An analysis of time and money spent on investigating painful Total Knee Replacements
AM Kassam, Professor P Dieppe and AD Toms
Cite this article as: BJMP 2012;5(3):a526
|
|
Abstract Painful Total Knee Replacements (TKR) occur in 10-20% of patients according to current literature. Considerable expense is incurred investigating and managing patients presenting with a painful TKR. We studied 41 patients with painful TKRs’ who were referred to one of the authors, a knee surgeon with a specialist interest in revision surgery. We calculated the number of appointments, investigations (serological, radiological and microbiological) along with the different managements (both surgical and medical) performed by both the originating surgeon and the specialist knee surgeon. We estimate that an average of £5136 is spent on each patient. Many of these investigations were repetitive and unnecessary. There is also a considerable difference in the cost of medical and surgical management of painful TKR patients, suggesting that early pain management would be beneficial. We conclude that early referral of patients with a painful TKR to a knee surgeon with specialist interest in revision knee surgery is beneficial and allows to reduced incurred cost to the NHS and also improved patient assessment, investigation and management. |
Introduction:
Total knee replacement (TKR) is an effective and cost-effective intervention for advanced osteoarthritis (OA). Pain is the main indication for the procedure, and the majority of patients undergoing a TKR gain significant pain relief 1-3.
However, an important minority of those who undergo a TKR have persistent pain in the operated knee 4. Baker showed that 19.8% of patients with data in the National Joint Registry had persistent knee pain, and 18.2% were dissatisfied with the procedure 5. Anderson, in a study of 98 patients, found that 8.1% claimed that the operated knee was worse at follow-up (2-3 years after surgery) than prior to surgery and 9.2% were dissatisfied Wylde et al reviewed the available literature in 2009, and found that 10-20% of patients report significant pain in the operated knee, and that the patient centred outcomes of TKR appear to be considerably worse than those of total hip replacement, where as implant survivorship figures are fairly similar 7.
There are numerous possible causes of pain after a TKR, including anterior knee pain arising from the patello-femoral joint and extensor apparatus, prosthesis loosening, or infection. Other likely causes include soft-tissue periarticular problems, referred pain, pain sensitisation, or neuropathic painBecause of the risk of infection, and the possible need for further surgery, orthopaedic surgeons are generally keen to investigate these patients thoroughly and exclude surgical causes of the problem. However, there seems to be background pain vulnerability in the knee causing this high incidence of post-operative pain. The pain itself clearly needs appropriate management but patients also need surgical evaluation to exclude important reversible causes.9
In spite of this being a sizeable and worrying problem in orthopaedics, very little has been written about the assessment or management of these patients. No protocols or guidelines are available and the costs of management have not been explored.
In this paper we describe the first case series of patients with chronic knee pain after a TKR, and document the investigations and treatment undertaken, and the direct financial costs of their care to the NHS Trust in which they were seen.
RD&E provides an Arthroplasty tertiary referral service for a large area but is a large District General Hospital and as such the costs and results we report should be representative of most trusts within the UK
Methods:
A specialist service for revision knee surgery is available at the Royal Devon and Exeter Hospital, resulting in the referral of patients with problems in a knee after a TKR. A registry of such patients has been established at the hospital. The data presented here is based on examination of the records of 41 of these patients. These were patients with a painful TKR who had been referred to one of the authors from Orthopaedic specialists in various institutions including the resident hospital.
The notes of these patients were analysed to ascertain the number of appointments patients’ had attended to address the TKR problem, and what investigations and treatments had been undertaken for that problem both by the originating surgeon and by the revision knee specialist.
In addition data was obtained from the Trust on the current costs of the clinic appointments, investigations and any treatment or interventions undertaken.
Results:
The 41 patients studied included 27 women and 14 men, with a mean age of 63.9 years (range 49-81) at time of initial TKR. In the year 2009, 536 TKR’s were performed in the trust with an average age of 70.5 years (range 37-94) with 298 females and 238 males.
Investigations were commenced for abnormal pain post total knee replacement on average 15 months (range 1-84) after their knee replacement. Appointments and investigations were undertaken over a mean time of 20 months from initial investigation (range 7-45).
Neuropathic pain was diagnosed in 6 patients and instability was identified as a cause in 5 patients. 4 patients suffered aseptic loosening and no diagnosis was made in 26 patients (63%).
Table 1 shows the average number of appointments attended and investigations undertaken on these 41 patients.
Data on the costs of these appointments, investigations and treatments to the local NHS Trust are presented in Table 2.
Table 1- Number of appointments and investigations per patient with a painful TKR
| Ave appt/pt | Range | |
| Orthopaedic appointment | 4.37 | 2 – 11 |
| Pain team appointment | 2.05 | 0 – 6 |
| Physiotherapy appointment | 3.05 | 0 – 12 |
| Hydrotherapy appointment | 0.8 | 0 – 8 |
| ESR/CRP/WCC/PV | 7.75 | 2 – 38 |
| X-rays | 7.92 | 2 – 35 |
| MRI/CT/Bone scan | 0.41 | 0 – 2 |
| Aspiration/Arthroscopies | 0.51 | 0 – 3 |
Table 2 – Costs of appointments, investigations and treatments per patient
| Ave cost/pt (£) | |
| Orthopaedic appointment | 370 |
| Pain team appointment | 235 |
| Physiotherapy appointment | 45 |
| Hydrotherapy appointment | 68 |
| ESR/CRP/WCC/PV | 21 |
| X-rays | * |
| MRI/CT/Bone scan | 70 |
| Aspiration/Arthroscopies | 1529 |
| Operative Costs | 2624 |
| Drug Costs | 174 |
| Average cost/patient | 5136 |
*= X-ray radiographs costs were insignificant and not charged to the NHS Trust
The outcomes of these 41 patients included medical management alone in 19 (14 of whom reported significant improvement) and further surgical interventions in 22 (14 of whom reported improvement). The calculated direct costs of investigation and management of those treated solely medically (i.e. non-surgically) was £190/patient, while the cost of those treated surgically was £5,051/patient. This is shown in table 3.
Table 3 – Comparison of operative versus non-operative costs
| Average Surgical intervention cost/pt | Average drug therapy cost/pt | Total cost/pt | |
| Operative patients (22) | 4891.09 | 160.22 | 5051.31 |
| Non-operative patients (19) | N/A | 190.63 | 190.63 |
Discussion:
We have analysed the management of a case series of patients with persistent pain in the knee after TKR. The results show that most of the 41 people studied attended numerous appointments with different specialists, and had the same investigations (serology and x-rays) repeated on many occasions over a relatively short period of time (less than 2 years), often before referral to a surgeon with a specific revision knee interest. We have also shown that the investigations and treatment undertaken were costly to the NHS, particularly if specialist imaging investigations (CT or MRI) or further surgical procedures (including aspiration or arthroscopy) were undertaken. The costs to the patients of the numerous appointments and repeated investigations have not been included, but are likely to have been considerable.
The fact that many different appointments were offered, and many investigations repeated, along with the wide range of different approaches to the different patients, are indicative of the absence of clear patient pathways or of a co-ordinated clinical service for these patients. Patients were seen by orthopaedic surgeons, pain specialists and physiotherapists, but definitive diagnoses or management plans did not often result from these appointments, and investigations were often repeated unnecessarily. We do not believe that this situation is unique to our area, as there are no clear guidelines or protocols to help us know how best to investigate or manage these patients before referral and the natural history of the condition is unknown.
The investigations carried out most frequently were serological tests (ESR and CRP) to try to exclude infection, and x-rays to look for prosthesis loosening or other bony problems. Previous work has shown that a single test of ESR greater than 22.5 or CRP greater than 13.5, in this situation, has a sensitivity of 0.77 and a specificity of 0.93 for the diagnosis of infection Repeating these tests offers little help, and if these were positive it would seem more appropriate to proceed to joint aspiration 11, 12-15.
Similarly, there is little point in doing more than one x-ray study a year, as the rate of change in radiographic findings is slow. If a bone problem is suspected, other more sophisticated imaging modalities can be used 16-18.
The cost data obtained from our Trust show that high costs are incurred from new clinic referrals and visits, sophisticated imaging procedures (CT, MRI and bone scans), and surgical procedures – in particular revision surgery. These high costs of investigations would indicate that patients with a painful TKR would be more appropriately investigated and managed by specialist centres with early and meticulous evaluation by surgeons with a special interest in revision knee surgery.
The surgical costs of management of painful TKR’s dwarf the amount of money spent on medical (i.e. non-surgical) approaches. This considerable difference suggests that it is of paramount importance to manage the pain early, irrespective of whether surgery is required. Good pain management will allow the surgeon, and particularly the patient, to evaluate the problem in a clearer manner, weighing up the treatment options and making a decision from a more balanced position.
According to data from the National Joint Registry, over 53,000 TKRs were performed in NHS hospitals in England and Wales in 2009 19. Using the estimates of Baker, and Wylde and others on the numbers of these patients who are in pain or dissatisfied, we calculate that over 10,000 patients each year, in this country alone, are acquiring the problem of persistent pain in a TKR ,7This represents a huge public health problem, and one that, if our Trust’s cost figures are representative, is probably costing the NHS over £10 Million/annum. In view of that, we believe that this issue needs urgent attention from the research community and health care providers.
Figure 1 – Algorithm for assessment of a patient with a painful TKR
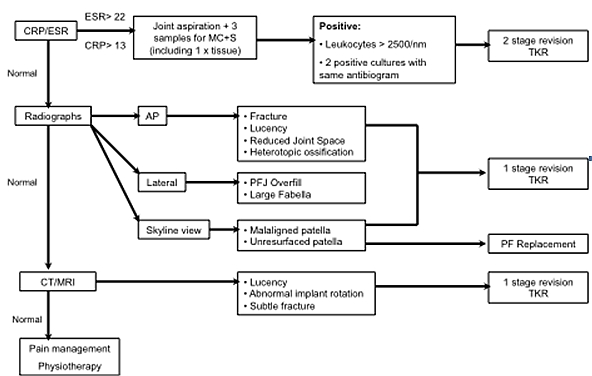
Our recommendation is that research is undertaken to document the natural history of pain in a TKR knee, differentiate the main causes of this pain, and develop simple algorithms to help clinicians make the correct diagnosis. We suggest a protocol that can be utilised by healthcare professionals to investigate painful TKR’s to allow correct assessment and diagnosis (Figure 1). We believe that health care providers in major orthopaedic centres should set up interdisciplinary clinics in which surgeons, pain specialists and physiotherapists can work together to help investigate and manage these patients.
|
Competing Interests None declared Author Details AM Kassam MRCS MBBS BSc (Hons), Department of Trauma and Orthopaedics, Royal Devon and Exeter NHS Foundation Trust, Barrack Road, Exeter, EX2 5DW. Professor P Dieppe PhD, Department of Trauma and Orthopaedics, Royal Devon and Exeter NHS Foundation Trust, Barrack Road, Exeter, EX2 5DW. AD Toms FRCS (Orth) MSc, Department of Trauma and Orthopaedics, Royal Devon and Exeter NHS Foundation Trust, Barrack Road, Exeter, EX2 5DW. CORRESPONDENCE: AM Kassam MRCS MBBS BSc (Hons), Department of Trauma and Orthopaedics, Royal Devon and Exeter NHS Foundation Trust, Barrack Road, Exeter, EX2 5DW. Email: akassam@doctors.net.uk |
References
1) Ewald FC, Wright RJ, Poss R, Thomas WH, Mason MD, Sledge CB. Kinematic total knee arthroplasty: a 10 to 14 year prospective followup review. Journal of Arthroplasty. 1999; 14:473-480
2) Losina E, Walensky RP, Kessler CL, Reischmann WM et al. Cost-effectiveness of Total Knee Arthroplasty in the United States. Archive of Internal Medicine. 2009; 169(12); 1113-1121
3) Worland RL, Johnson GV, Alemparte J, Jessup DE, Keenan J, Norambuena N. Ten to fourteen year survival and functional analysis of the AGC total knee replacement system. Knee. 2002; 9: 133-137
4) Hawker GA. Who, when and why total joint replacement surgery?: the patient’s perspective. Current Opinion in Rheumatology. 2006; 18:526-30
5) Baker PN, van der Meulen JH, Lewsey J, Gregg PJ. The role of pain and function in determining patient satisfaction after total knee replacement. Journal of Bone and Joint Surgery (Br). 2007; 89(B): 893-900
6) Anderson JG, Wixson RL, Tsai D, Stulberg SD, Change RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. Journal of Arthoplasty. 1996; 11:831-840
7) Wylde V, Blom AW, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC. Patient-reported outcomes after total hip and knee arthroplasty: comparison of midterm results. Journal of Arthroplasty. 2009; 24(2):210-216
8) Mandalia V, Eyres K, Schranz P, Toms AD. Evaluation of patients with a painful total knee replacement. Journal of Bone and Joint Surgery (British). 2008; 90B(3): 265-271
9) Toms AD, Mandalia V, Haigh R, Hopwood B. The management of patients with painful total knee replacement. Journal of Bone and Joint Surgery (British). 2009; 91B: 265-271
10) Greidanus NV, Masri BA, Garbuz DS, Wilson SD, McAlinden MG, Xu M, Duncan CP. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty: a prospective evaluation. Journal of Bone and Joint Surgery (American). 2007; 89A:1409-1416
11) Spangehl MJ, Masri BA, O’Connell JX, Duncan CP. Prospective analysis of pre-operative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. Journal of Bone and Joint Surgery (American). 1999; 81A:672-83
12) Atkins BL. Athanasou N, Deeks, JJ, Crook DW, Simpson H, Peto TE, McLardy-Smith P, Berendt AR. Prospective evaluation of criteria for microbiological diagnosis of prosthetic joint infection at revision arthroplasty: the OSIRIS Collaborative Study Group. Journal of Clinical Microbiology. 1998; 14:500-504
13) Kersey R, Benjamin J, Marson B. White blood cell counts and differential in synovial fluid of aseptically failed total knee arthroplasty. Journal of Arthroplasty. 2000; 15:301-304
14) Duff GP, Lachiewicz PF, Kelley SS. Aspiration of the knee joint before revision arthroplasty. Clinical Orthopaedics. 1996; 331:132-139
15) Hendrix RW, Anderson TM. Arthrographic and radiologic evaluation of prosthetic joints. Radiologic Clinics of North America. 1981; 19(2):349-364
16) Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement: a controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT protocol). Journal of Bone and Joint Surgery (British). 2004; 86B:818-823
17) Carpenter RD, Brilhault J, majumdar S, Ries MD. Magnetic resonance imaging of in vivo patellofemoral kinematics after total knee arthroplasty. Knee. 2009. January (online)
18) Love C, Tomas MB, Marwin SE, Pugliese PV, Palestro CJ. Role of nuclear medicine in diagnosis of infected joint replacement. Radiographics. 2001; 21:1229-1238
19) National Joint Registry, Department of Health and Welsh Assembly UK. www.njrcentre.org.uk. Accessed September 2010.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




