Assessment of risk factors and precipitating factors of delirium in patients admitted to intensive care unit of a tertiary care hospital
Nikita Nagari & M Suresh Babu
Cite this article as: BJMP 2019;12(2):a011
|
|
Abstract Background and Aim: Delirium is defined as disturbance in attention and awareness. Delirium is a common complication in patients admiited to intensive care unit. The focus of the researchers has shifted from treatment to prevention of the syndrome. There is a need to study risk factors for prevention of delirium. Data on delirium in intensive care unit is scarce in the Indian subcontinent. Hence, the present study was done to assess risk factors and precipitating factors of delirium in patients admitted to medical intensive care unit of a tertiary care hospital. Abbreviations: CAM-ICU= Confusion Assessment Method for ICU, ICU = Intensive Care Unit, RASS= Richmond Agitation-Sedation Scale, OR = Odds ratio |
Introduction:
According to DSM V, delirium is defined as disturbance in attention (i.e., reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment). This disturbance develops over a short period of time and it represents an acute change from baseline attention and awareness, and tends to fluctuate in severity during the course of a day.
The focus of the researchers has shifted from treatment to prevention of the syndrome. There is a need to study risk factors for prevention of delirium1. Data on delirium in the intensive care unit is scarce in the Indian subcontinent2.
A multicenter study indicated risk factors significantly contributing to delirium were related to patient characteristics (smoking, daily use of more than 3 units of alcohol, living alone at home), chronic pathology (pre-existing cognitive impairment), acute illness (use of drains, tubes, catheters, use of psychoactive medication, a preceding period of sedation, coma, mechanical ventilation) and the environment (isolation, absence of visit, absence of visible daylight, transfer from another ward, use of physical restraints)1. Psychoactive medications can provoke a delirious state. Lorazepam has an independent and dose related temporal association with delirium3.
Each additional day spent in delirium is associated with 20% increased risk of prolonged hospitalisation and 10% increased risk of death4.
Hence, the present study was done to assess risk factors and precipitating factors of delirium in a medical intensive care unit of a tertiary care hospital.
Materials and methods:
This is an observational study done over a period of 1 year in a tertiary care medical college hospital located in southern part of India. Ethical committee approval for the study was obtained from the institutional ethical committee.
All patients admitted to medical intensive care unit in our tertiary care hospital, were screened for presence of delirium during the first 72 hours of admission using Richmond Agitation Sedation Scale (RASS) and Confusion Assessment Method for ICU (CAM-ICU). Patients with delirium were classified as delirious and the remaining as non-delirious patients. Comatose patients (RASS score -4 or -5) were excluded from the study.
Patients were initially screened with Richmond Agitation Sedation Scale (RASS). It is a 10-point scale, with 4 levels of agitation (+1 to +4) and 5 levels of sedation (-1 to -5). Level zero indicates calm and alert patient. Patients with RASS score of -4 or -5 (deep sedation and unarousable patients) were excluded from the study. Patients with RASS score of +4 to -3 were then screened for presence of delirium using Confusion Assessment Method for ICU (CAM-ICU). CAM–ICU has 4 criteria:
1) Acute onset and fluctuating course of delirium
2) Inattention
3) Disorganized thinking
4) Altered level of consciousness
The diagnosis of delirium requires the presence of criteria 1 and 2 and of either criterion 3 or 4.
Risk factors for developing delirium were assessed in the study population. Risk factors are those proven factors which may also be present before patient’s admission to intensive care unit, and which predispose the patient to develop delirium. Risk factors were compared between delirious and non-delirious patients. Risk factors which were assessed were history of diabetes and hypertension, history of previous stroke, history of previous cognition impairment, history of previous psychiatric illness, history of previous trauma, history of previous episodes of delirium, history of bowel and bladder disturbances prior to admission (such as constipation and urinary retention respectively), history of alcohol abuse (consumption of more than 2 units of alcohol), history of smoking (more than 10 cigarettes per day), history of consumption of substances other than cigarettes and alcohol (such as cannabis, cocaine etc.), history of uncorrected visual or hearing disturbances before admission, history of usage of barbiturates (such as phenobarbital), benzodiazepines (such as alprazolam, chlordiazepoxide, clobazam, clonazepam) & opioids (such as morphine) before admission, history of usage of sedatives (such as haloperidol, midazolam, fentanyl) and pain killers (such as morphine, tramadol) at the time of admission. Metabolic risk factors which were compared between delirious and non-delirious subjects were uraemia, hyponatremia, hyperbilirubinemia, metabolic and respiratory acidosis.
Precipitating factors weredefined as factors that were the likely causes of delirium in delirious patients. Precipitating factors for delirium which were looked into were exposure to toxins (alcohol/drugs), deranged metabolic parameters, infections and central nervous system causes.
SPSS21 software was used to calculate statistics. Independent t-sample test and the Pearson Chi-square test were used to calculate differences between delirious and non-delirious subjects. Odds ratios (OR) was calculated for all factors using univariate binary logistic regression.
Results:
Total number of patients enrolled in the study was 1582, of which 406 were diagnosed with delirium. Percentage of patients developing delirium within first 72 hours of admission was 25.7%. Hypoactive delirium was present in 52% and hyperactive delirium in 48% of patients. Patients who experienced delirium (57.5 + 17 years) were older compared to their non-delirious (53.3 + 18.1 years) counterparts (p value <0.0001). Among delirious subjects, majority were in the age group of 61-70 years (Figure 1).
Figure 1- Age distribution among delirious patients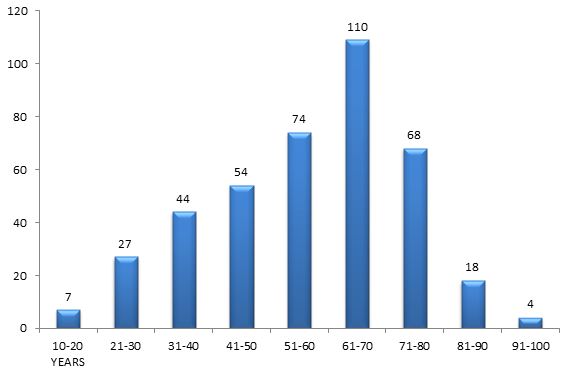
38.2% of delirious patients and 39.3% of non-delirious patients were females. 61.8% of delirious patients and 60.7% of non-delirious patients were males.
Alcohol consumption [OR = 6.54 (95% CI 3.76-11.4, p = 0.0001)], previous psychiatric illness [OR = 3.73 (95% CI 1.712-8.159, p = 0.033)], previous cognition impairment [OR = 2.739 (95% CI 1.509-4.972, p = 0.001)], sedatives usage at the time of admission [OR = 2.488 (95% CI; 1.452-4.264), p = 0.001)], visual disturbances [OR = 2.227 (95% CI; 1.328-3.733, p = 0.002)], bowel and bladder disturbances [OR = 1.677 (95% CI 1.044-2.693, p = 0.032)] were significant risk factors contributing to delirium after univariate analysis (Table 1). Metabolic acidosis [OR = 1.996 (95% CI 1.469-2.711, p = 0.0001)] and hyperbilirubinemia [OR = 1.448 (95% CI 1.111-1.886, p = 0.006)] were significant metabolic parameters contributing to delirium after univariate analysis (Table 2).
Precipitating factors (Table 3) for delirium are those factors that were considered the most likely causes of delirium among the delirious patients. Precipitating factors for delirium were classified into toxins, deranged metabolic parameters, infections and central nervous system causes, of which metabolic parameters were most common. Among metabolic parameters, uraemia (25.1%), hepatic encephalopathy (22.7%) and hyponatremia (19.5%) contributed to the majority of cases with delirium.
Table 1 – Univariate analysis of risk factors of delirium
|
NO DELIRIUM |
DELIRIUM |
||||||
| COUNT | % | COUNT | % | P | UNIVARIATE | ||
|
Diabetes |
No | 729 | 62 | 226 | 55.7 | .025 | 1.3(1.1-1.6) |
| Yes | 447 | 38 | 180 | 44.3 | |||
|
Hypertension |
No | 684 | 58.2 | 239 | 58.9 | .8 | .97(0.8-1.2) |
| Yes | 492 | 41.8 | 167 | 41.1 | |||
|
History of Stroke |
No | 1107 | 94.1 | 379 | 93.3 | .6 | 1.14(0.7-1.8) |
| Yes | 69 | 5.9 | 27 | 6.7 | |||
|
Previous memory disturbances |
No | 1149 | 97.7 | 264 | 89.7 | <.0001 | 4.9(2.9-8) |
| Yes | 27 | 2.3 | 42 | 10.3 | |||
|
Previous psychiatric illness |
No | 1161 | 98.7 | 386 | 95.1 | <.0001 | 4(2-7.9) |
| Yes | 15 | 1.3 | 20 | 4.9 | |||
|
Trauma |
No | 1137 | 96.7 | 396 | 97.8 | .3 | 0.6(0.3-1.3) |
| Yes | 39 | 3.3 | 9 | 2.2 | |||
|
Previous episodes of delirium |
No | 1155 | 98.2 | 402 | 99 | .3 | 0.55(0.2-1.6) |
| Yes | 21 | 1.8 | 4 | 1.0 | |||
|
Bowel & bladder disturbances |
No | 1107 | 94.1 | 350 | 86.2 | <.0001 | 2.6(1.8-3.7) |
| Yes | 69 | 5.9 | 56 | 13.8 | |||
|
Alcohol |
No | 1089 | 92.6 | 336 | 82.8 | <.0001 | 2.6(1.8-3.7) |
| Yes | 87 | 7.4 | 70 | 17.2 | |||
|
Smoking |
No | 981 | 83.4 | 354 | 87.2 | .07 | 0.7(0.5-1.03) |
| Yes | 195 | 16.6 | 52 | 12.8 | |||
|
Other substance abuse (apart from cigarettes and alcohol) |
No | 1071 | 91.1 | 391 | 96.3 | .001 | 0.4(0.22-0.6) |
| Yes | 105 | 8.9 | 15 | 3.7 | |||
|
Visual disturbances |
No | 1062 | 90.3 | 298 | 73.4 | <.0001 | 3.4(2.5-4.5) |
| Yes | 114 | 9.7 | 108 | 26.6 | |||
|
Hearing disturbances |
No | 1104 | 93.9 | 338 | 83.3 | <.0001 | 3.1(2.2-4.4) |
| Yes | 72 | 6.1 | 68 | 16.7 | |||
|
Barbiturates |
No | 1155 | 98.2 | 401 | 98.8 | .5 | 0.7(0.3-1.8) |
| Yes | 21 | 1.8 | 5 | 1.2 | |||
|
Benzodiazepines |
No | 1155 | 98.2 | 400 | 98.5 | .7 | 0.8(0.3-2.1) |
| Yes | 21 | 1.8 | 6 | 1.5 | |||
|
Opioids |
No | 1176 | 100 | 405 | 99.8 | .9 | 4.7(0-IN) |
| Yes | 0 | .0 | 1 | .2 | |||
|
Sedatives usage in present admission |
No | 1143 | 97.2 | 369 | 90.9 | <.0001 | 3.5(2.1-5.6) |
| Yes | 33 | 2.8 | 37 | 9.1 | |||
|
Pain killers usage in present admission |
No | 1080 | 91.8 | 400 | 98.5 | <.0001 | 0.17(0.07-0.39) |
| Yes | 96 | 8.2 | 6 | 1.5 | |||
Table 2- Univariate analysis of metabolic parameters
|
NO DELIRIUM |
DELIRIUM |
||||||
| COUNT | % | COUNT | % | P | UNIVARIATE | ||
|
Uraemia |
NO | 648 | 55.1 | 186 | 45.8 | 0.001 | 1.45(1.2-1.8) |
| YES | 528 | 44.9 | 220 | 54.2 | |||
|
Hyponatremia |
NO | 645 | 54.8 | 202 | 49.8 | 0.08 | 1.2(0.98-1.5) |
| YES | 531 | 45.2 | 204 | 50.2 | |||
|
Hyperbilirubinemia |
NO | 837 | 71.2 | 246 | 60.7 | <0.0001 | 1.6(1.3-2) |
| YES | 339 | 28.8 | 159 | 39.3 | |||
|
Metabolic acidosis |
NO | 990 | 84.2 | 286 | 70.4 | <0.0001 | 2.2(1.7-2.9) |
| YES | 186 | 15.8 | 120 | 29.6 | |||
|
Respiratory acidosis |
NO | 1092 | 92.9 | 377 | 92.9 | 1 | 1(0.6-1.5) |
| YES | 84 | 7.1 | 29 | 7.1 | |||
Table 3- Precipitating factors of delirium in the present study
|
PRECIPITATING FACTORS |
% | |
|
Toxins |
Drug or Alcohol overdosage | 1.5 |
| Alcohol withdrawal | 2.7 | |
|
Metabolic conditions |
Hyponatremia | 19.5 |
| Hyperglycaemia | 6.2 | |
| Hypoglycaemia | 2.5 | |
| Hypercarbia | 5.7 | |
| Uraemia | 25.1 | |
| Hepatic encephalopathy (hyperammonemia) | 22.7 | |
|
Infections |
Systemic infective causes | 16.5 |
| Meningitis/ Encephalitis | 8.9 | |
|
Central Nervous System causes |
Hypoperfusion states | 14.5 |
| Hypertensive encephalopathy | 5.9 | |
| Cerebrovascular accident (CVA) | 7.6 | |
| Intracranial space occupying lesion (ICSOL) | 5.4 | |
| Seizures | 10.3 | |
| Psychiatric illness | 4.9 | |
Discussion:
Delirium is classified into hyperactive, hypoactive and mixed type. Hyperactive subtype is present if there is definite evidence in the previous 24 hours of at least two out of the following factors - increased quantity of motor activity, loss of control activity, restlessness, wandering. Hypoactive subtype is present if there is definite evidence in the previous 24 hours of at least two of the following factors - decreased amount of activity, decreased speed of actions, reduced awareness of surroundings, decreased amount of speech, decreased speed of speech, listlessness, reduced alertness, withdrawal. Mixed subtype is present if there is evidence of both hyperactive and hypoactive subtypes in the previous 24 hours5. Percentage of patients with hypoactive delirium was high in this study (52%). Hypoactive delirium often carries relatively poor prognosis, occurs more commonly in elderly patients and is frequently overlooked or misdiagnosed as having depression or a form of dementia.
In the present study, delirium was more prevalent in the elderly population. Most of the elderly patients will have multiple risk factors making them more vulnerable to delirium. Delirium is often the only sign of an underlying serious medical illness in an elderly patient and particular attention should be given to identify and correct the underlying illness.
History of alcohol consumption of more than 2 units per day, prior to admission of the patient, was the major risk factor contributing to delirium in this study (OR = 6.54). This was similar to other studies done by Bart1 et al & Ouimet6 et al where consumption of more than 3 units of alcohol (OR 3.23) & 2 units of alcohol (OR 2.03) respectively, was a significant risk factor for delirium. Patients with a previous psychiatric illness were at increased risk for delirium in this study (OR – 3.73). However, other studies explaining its importance in contributing to delirium were not available. Previous cognition impairment was a significant risk factor contributing to delirium (OR = 2.73). The study by Bart1 et al found that previously diagnosed dementia was an important risk factor (OR = 2.41). Positive correlation with dementia was reported by McNicoll et al7 (RR 1.4) and Pisani et al8 (OR 6.3). Usage of sedatives (OR = 2.48) at the time of admission was a significant risk factor for developing delirium. Bart1 et al found that use of psychoactive medication may disturb the neurotransmission in the brain provoking a delirious state and use of benzodiazepines is a risk factor for delirium (OR – 3.34). Pandharipande3 et al found that Lorazepam was an independent risk factor for daily transition to delirium (OR – 1.2). Pisani8 et al found that use of benzodiazepines was a significant risk factor for developing delirium with odds ratio of 3.4. Uncorrected visual disturbances were a significant risk factor for developing delirium in this study (OR-2.22). Inouye9 et al found that vision impairment (adjusted relative risk – 3.5) was an independent baseline risk factor for delirium. Bowel and bladder disturbances were a significant risk factor contributing to delirium in this study (OR – 1.67). Morley10 opined that constipation is a frequent, often overlooked precipitating factor for delirium. Tony11 et al was of the opinion that a careful history and physical, including a rectal examination with consideration of disimpaction, may be helpful in assessing and managing delirious patients. Waardenburg12 concluded that significant urinary retention can precipitate or exacerbate delirium, a disorder referred to as cystocerebral syndrome. Liem and Carter13 suggested that increased sympathetic tone and catecholamine surge triggered by the tension on the bladder wall may contribute to delirium. Metabolic acidosis and hyperbilirubinemia were significant metabolic parameters contributing to delirium in this study.Similar findings were reported by Aldemir14 et al.
Among delirious patients, most common precipitating factors for delirium in this study were uraemia (25.1%), hepatic encephalopathy (22.7%) and hyponatremia (19.5%). Alterations of serum electrolytes, renal function predispose to delirium15. Hyponatremia causes delirium and the mechanism is not well understood16, 17. Blood urea nitrogen/creatinine ratio greater than 18 is an independent risk factor for delirium in general medical patients9.Hepatic failure leads to hyperammonemia, which leads to excessive NMDA (N-methyl-D-aspartate) receptor activation, resulting in dysfunction of glutamate-nitric oxide-cGMP pathway and causing impaired cognitive function in hepatic encephalopathy18.Excess activation of NMDA receptors results in neuronal degeneration and death19. In hepatic failure, there may be a shift in regional cerebral blood flow and cerebral metabolic rates from cortex to subcortex resulting in delirium20.
Patients who develop delirium during their stay in hospital have higher 6-month mortality rates, longer hospital stay, increased economic burden and a higher incidence of cognitive impairment at hospital discharge21. Limitation of this study was long term follow up of patients who developed delirium was not done.
Conclusion:
Delirium is common in intensive care unit patients and hypoactive delirium is more common. Major risk factor contributing to delirium was alcohol consumption before admission. Most common precipitating factors contributing to delirium were deranged metabolic parameters.
Delirium in ICU patients especially hypoactive delirium is easily missed. Hence, all ICUs should implement both RASS and CAM-ICU for early detection of delirium. Future research needs to be directed at development of scoring systems for detection of delirium, which are easy to use and are accurate.
|
Acknowledgements Dr M Kishor, Associate Prof of Psychiatry, JSS Medical College, JSS Academy of Higher Education & Research, Mysuru, Karnataka, India. Competing Interests None declared Author Details NIKITA NAGARI, MD (Int Medicine), JSS Medical College, JSS Academy of Higher Education & Research, Mysuru, Karnataka, India. M SURESH BABU, MD (Internal Medicine), FRCP Edin, FACP, Professor of Medicine, JSS Medical College, JSS Academy of Higher Education & Research, Mysuru, Karnataka, India. CORRESPONDENCE: Dr M SURESH BABU, MD (Internal Medicine), FRCP Edin,FACP, Professor of Medicine, JSS Medical College, JSS Academy of Higher Education & Research, Mysuru, Karnataka, India. Email: drmsureshbabu@yahoo.co.in |
References
- Van Rompaey B, Elseviers MM, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, Bossaert L. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care. 2009;13(3):R77.
- Grover S, Subodh BN, Avasthi A, Chakrabarti S, Kumar S, Sharan P et al. Prevalence and clinical profile of delirium: a study from a tertiary care hospital in north India. Gen Hosp Psychiatry. 2009;31(1):25-9.
- Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology 2006 Jan;104(1):21-6.
- Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest 2007 Aug;132(2):624-36.
- Meagher D. Motor subtypes of delirium: past, present and future. Int Rev Psychiatry. 2009 Feb;21(1):59-73.
- Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007;33(1):66-73.
- McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-98.
- Pisani MA, Murphy TE, Van Ness PH, Araujo KL, Inouye SK. Characteristics associated with delirium in older patients in a medical intensive care unit. Arch Intern Med. 2007 Aug;167(15):1629-34.
- Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993 Sep;119(6):474-81.
- Morley JE. Constipation and irritable bowel syndrome in the elderly. Clin Geriatr Med. 2007 Nov;23(4):823-32.
- Rosen T, Connors S, Clark S, Halpern A, Stern ME, DeWald J et al. Assessment and management of delirium in older adults in the emergency department: Literature review to inform development of a novel clinical protocol. Adv Emerg Nurs J. 2015 Jul-Sep;37(3):183-96.
- Waardenburg IE. Delirium caused by urinary retention in elderly people: a case report and literature review on the cystocerebral syndrome. J Am Geriatr Soc. 2008 Dec;56(12):2371-2.
- Liem PH, Carter WJ. Cystocerebral syndrome: a possible explanation. Arch Intern Med. 1991 Sep;151(9):1884,1886.
- Aldemir M, Ozen S, Kara IH, Sir A, Bac B. Predisposing factors for delirium in the surgical intensive care unit. Crit Care. 2001 Oct;5(5):265-70.
- Elie M, Cole MG, Primeau FJ, Bellavance F. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998 Mar;13(3):204-12.
- Welti W. Delirium with low serum sodium. AMA Arch Neurol Psychiatry. 1956 Nov;76(5):559-64.
- Zaluska M, Janota B, Papierska L. Personality and behavioural disturbances, with delusional-hallucinatory and delirium episodes in the course of hyponatremia due to paraneoplastic inappropriate vasopressin secretion (SIADH). Psychiatr Pol. 2006 Nov-Dec;40(6):1149-60.
- Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008 Oct;24(4):789-856.
- Llansola M, Rodrigo R, Monfort P, Montoliu C, Kosenko E, Cauli O et al. NMDA receptors in hyperammonemia and hepatic encephalopathy. Metab Brain Dis. 2007 Dec;22(3-4):321-35.
- Baldy-Moulinier M, Bories P. Cerebral blood flow and metabolism in hepatic encephalopathy: effects of acute hyperammonemia and of L.dopa. Acta Neurol Scand Suppl. 1977; 64:348-9.
- Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr et al . Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004 Apr;291(14):1753-62.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




