Anaesthetic management of a patient with Klippel-Feil syndrome for elective Caesarean section
MK Kada Venkata, Jameel Ahmed Khan, Muhammad Tayyab Qureshi, Asif Qureshi and Imtiaz Kar
Cite this article as: BJMP 2009: 2(3) 54-56
|
|
Abstract Klippel-Feil syndrome is an inherited autosomal dominant condition and is associated with various anomalies including short neck, complete fusion of the cervical spine and severe restriction of neck movements which can cause difficulty in securing the airway. The spinal deformities pose a challenge for positioning and regional anaesthesia. We present a case of a primigravida scheduled for an elective Caesarean section successfully managed with a general anaesthetic technique using awake fibreoptic technique for endotracheal intubation. |
Case report
We describe a case of a 32 year old primigravida with type III Klippel-Feil Syndrome for an elective Caesarean section. A preanaesthetic assessment at 32nd week of pregnancy revealed a history of mild asthma for which the patient was on regular salbutamol inhaler. She had no history of cardiovascular or respiratory insufficiency. There was no significant family history. Anaesthetic history included a repair of encephalomyelocele immediately after birth and a squint correction surgery at the age of 6 years under general anaesthesia which was uneventful.
Examination revealed a woman of small stature, 137 cm in height and weighing 52 kg. Airway examination revealed Mallampati III with a normal mouth opening, a reduced thyromental distance (3 cm) and inability to flex or extend the neck (Figure 1). She had thoraco-lumbar kyphoscoliosis and examination of the respiratory and cardiovascular system was unremarkable. Electrocardiogram was within normal limits as were haemoglobin, urea and electrolyte estimation. Radiography revealed fusion of atlanto-axial joint (flexion and extension views, Figure 2 ) and also fusion of lumbar vertebrae with associated scoliosis (Figure 3Cobb’s angle 25 degree) and Cobb’s angle 25 degree  Figure 1. A 32 year old parturient with Klippel-Feil syndrome with a short webbed neck and severely restricted neck movements
Figure 1. A 32 year old parturient with Klippel-Feil syndrome with a short webbed neck and severely restricted neck movements 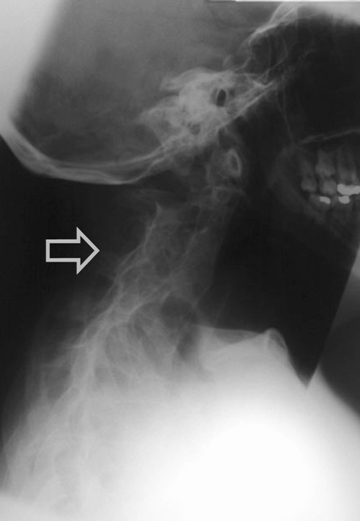 Figure 2. Radiograph of a Lateral view of cervical spine showing fusion of atlanto - occipital joint and cervical vertebrae
Figure 2. Radiograph of a Lateral view of cervical spine showing fusion of atlanto - occipital joint and cervical vertebrae 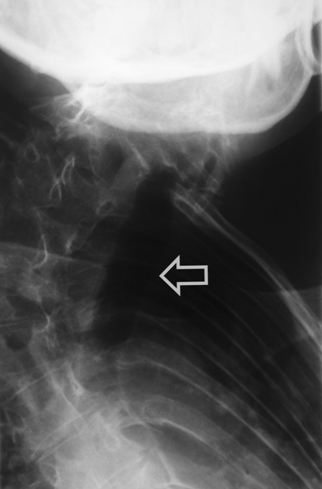 Figure 3. Antero - posterior view of dorsal spine showing deviation of trachea and marked kyphoscoliosis of thoracic spine She was scheduled to have an elective Caesarean section. The anaesthetic management options in this case included either a general anaesthetic with an anticipated difficult endotracheal intubation or a regional anaesthetic. After discussion with the patient, we planned a general anaesthetic technique with awake intubation using a fibreoptic bronchoscope (FOB) as we considered this safe. For FOB through oral route was preferred due to narrow anterior nares. Oral Ranitidine 150 mg was administered as a premedication the night before and on the morning of the planned section. After institution of standard monitoring and securing two peripheral intravenous cannulae (18G & 16 gauges), the upper airway was anaesthetised with nebulisation of 4% Lignocaine (5 ml) and 10% Lignocaine spray to the posterior pharynx. The FOB was passed through the Berman airway by using a ‘spray as you go” technique to anaesthetise the larynx and upper trachea using 4% Lignocaine and keeping well below the toxic dose (3 mg/kg). A 6.5 mm ID endotracheal tube was rail roaded over the FOB prior to its insertion and the airway was successfully secured. Once position of the endotracheal tube was confirmed, anaesthesia was then induced using intravenous Thiopentone 200 mg, Alfentanil 0.5 mg followed by Rocuronium 25 mg. Anaesthesia was maintained using oxygen with nitrous oxide (1:1 ratio) and Sevoflurane (1 MAC). Patient was ventilated with intermittent positive pressure ventilation to maintain normocapnia. The surgery lasted for 45 min and was uneventful. Using a nerve stimulator for assessing neuromuscular blockade she was reversed with Neostigmine 2.5 mg and Glycopyrrolate 0.5 mg towards the end of surgery. The patient was extubated in supine, head-low position when fully awake and in presence of protective airway reflexes. Discussion Klippel-Feil syndrome is an inherited autosomal dominant condition. In 1912, Klippel and Feil 1 first reported on a patient with a short neck, a low posterior hairline, and severe restriction of neck movements due to complete fusion of the cervical spine. These features now constitute the classic clinical triad which is the hallmark of Klippel-Feil syndrome. A great number of other anomalies associated with Klippel-Feil syndrome may pose a threat to the patient than the obvious deformity of neck. The spinal deformities may cause difficulties with both tracheal intubation and regional anaesthetic techniques. Anaesthetic management may therefore be challenging in these patients. In our case we opted for a general anaesthetic technique rather than a regional technique because of the following reasons: firstly, the patient was not keen to have regional anaesthesia, secondly, it would entail difficulty for regional anaesthesia keeping in view the spinal fusion and scoliosis and thirdly, the dose of a single bolus of spinal anaesthetic would be difficult to judge in this patient and epidural anaesthesia 2 might prove technically difficult and is associated with an increased risk of inadvertent dural puncture and poor spread within the epidural space. This patient’s abnormalities posed problems for all the commonly used anaesthetic techniques for Caesarean section. General anaesthesia could be complicated by difficult intubation. While greater use of regional anaesthesia may have reduced the number of deaths due to failed intubation in obstetric practice, several complications of epidural and spinal anaesthesia may still require intubation as part of their management. Some of these include total or high spinal anaesthesia, inadvertent intravascular injection, overdose of local anaesthetic, anaphylaxis and failure. For these reasons, the choice of regional anaesthesia for a patient with known difficult airway does not necessarily bypass the problem of unanticipated intubation. The most commonly associated anomaly in a series of 50 patients from Delaware, USA 3 was scoliosis (60% of cases), renal abnormalities (35%), Sprengel deformity (30%), deafness (30%), synkinesia (20%) and congenital heart disease (14%). The most common heart disease variant was ventricular septal defect. Less commonly associated were ptosis, lateral rectus palsy, facial nerve palsy and upper extremity anomalies. There are 3 variants of Klippel-Feil Syndrome. 4 Type I is an extensive abnormality where elements of several cervical and upper thoracic vertebrae are incorporated into a single block. In Type II variant, failure of complete segmentation occurs at one or two cervical interspaces. Type III variant includes Type I or II deformities with coexisting segmentation errors in the lower thoracic or lumbar spine. The incidence of Type II abnormalities was found to be 0.71% of Black and Caucasian skeletons that were between the ages of 17 and 102 years in a study from St Louis, Missouri, USA 5 and it is considered to be the most common form. C2-3 and C5-6 are the interspaces usually involved. It often remains unrecognised since the neck may appear normal and the patients are asymptomatic until later in life, when they present due to their increased susceptibility to cervical osteo-arthritis. Patients with Type I abnormalities are 50 times less common than Type II but are reported more frequently. This is probably because they exhibit the classic triad and thus have bizarre appearances. 6 These patients are frequently disabled by birth injuries, or have major anomalies in other organ systems. A planned elective section at term was considered as the best option for delivery of the baby by the obstetricians due to severe cephalo-pelvic disproportion and also due to anaesthetic issues regarding management. The case was managed successfully with a favourable outcome both for the mother and the baby.
Figure 3. Antero - posterior view of dorsal spine showing deviation of trachea and marked kyphoscoliosis of thoracic spine She was scheduled to have an elective Caesarean section. The anaesthetic management options in this case included either a general anaesthetic with an anticipated difficult endotracheal intubation or a regional anaesthetic. After discussion with the patient, we planned a general anaesthetic technique with awake intubation using a fibreoptic bronchoscope (FOB) as we considered this safe. For FOB through oral route was preferred due to narrow anterior nares. Oral Ranitidine 150 mg was administered as a premedication the night before and on the morning of the planned section. After institution of standard monitoring and securing two peripheral intravenous cannulae (18G & 16 gauges), the upper airway was anaesthetised with nebulisation of 4% Lignocaine (5 ml) and 10% Lignocaine spray to the posterior pharynx. The FOB was passed through the Berman airway by using a ‘spray as you go” technique to anaesthetise the larynx and upper trachea using 4% Lignocaine and keeping well below the toxic dose (3 mg/kg). A 6.5 mm ID endotracheal tube was rail roaded over the FOB prior to its insertion and the airway was successfully secured. Once position of the endotracheal tube was confirmed, anaesthesia was then induced using intravenous Thiopentone 200 mg, Alfentanil 0.5 mg followed by Rocuronium 25 mg. Anaesthesia was maintained using oxygen with nitrous oxide (1:1 ratio) and Sevoflurane (1 MAC). Patient was ventilated with intermittent positive pressure ventilation to maintain normocapnia. The surgery lasted for 45 min and was uneventful. Using a nerve stimulator for assessing neuromuscular blockade she was reversed with Neostigmine 2.5 mg and Glycopyrrolate 0.5 mg towards the end of surgery. The patient was extubated in supine, head-low position when fully awake and in presence of protective airway reflexes. Discussion Klippel-Feil syndrome is an inherited autosomal dominant condition. In 1912, Klippel and Feil 1 first reported on a patient with a short neck, a low posterior hairline, and severe restriction of neck movements due to complete fusion of the cervical spine. These features now constitute the classic clinical triad which is the hallmark of Klippel-Feil syndrome. A great number of other anomalies associated with Klippel-Feil syndrome may pose a threat to the patient than the obvious deformity of neck. The spinal deformities may cause difficulties with both tracheal intubation and regional anaesthetic techniques. Anaesthetic management may therefore be challenging in these patients. In our case we opted for a general anaesthetic technique rather than a regional technique because of the following reasons: firstly, the patient was not keen to have regional anaesthesia, secondly, it would entail difficulty for regional anaesthesia keeping in view the spinal fusion and scoliosis and thirdly, the dose of a single bolus of spinal anaesthetic would be difficult to judge in this patient and epidural anaesthesia 2 might prove technically difficult and is associated with an increased risk of inadvertent dural puncture and poor spread within the epidural space. This patient’s abnormalities posed problems for all the commonly used anaesthetic techniques for Caesarean section. General anaesthesia could be complicated by difficult intubation. While greater use of regional anaesthesia may have reduced the number of deaths due to failed intubation in obstetric practice, several complications of epidural and spinal anaesthesia may still require intubation as part of their management. Some of these include total or high spinal anaesthesia, inadvertent intravascular injection, overdose of local anaesthetic, anaphylaxis and failure. For these reasons, the choice of regional anaesthesia for a patient with known difficult airway does not necessarily bypass the problem of unanticipated intubation. The most commonly associated anomaly in a series of 50 patients from Delaware, USA 3 was scoliosis (60% of cases), renal abnormalities (35%), Sprengel deformity (30%), deafness (30%), synkinesia (20%) and congenital heart disease (14%). The most common heart disease variant was ventricular septal defect. Less commonly associated were ptosis, lateral rectus palsy, facial nerve palsy and upper extremity anomalies. There are 3 variants of Klippel-Feil Syndrome. 4 Type I is an extensive abnormality where elements of several cervical and upper thoracic vertebrae are incorporated into a single block. In Type II variant, failure of complete segmentation occurs at one or two cervical interspaces. Type III variant includes Type I or II deformities with coexisting segmentation errors in the lower thoracic or lumbar spine. The incidence of Type II abnormalities was found to be 0.71% of Black and Caucasian skeletons that were between the ages of 17 and 102 years in a study from St Louis, Missouri, USA 5 and it is considered to be the most common form. C2-3 and C5-6 are the interspaces usually involved. It often remains unrecognised since the neck may appear normal and the patients are asymptomatic until later in life, when they present due to their increased susceptibility to cervical osteo-arthritis. Patients with Type I abnormalities are 50 times less common than Type II but are reported more frequently. This is probably because they exhibit the classic triad and thus have bizarre appearances. 6 These patients are frequently disabled by birth injuries, or have major anomalies in other organ systems. A planned elective section at term was considered as the best option for delivery of the baby by the obstetricians due to severe cephalo-pelvic disproportion and also due to anaesthetic issues regarding management. The case was managed successfully with a favourable outcome both for the mother and the baby.
|
Competing Interests None declared Author Details <p>MK KADA VENKATA.MD, FRCA, FFARCSI. Consultant Anaesthetist, Ulster Hospital, Belfast, UK<br /> JAMEEL AHMED KHAN. MD, FCARCSI. Specialty Registrar Anaesthetics, Royal Victoria Hospital, Belfast, UK<br /> MUHAMMAD TAYYAB QURESHI. FFARCSI. Consultant Anaesthetist, Altnagelvin Hospital, Londonderry, UK<br /> ASIF QURESHI. MBBS. Staff Grade Anaesthetist, Altnagelvin Hospital, Londonderry, UK.<br /> IMTIAZ KAR. MBBS, MD. Staff Grade Anaesthetist, Altnagelvin Hospital, Londonderry, UK</p> CORRESPONDENCE: JAMEEL AHMED KHAN, ST-4 Anaesthetics, Royal Victoria Hospital, Belfast, UK Email: drjameel@hotmail.co.uk |
References
1. Robert NH, John EL, Dean M. Klippel-Feil Syndrome: A constellation of associated anomalies. J. Bone Joint Surg. Am 1974, 56A: 1246-53
2. Dresner MR, Maclean AR. Anaesthesia for Caesarean section in a patient with Klippel-Feil syndrome. Anaesthesia 1995, 50:807-09
3. Hensinger RN, Macewen GD. Congenital anomalies of the spine. In: Rothman RH, Simeone FA, eds. The spine. Philadelphia: W. B. Saunders, 1982: 216-33
4. Morrison SDG, Perry LW, Scott LP. Congenital brevicolis (Klippel-Feil syndrome) and cardiovascular anomalies. American Journal of Diseases of Children 1968; 115: 614-20
5. Brown MW, Templeton AW, Hodges FJ. The incidence of acquired and congenital fusions in the cervical spine. American Journal of Roentgenology, Radiotherapy and nuclear Medicine 1964; 92: 1255-9
6. Helmi C, Pruzansky S. Craniofacial and extracranial malformation in the Klippel-Feil syndrome. Cleft Palate Journal 1980; 17: 65-88

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




