.3% (14) | 31.4% (33) | 44.8% (47) | 105 |
| Through my work, I feel that I have a positive influence on people | 0.9% (1) | 4.8% (5) | 4.8% (5) | 8.6% (9) | 9.5% (10) | 38.1% (40) | 33.3% (35) | 105 |
| I am easily able to create a relaxed atmosphere with my team/colleagues | 0.9% (1) | 3.8% (4) | 2.8% (3) | 9.4% (10) | 11.3% (12) | 34.0% (36) | 37.7% (40) | 106 |
| I feel refreshed when I have been close to my team/colleagues | 1.9% (2) | 8.5% (9) | 3.8% (4) | 17.0% (18) | 11.3% (12) | 34.9% (37) | 22.6% (24) | 106 |
In other quantitative questions, all respondents reported that their screen time had increased during the pandemic. A majority reported it to be by more than 2 hours/week, and 71% registered an increase of more than 4 hours/week. Despite this, there appears to be no increase in their home-working that could account for this difference.
The results of the remaining questions reflected a poorer work experience. The strongest evidence was for a feeling that mask wearing had affected rapport with patients. Other more common experiences included poor outcomes for patients during the pandemic, with decreased staffing levels, increased workload, and delayed treatments.
Table 2: Other Question Responses – Quantitative only
| Question | Possible responses | n | ||||
| 0-1 hours | 1-2 hours | 2-3 hours | 4-6 hours | 6 hours + | ||
| During the pandemic, my screen time (e.g. due to meetings and teaching) increased by | 4.0% (4) | 5.0% (5) | 20.0% (20) | 37.3% (37) | 33.3% (33) | 99 |
| Question | Possible responses | n | ||||
| Yes | No | |||||
| Were you working from home more often during the pandemic? | 48%(48) | 52%(52) | 100 | |||
| Question | Possible responses | n | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree | ||
| I felt that the increase in screen time negatively affected my mood | 10.0% (10) | 23.0% (23) | 35.0% (35) | 24.0% (24) | 8.0% (8) | 100 |
| I felt that the increase in screen time increased my level of exhaustion | 14.3% (14) | 16.3% (16) | 19.4% (19) | 39.8% (39) | 10.2% (10) | 98 |
| I felt that the increase in screen time resulted in depersonalisation of my patients | 11.0% (11) | 25.0% (25) | 33.0% (33) | 25.0% (25) | 6.0% (6) | 100 |
| I felt that the increased screen time hindered the working relationship between colleagues | 10.0% (10) | 25.0% (25) | 20.0% (20) | 33.0% (33) | 12.0% (12) | 100 |
| I felt that the increase in screen time resulted in feelings of burnout | 17.0% (17) | 26.0% (26) | 27.0% (27) | 23.0% (23) | 7.0% (7) | 100 |
| I felt dissatisfied with my online/telephone consultations | 8.2% (8) | 31.6% (31) | 41.8% (41) | 13.3% (13) | 5.1% (5) | 98 |
| I felt that wearing masks affected my rapport with patients | 8.1% (8) | 17.1% (17) | 9.1% (9) | 49.5% (49) | 16.2% (16) | 99 |
| I felt dissatisfied with the patient care provided to patients during the pandemic | 7.1% (7) | 36.4% (36) | 33.3% (33) | 21.2% (21) | 2.0% (2) | 99 |
| I felt that patients did have poorer outcomes during the pandemic | 5.1% (5) | 27.2% (27) | 28.3% (28) | 35.4% (35) | 4.0% (4) | 99 |
| I felt that working from home affected my work-life balance | 10.4% (10) | 24.0% (23) | 42.7% (41) | 17.7% (17) | 5.2% (5) | 96 |
| I felt that working from home resulted in increased work related stressors | 12.5% (12) | 30.2% (29) | 37.5% (36) | 18.8% (18) | 1% (1) | 96 |
| I felt that working from home resulted in more difficulties in my job e.g. communicating with my team or patient | 11.5% (11) | 29.2% (28) | 35.4% (34) | 21.9% (21) | 2.0% (2) | 96 |
DISCUSSION
Our study provides a snapshot of difficulties encountered by different grades of psychiatrists, while working in a large English county, during the COVID-19 pandemic. We found a burnout rate of 44.2%, which is higher than 36.7% observed by Jovanović et al8 among those working in other countries before the pandemic. Since a higher prevalence is also documented in other recent studies13, it is reasonable to assume that the higher rate of burnout is due to increased work-related stressors during the COVID-19 pandemic. These stressors could be linked to the newly introduced guidelines, which involved social distancing, high staff sickness and redeployment.
In the personal accomplishment subset of our study, highest number of doctors experienced burnout, possibly suggesting a link to the COVID-19 pandemic. Unfortunately, we do not have a pre-COVID pandemic survey for the sake of comparison, which could have confirmed causality with greater certainty.
71% of our cohort reported an increase of more than 4 hours of computer screen time a week, which was not due to increased amount of working from home. Various factors could explain this finding including the introduction of remote medical consultations, online multidisciplinary team meetings and teaching/training. Virtual consultations may provide an alternative to face-to-face assessments, but complications such as difficulty in discussing sensitive topics and demonstrating empathy could influence therapeutic relationship, medical errors, and screen fatigue resulting in increased levels of burnout14, 15.
A compromised professional identity and reduced job satisfaction are considered among significant predictors of job burnout16, 17. It is, therefore, reasonable to question whether the increased screen time and reduced patient contact could have impacted the professional identity of our cohort and their job satisfaction. This could also provide possible explanation for our cohort scoring highly for low personal accomplishment. However, one study that examined burnout in medical residents, who had used virtual telemedicine to replace outpatient clinics, found that the burnout actually decreased with increased use of virtual consultations18. Therefore, more consideration and research needs to be conducted on telemedicine practices in different medical subspecialties and their impact on medical professionals’ working lives.
Burnout is associated with an increase in clinical errors and may manifest in irritability, fatigue, and reduced cognitive functioning that ultimately result in a reduction in quality of patient care12,19. Medical errors on the other hand cost the National Health Service (NHS) £3.3 billion in litigation costs and additional bed days due to both systemic and individual factors20. Overall, 41% of our cohort were dissatisfied with remote consultations and the care provided to their patients during the pandemic. The reported difficulties with providing good patient care primarily consisted of poorer quality of and reduced patient interaction, patients being unable to engage with services and delayed treatments.
Wearing face masks could affect both verbal and non-verbal communication that in turn hinder the therapeutic relationship, as previous research has shown that patient engagement, understanding and treatment success are influenced by a clinician’s facial expressions21. Poorer patient outcomes found in our study could partly be due to the difficulties experienced during the pandemic as approx. 62% of our cohort felt that face masks affected their rapport with patients. Other factors that could have contributed to these poorer outcomes include redeployment of staff due to NHS pressures and reduced services. Further work is, however, needed to ascertain the associated casual pathway.
During the height of pandemic, carrying out frenetic clinical work with limited resources and little respite, coupled with the loss of loved ones and colleagues, could have undoubtedly impacted the mental health of medical workforce including psychiatrists. On the other hand, the pandemic may have also heightened the sense of vocation for some doctors. It is, therefore, difficult to assess the lasting effects of burnout until the pandemic is finally over and we resume normal therapeutic practices, in both clinical and personal settings.
|
Competing Interests None declared Author Details HONG DOAN (Foundation Trainee), BEN HARMON-JONES (Psychiatry trainee) & M AAMER SARFRAZ CORRESPONDENCE: Prof M AAMER SARFRAZ, Elizabeth Raybould Centre, Bow Arrow Lane, Dartford DA2 6PB. Email: Amer.Sarfraz@Canterbury.ac.uk |
References
- Maslach, C, Jackson, SE, Leiter MP. Maslach Burnout Inventory. In Evaluating stress: A book of resources , C. P. Zalaquett & R. J. Wood. 1997; 191-218.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001; 52: 397-422.
- Tait DS, Sonja B, Litjen T, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012 Oct 8;172(18):1377-85.
- Soler JK, Yaman H, Esteva M, et al. European General Practice Research Network Burnout Study Group. Burnout in European family doctors: the EGPRN study. Fam Pract 2008; 25 (4): 245-65.
- Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med 2014; 9(3): 176-81.
- Dugani S, Afari H, Hirschhorn LR, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: A systematic review. Gates Open Res 2018; 11.
- Rössler, W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin Neurosci 2012; 262: 65-9.
- Jovanović N, Podlesek A, Volpe U, et al. Burnout syndrome among psychiatric trainees in 22 countries: Risk increased by long working hours, lack of supervision, and psychiatry not being first career choice. Eur Psychiatry 2016; 32: 34-41.
- Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord 2020; 277: 347-357.
- Grimshaw B, Chaudhuri E. Mental-health-related admissions to the acute medical unit during COVID-19. Clin Med (Lond) 2021; 21 (1): 77-79.
- Jia R, Ayling K, Chalder T, Massey A, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open 2020; 10 (9).
- Maslach, C., Jackson, S. E., & Leiter, M. P. The Maslach burnout inventory-test manual. Palo Alto 1996.
- Lasalvia A, Amaddeo F, Porru S, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open 2021; 11 (1).
- Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106-114.
- Shachak A, Alkureishi MA. Virtual care: a 'Zoombie' apocalypse? J Am Med Inform Assoc 2020; 27 (11): 1813-1815.
- Scanlan JN, Hazelton T. Relationships between job satisfaction, burnout, professional identity and meaningfulness of work activities for occupational therapists working in mental health. Aust Occup Ther J 2019; 66 (5): 581-590.
- Chen H, Liu F, Pang L, et al. Are You Tired of Working amid the Pandemic? The Role of Professional Identity and Job Satisfaction against Job Burnout. Int J Environ Res Public Health 2020; 17 (24).
- Mills K, Peterson A, McNair M, et al. Virtually Serving the Underserved: Resident Perceptions of Telemedicine Use While Training During Coronavirus Disease 2019. Telemed J E Health; 2021.
- Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg 2010; 251 (6): 995-1000.
- Department of Health. An Organisation with a Memory: Report of an Expert Group on Learning from Adverse Events in the NHS. 2000: The Stationery Office .
- Ambady N, Koo J, Rosenthal R, Winograd CH. Physical therapists' nonverbal communication predicts geriatric patients' health outcomes. Psychol Aging 2002; 17 (3): 443-452.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




