Accuracy of visual estimation in diagnosing obese individuals- a blinded study
Masliyana Husin, Sazzli Kasim and Antoinette Tuthill
Cite this article as: BJMP 2012;5(2):a520
|
|
Abstract Background: Obesity is a recognised risk factor for metabolic diseases. The clinic visit allows a platform to identify patients at risk but consultation time may be limited. Visual estimation is routinely used when addressing obesity. This may lead to either an accurate or misdiagnosis of BMI, which affects management. The validity of visual scoring in engaging BMI and waist circumference is yet to be tested. Methods: Questionnaires estimating weight, height, BMI and WC were randomly distributed to doctors and patients attending different outpatient clinics. True measurements were recorded and blinded. Data was matched and analysed using SPSS. Results: In patient only analysis, 49% of patients under reported their own weight and 68% under reported their waist circumference. In physician group analysis, we found that in patients who are obese, 81% were estimated as obese by doctors. In patients who are overweight, 63% were estimated as overweight, and 25.7% as normal. In the normal weight group, 69.5% were estimated as normal. Overall, 72% of BMI was estimated correctly by doctors. There is no accuracy difference in doctor's and patient's weight estimation. Patients are not aware of the effect of abdominal obesity to health with poor insight. Conclusions: Visual estimation would miss accurate diagnosis in overweight individuals and should not replace true anthropometric measurements. Keywords: Obesity, BMI, waist circumference, diagnosis, visual estimation |
Introduction:
There are approximately over 1.6 billion overweight people with a body mass index (BMI) greater than 25 kg/mAnnually, around 2.8 million deaths are attributed to overweight and obesity worldwide(1). Many overweight individuals underestimate their weight and despite acknowledging their overweightness, many are not motivated to losing weight(2).Accurate measurement is important as it identifies patients with diagnoses which subsequently impact on their management. Self-reported weight is often used as a means of surveillance but has been shown to bias towards under reporting of body weight and BMI as well as over reporting on height(3). Several estimation techniques has been devised to quantify anthropomorphic measurements when actual measurement cannot take place(4),(5),(6), however, these methods are associated with significant errors for hospitalised patients(7). There is no published study that questions the validity of visual estimation of obesity in daily clinical setting despite its relevance to the daily practice. We aim to investigate the accuracy of visual estimation compared to actual clinical measurements in the diagnosis of overweight and obesity.
Methods:
This is a case control study. Patients for this study were attending the endocrinology, cardiology and chest pain out-patient clinic in Cork University Hospital, Cork, Ireland. The questionnaire session was carried out at every endocrinology, cardiology and chest pain clinic for 5 consecutive weeks. A total of 100 patients were recruited allowing for a 10% margin of error at 95% confidence level in a sample population of 150 000. Ten doctors of varying grades were chosen randomly to visually score the subjects. Exclusion criteria included patients who were pregnant and who are wheelchair bound. Consent was obtained from patients prior to filling questionnaires. Ethical approval was received from the Clinical Research Ethics Committee of the Cork Teaching Hospitals.
In the waiting room, patients were asked to self- report their weight, height and waist circumference to the best of their estimate. Demographics and cardiovascular risk were obtained from medical charts and presented in Table 1. The questionnaires have a section that specifically tests patients’ awareness of abdominal obesity and patients were asked to choose between obesity and abdominal obesity, relying on their own knowledge of markers of cardiovascular risks. Clinical measurements were taken in the nurses’ assessment room. Weight was measured by using portable SECA scales (Seca 755 Mechanical Column Scale) and was measured to the nearest 0.1kilogram. All patients were measured on the same weighing scale to minimize instrumental bias. Patients were asked to remove their heavy outer garments and shoes and empty their pockets and to stand in the centre of the platform, so that weight is distributed evenly to both feet.
Height was measured by using a height rule attached to a fixed measuring rod (Seca 220 Telescopic Measuring Rod). Patients were asked to remove their shoes and are asked to stand with their back to the height rule. It was ensured that the back of the head, back, buttocks, calves and heels are touching the wall. Patients were asked to remain upright with their feet together. The top of the external auditory meatus is leveled with the inferior margin of the bony orbit. The patients were asked to look straight. Height is recorded to the resolution of the height rule (i.e. nearest millimeter).
Waist circumferences were measured using a myotape. Patients were asked to remove their outer garments and stand with their feet close together. The tape is placed horizontally at a level midway between the lower rib margin and iliac crest around the body. They were then asked to breathe normally and the reading of the measurement was taken at the end of gentle exhaling. This prevents patients from holding their breath. The measuring tape is held firmly, ensuring its horizontal position and loose enough that it allows placement of one finger between the tape and the subject's body. A single operator who has been trained to measure waist circumference as per the WHO guidelines is used repeatedly in order to reduce measurement bias(8).
The doctors were asked to visually estimate the patients' weight, height, waist circumference and BMI. The estimation is recorded on a separate sheet. All doctors were blinded to the actual clinical measurements. The questionnaires were then collected at the end of the clinic and matched to individual patients. Data entry was performed in Microsoft Excel and exported for statistical analysis on SPSS version 16.
Findings
The study enrolled 100 patients. Demographic and cardiovascular risk details are shown in Table 1. Among these, 42 were obese, 35 were overweight and 23 patients had a normal BMI. The sample has a mean BMI of 29.9kg/m2 (95% CI 28.7-31.1) with a mean waist circumference (WC) of 103.2cm (95% CI 100.7-107.2). The average male waist circumference is 105.8 cm while the average female waist circumference is 101.6cm. The mean measured weight was 84.6kg (95% CI 81.0-88.2) and the mean height measurement was 1.68m (95% CI 1.66-1.70).
Table 1: Cardiovascular risk factors
| Sex | Male(n=55) | Female(n=45) |
| Mean age | 53.6(19-84) | 56.7(23-84) |
| Diabetes | 17 | 14 |
| Hypertension | 16 | 20 |
| Hypercholesterolaemia | 24 | 19 |
| Active smoker | 10 | 5 |
| Ex- smoker (>10years) | 8 | 3 |
| Previous stroke or heart attack | 6 | 6 |
| Previous PCI | 6 | 3 |
Patient’s perception and doctor’s estimation of anthropomorphic measurements were compared to actual measurements and is displayed in Table 2.
Table 2. Deviation from actual measurement values in both groups
| Patient’s Estimation | Mean estimated | Mean deviation (estimated – actual measurements) | 95% Confidence interval of Mean Deviation |
| Weight | 81.16 | -3.71 | -5.10 to -2.32 |
| Height | 1.6782 | 0.0039 | -0.0112 to 0.0033 |
| Waist | 90.85 | -13.09 | -15.48 to -10.70 |
| BMI | 28.68 | -1.24 | -1.87 to -0.61 |
| Doctor’s visual estimation | |||
| Weight | 80.85 | -3.78 | -5.54 to -2.02 |
| Height | 1.6710 | -0.0113 | -0.224 to 0.002 |
| Waist | 92.10 | -11.84 | -13.87 to -9.81 |
| BMI | 29.08 | -8.47 | -1.54 to -0.15 |
In terms of patients own estimation of height, weight and waist circumference, 49% of patients under estimated their weight by up to 1.5kg, 35% reported accurately to 1.5 kg and 16% over reported weight. 67% of patients estimated height accurately, 18% of patients under-estimated, and 15% over-estimated. When asked to estimate their waist circumference, 68% of patients under estimated by up to 5cm, 30% over estimated and 2 patients estimated accurately to 5cm (Figure 1). We found that 70% of patients regarded obesity as the higher threat to health compared to abdominal obesity. There were no differences in patient’s self reported weight and doctor’s weight estimation (p= 0.236).
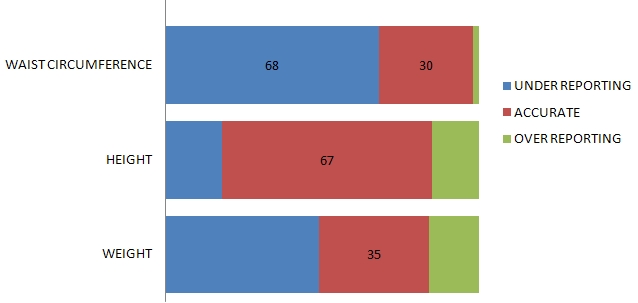
Figure 1. Graphical representation of patients estimated weight, height and waist circumference
We then analysed the doctor’s estimation of height, weight, waist circumference and BMI. For the purpose of interpreting the data on BMI, the estimates that is recorded by doctors that matches the patient’s real BMI by clinical measurement is considered accurate. Therefore, for patients who have a normal BMI, 69.5% were correctly estimated as normal and the rest (30.5%) were estimated as overweight. For those patients who are obese, 81% were estimated as obese and by the doctors as a group and the rest (19%) is estimated to be overweight. In patients who are overweight, 63% were correctly estimated as being overweight by doctors, 9% were estimated as being obese and the rest (28%) were mistakenly estimated as having a normal BMI. Accurate BMI estimation by doctors was achieved in 72% patients (Figure 2).
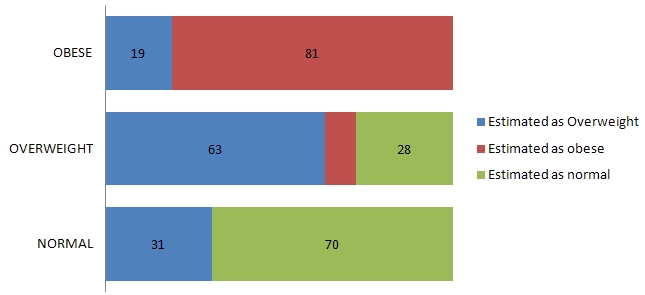
Figure 2. Doctors estimation of BMI compared to actual clinical measurement
Doctors were noted to underestimate the patients’ weight in 53 patients, over estimated in 26, while being accurate in their estimation in 21 patients. Estimation of waist circumference to the nearest 5 cm shows marked under estimation of waist circumference in 71% of patients, over reporting in 3% of patients and 26% accurate estimation. The majority of underestimation of waist circumference happens in the region of 10 to 15cm. For patients who are obese, doctors were able to estimate waist circumference correctly in 58% of obese individuals.
Discussion:
This is the first study demonstrating the relationship of visual estimation of a cardiovascular risk factor and comparing to actual clinical measurements. As obesity and abdominal obesity becomes an increasingly common phenomenon, our perception of the 'normal' body habitus may be distorted(9).
It is observed that in the bigger hospitals out-patient departments, physicians and nurses are commonly affected by clinical workload and tend to spend a limited amount of time with patients in order to achieve a quicker turnaround time. Cleator et al looked at whether clinically significant obesity is well detected in three different outpatient department and whether they are managed appropriately once diagnosed(10). In all the outpatient departments involving the specialties of rheumatology, cardiology and orthopedics, the actual cases of clinical obesity is higher than what is being diagnosed and the management of obesity was heterogeneous and minimal in terms of intervention. With the ever increasing obese patients attending hospitals, it is understandable that healthcare providers such as physicians, nurses, dietician and physiotherapist resort to relying on visual estimation.
In terms of patient’s own estimation of height, weight and waist circumference, we gained that patients were reasonably good at estimating their own height but tend to under estimate weight. This is probably due to the fact that these patients have not had a recent measurement of weight and their weight estimation is based on previous historical measurement from months to years back, which in the majority of people, is less than their current weight. This also explains why their height estimation is more accurate, as adult heights do not undergo significant changes and are relatively constant.
When attempting to obtain patient’s own estimation of waist circumference, we found that most patients are not at all aware of the method used to measure waist circumference. Some patients even mistaken waist circumference as being their trousers’ waist size. In those who were able to give estimation, a large proportion would under estimate.
The majority of patients think that general obesity is more predictive of cardiovascular outcome compared to abdominal obesity. This lack of awareness is reflective on clinician’s effort in addressing abdominal obesity as an important cardiovascular risk factor to patients during consultations. The lack of proper awareness campaign by healthcare providers along with the evolving markers of cardiovascular risk may further confuse the general public.
Recently, waist circumference, waist to hip ratio along with many serum biomarkers have been noted to correlate to adverse outcomes in obese individuals, independent of BMI. Waist circumference measurement is a relatively new tool compared to the measurement of BMI. This would explain the discrepancy between doctors’ estimation of BMI and waist circumference. Visual estimation is further compromise as many patients would be covered in items of clothing during consultations. In order to obtain a better estimation of waist circumference, the individual have to be observed from many angles, a task that may be impossible in a busy clinic.
Although BMI is a convenient method to quantify obesity, recent studies have shown that waist circumference is a stronger predictor of cardiovascular outcomes(11),(12),(13),(14).The importance of waist circumference in predicting health risk is thought to be due to the relationship between waist circumference and intra-abdominal fat(15),(16),(17),(18),(19),(20).We now know that the presence of intra-abdominal visceral fat is associated with a poorer outcome in that patients are prone to develop metabolic syndrome and insulin resistance(21).We have yet to devise a more accurate measurement on visceral fat and at present limited to using waist circumference measurements.
Although doctors are generally good at BMI estimation, we found that in estimating overweight patients’ BMI, close to 30% were wrongly estimated as having normal BMI. Next to the obese, these groups of patients are likely to have metabolic abnormalities and increased cardiovascular risk. If actual measurement of BMI is not routinely done, we may neglect patients who would benefit from intervention. A simple, short counseling during the outpatient visit with emphasis on weight loss, the need to increase their daily activity levels and the morbidity related to being overweight may be all that is needed to improve the population health in general. Further intervention may include referrals to hospital or community dieticians and prescribed exercise programmes. These intervention tools already exist in the healthcare system and could be accessed readily.
The nature of our study design exposes it to several potential selection and measurement biases. Future studies should include patients of differing ages and socioeconomic background. Additionally, clinicians of differing appointments from various different specialties should be included to obtain a more applicable result. A measure of diagnostic efficacy should also be employed to further assess the value of clinical measurement and therapeutic intervention.
Conclusion:
The appropriateness of visual scoring of markers of obesity by doctors is flawed and limited to the obese individuals. True anthropometric measurements would avoid misdiagnosing overweight individuals as normals. We can conclude that patients’ own estimation of weight is unreliable and that they are unaware of the impact of high abdominal fat deposition on cardiovascular outcome. The latter should be addressed in consultations by both hospital physicians and general practitioners. Further emphasis and education in schools and awareness campaigns should also advocate this emerging cardiovascular risk factor.
|
Acknowledgements We would like to thank the nursing staff in the respective clinics for providing valuable time and assistance in performing this study. Competing Interests None declared Author Details Masliyana Husin MBBCh, Cork University Hospital, Ireland. Sazzli Kasim MRCPI, Cork University Hospital, Ireland and UiTM SgBuloh Malaysia. Antoinette Tuthill, MD, Department of Endocrinology, Cork University Hospital, Ireland. CORRESPONDENCE: Sazzli Kasim MRCPI, Department of Cardiology, Cork Universiy Hospital, Ireland. Email: sazzlikasim@gmail.com |
References
1.World Health Organization http://www.who.int/mediacentre/factsheets/fs311/en/index.html accessed on 21st August 2011.
2. Wardle J, Johnson F. Weight and dieting: Examining level of weight concern in British adults. Int J Obesity 2002; 26(8):1144-1149.
3. Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self –report measures for assessing height, weight and body mass index: a systematic review. Obes Rev 2007; 8:307-26.
4. Crandall CS, Gardner S, Braude DA. Estimation of total body weight in obese patients. Air Med J 2009; 28:139-45.
5. Lorenz MW, Graf M, HenkeC, Hermans M, Ziemann U et al. Anthropomorphic approximation of body weight in unresponsive stroke patients. J Neurol Neurosurg Psychiatry 2007; 78:1331-6.
6. Todorovic V, Russell C, Stratton R, Ward J, Elia M. The ‘MUST’ Explanatory Booklet. Redditch: British Association for parenteral and enteral nutrition, 2003.
7. Darnis S, Fareau N, Corallo C, Poole S, Dooley M, Cheng AC. Estimation of body weight in hospitalized patients. QJM 2012 Apr 4 (doi:10.1093/qjmed/hcs060) Epub ahead of print.
8. Report of a WHO Expert Consultation: Waist Circumference and Waist-Hip ratio. Geneva 8-11 December 2008.
9. Johnson F, Croker H, Wardle J. Changing perceptions of weight in Great Britain: comparison of two population surveys. BMJ 2008; 337:a494.
10. Cleator J, Richman E, Leong KS, White S, Wilding J. Obesity: under-diagnosed and under-treated in hospital outpatient departments. Int J Obes Relat Metab Disord. 2002; 26(4):581-4.
11. Janssen I, Katzmarzyk PT and Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med 2002; 162: 2074-9.
12. Karter AJ, D'Agostino RB, Jr., Mayer-Davis EJ. Abdominal obesity predicts declining insulin sensitivity in non-obese normoglycaemics: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Obes Metab 2005; 7: 230-8.
13. Janssen I, Katzmarzyk PT and Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 2004; 79: 379- 84.
14. Ardern CI, Katzmarzyk PT, Janssen I. Discrimination of health risk by combined body mass index and waist circumference. Obes Res 2003; 11: 135-42.
15. Janssen I, Heymsfield SB, Allison DB. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous and visceral fat. Am J Clin Nutr 2002; 75: 683- 8.
16. Després JP, Prud'homme D, Pouliot MC. Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men. Am J Clin Nutr 1991; 54: 471-7.
17. Han TS, McNeill G, Seidell JC. Predicting intra-abdominal fatness from anthropometric measures: the influence of stature. Int J Obes Relat Metab Disord 1997; 21: 587-93.
18. Ross R, Shaw KD, Rissanen J. Sex differences in lean and adipose tissue distribution by magnetic resonance imaging: anthropometric relationships. Am J Clin Nutr 1994; 59: 1277-85.
19. Ross R, Leger L, Morris D. Quantification of adipose tissue by MRI: relationship with anthropometric variables. J Appl Physiol 1992; 72: 787-95.
20. Seidell JC, Bjorntorp P, Sjostrom L. Regional distribution of muscle and fat mass in men--new insight into the risk of abdominal obesity using computed tomography. Int J Obes 1989; 13: 289-303.
21. Canoy D. Distribution of body fat and risk of coronary heart disease in men and women. Curr Opin Cardiol. 2008 Nov; 23(6):591-8.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




