General Medical Practitioners’ knowledge of assessment and management of Temporomandibular Joint disorders: a questionnaire -based survey in the UK
Siddiq Ahmed, Muhammad Ali, Faisal Rehan, Anil Israni & Christopher Avery
Cite this article as: BJMP 2019;12(2):a015
|
|
Abstract Background: The management of temporomandibular joint disorders (TMDs) is a challenge for General Medical Practitioners (GMPs). They are increasingly approached by patients for advice on TMD but little is known about how this disorder is dealt with in primary health care. Abbreviations: GMPs: General Medical Practitioners, GDPs: General Dental Practitioners, TMD: Temporomandibular joint disorders, RDC/TMD: Research Diagnostic Criteria for Temporomandibular Disorders |
Introduction:
Temporomandibular joint disorder (TMD) refers to a broad spectrum of disease states characterised mainly by pain and tenderness in the temporomandibular joint (TMJ) and adjacent soft tissues, TMJ clicking and limitation in jaw movements. TMD symptoms vary in severity and if left untreated, may lead to debilitating pain and limited function with a significant impact on quality of life. The estimated prevalence of TMD is 2-6 % 1 although up to 25 % has also been reported. The aetiology of TMD is not fully understood and it is multifactorial including organic disease of the TMJ, trauma, malocclusion and stress. Treatment options include reassurance and education, physical and splint therapy, simple analgesia and other drugs, surgical intervention or combined treatment. Most cases of TMD can be managed non-surgically. Most patients with TMD have traditionally been initially managed by a GDP and are often referred to a specialist for further non-surgical or surgical therapies if symptoms are not controlled.
Andersen et al (1999) reported approximately 3 out of every 100 attendances to GMP services in Wales, UK were due to oral and dental problems 2. The number of people attending their GMP for dental problems has been increasing 3, 4. GMPs have expressed concerns about their ability to treat dental diseases 5 as these conditions are beyond the scope of their expertise.
Consulting GMPs for TMD has been observed dating back to over nearly six centuries 6. Similar to the rising trend of attending GMP for oral problems in general, there has been an increasing tendency for patients with TMD symptoms to approach their GMP as the first point of contact due to comparatively easier availability and financial feasibility. Prompt referral to a GDP or relevant speciality is likely to improve management and reduce the adverse impact on quality of life. This could potentially reduce the burden on overstretched NHS hospitals in UK. There is paucity of data on the management of TMD among GMPs in UK. To the best of our knowledge, there has been no prior survey of their knowledge of and attitude towards assessment and management of TMD. The objectives of this study are to assess the current experience of UK GMPs with the care of TMD patients in primary care.
Method:
Design
A Single-Centre Cross-sectional survey
Study population and survey development
GMPs listed within the Leicester City Clinical commissioning groups 7 with access to refer to the regional NHS Oral and Maxillofacial Services Providers. GMPs were formally invited to complete a specifically prepared postal questionnaire (See Appendix) consisting of their knowledge and management of TMD. In order to ensure the reliability and validity of the results of survey, the questionnaire was pretested on the GMPs in five different Urban GP surgeries other than Leicester city. To maximise response rates, a follow-up questionnaire and telephone calls were arranged after four weeks if no reply had been received. Confidentiality was maintained by number-coding the questionnaires. Selection bias was avoided by sending the questionnaire to all the GMPs in the Leicester city area.
The questionnaire Survey was conducted in February 2018 and comprised of 16 questions on TMD and two demographic questions .The questionnaire assessed knowledge of TMD including clinical features, diagnostic criteria, prevalence and aetiology. Participants were asked about awareness of current guidelines and treatment options, and their management practice, whether they would refer to a GDP, or oral and maxillofacial surgeon or TMD specialist. They were asked whether they update or have updated their knowledge about TMD. They were also invited to propose which means of TMD knowledge provision they would prefer to receive demographic data included information on the gender and clinical experience. There were no open-ended questions and participants were asked to select the most correct statement from more than one option in some of the questions. Participant GMPs were informed in the invitation letter that participation was voluntary, all responses were anonymous and that the study would be published in a peer-reviewed journal. Participation in the survey implied consent.
Data analysis
Data was analysed descriptively using IBM SPSS Statistics for Windows version 21 (IBM Corp, Armonk, USA). We aimed to determine whether there is any relationship between GMPs knowledge of diagnostic features of TMD and their length of experience in practice. We stratified GMPs into two groups according to the seniority [certificate of completion of specialist training (CCST) obtained within 5 years or earlier]. Chi square test was used to compare the proportion between two groups and a p value < 0.05 was considered to be statistically significant.
Results:
Out of 259 GMPs who were contacted and invited to participate, a total of 126 practitioners returned the questionnaire by post {response rate (48.6%)}. Of the respondents, 2 did not correctly fill the survey questionnaire; the remaining 124 responses were analysed. There was a slight male preponderance (55%). Only 12% GMPs rated themselves above average (score >4) in terms of being familiar in general with TMD. Five percent of responders were aware of published guidelines of TMD management. None of them were familiar of Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). Seventy-four percent of participants, including both GMPs with experience less than 5 years and more described the clinical features consistent with the diagnosis of TMD. 4% selected the correct option when asked about the possible causative factors. None of them knew about the actual prevalence of TMD symptoms in the community and majority of GMPs underestimated the proportion of population with TMD. Fourteen percent were correct in identifying the age group affected by TMD. While majority of them (56%) chose ‘ No’ and 12 % of them selected ‘Don’t know’ , thirty-two percent, participants believed that subjects with TMD symptoms require initial radiographic assessment before any treatment is commenced. 95% of respondents believed that they have seen on average 2 to 4 TMD patients per month. Eighty nine percent of respondents referred patients to GDPs whereas remaining 11 % of GMPs contacted Oral and maxillofacial surgery service providers for TMD management (see Figure). Only one of the participants was familiar of specialist-clinical services for TMD who, in addition to sending these patients to GDPs, also referred TMD patients directly to specialists. Majority of them (66%) were not comfortable in seeing and provide initial management of TMD and 34% of GMPs, in addition to referring TMD patients to other services, also provided initial treatment to these patients. All those who offered this initial non-surgical treatment to manage TMD, selected combined modalities i.e. patient education, pharmacological and physical therapy. In every 25 participants (6%) has updated their knowledge through internet resources in order to increase their awareness and knowledge about the TMD management in community. Almost all (97%) of the GMPs would welcome relevant continued education programmes and receiving leaflets / published literature. The summary of GMPs responses from survey is given in Table 1. Group analysis of participants (See Table 2) did not show any statistical association between the experience of GMPs and their knowledge of TMD clinical features (Chi-square statistics 3.78, p = 0.5).
Figure: GMPs Referral for TMD patients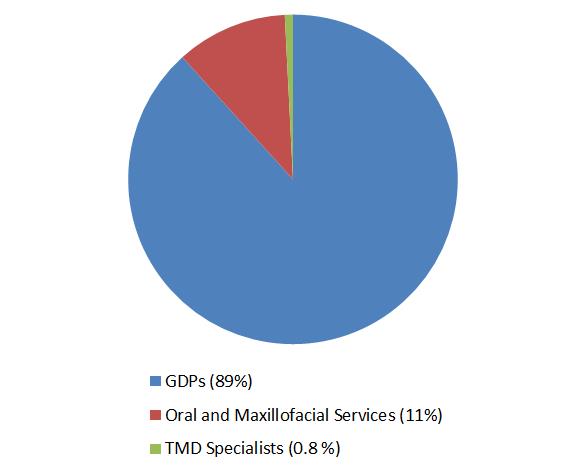
GMPs: General Medical practitioners, TMD: Temporomandibular joint disorders, GDPs: General Dental Practitioners
Table 1: Summary of the main responses from the GMPs survey about TMD knowledge
| Familiarity of TMD rated as above average | 12% |
| Awareness about TMD guidelines | 5% |
| Familiarity with RDC Criteria of TMD | 0% |
| Correctly identified the etiological factors of TMD | 4% |
| Correctly identified TMD clinical features | 74% |
| Correctly identified the TMD prevalence in General population | 0% |
| Correctly identified the age group suffered most with TMD | 14% |
| Selected ‘No’ about the need of radiograph before TMD management is initiated | 56% |
| Not comfortable in seeing and provide initial management of TMD | 66% |
| Selected combination of pharmacological and physiotherapy to treat TMD | 34% |
| Have referred TMD patients to GDPs | 89% |
| Have referred TMD patients to Oral and maxillofacial surgery | 11% |
| Have updated the TMD knowledge through any resource | 6% |
| Keen to receive further information about TMD | 97% |
GMPs: General Medical practitioners, TMD: Temporomandibular joint disorders
Table 2: Distribution of participant GMPs according to their seniority and familiarity with TMD clinical features
| Experience as GMP | Correctly identified TMD features (n) |
Incorrectly identified TMD features (n) |
| Greater than 5 years | 50 | 11 |
| Less than 5 years | 42 | 21 |
Chi-square statistics 3.7894 p = 0.5
GMPs: General Medical Practitioners, TMD: Temporomandibular joint disorders
Discussion:
Main Findings
Our study is the first which has explored in-depth the experience of GMP with TMD management. Findings from the survey indicate that uncertainty exists among GMPs regarding their level of knowledge. Most GMPs had no awareness of TMD management guidelines. The RDC/TMD 8 is a valuable tool to assess signs and symptoms and to classify patients with TMDs. Participants were not aware of these guidelines. The response from GMPs indicated that the prevalence of TMD within the general population is not accurately recognised at all along. The majority of respondents do not appreciate that TMD patients require radiographic evaluation before treatment planning. None but one of the GMPs was aware of clinicians with a subspecialty in TMD. All patients with such condition were referred either to dentists or maxillofacial surgeons. This reflects an awareness of an appropriate chain of referral 9. There was a generalised consensus in considering the general medical practice environment as an unsuitable place to manage dental problems 5, including TMD. A positive finding of our study was that a significant proportion of GMPs in Leicester city are interested in learning about TMD. This indicates there is a need for designing formal training courses for GMPs. If appropriately trained, these practitioners will potentially have an enhanced capability of not only managing TMD at an initial level but also providing knowledge and guidance to other practices and community services
Comparison with existing literature
The knowledge, attitude and practices of GDPs regarding TMD management are widely reported 10-12 but there is hardly any study relating to General Medical Practice. Results of a questionnaire survey based on screening of TMD in 38 London teaching General Medical Practices were similar to our findings 13. .Thirty-six of 38 GMPs, who replied in that survey, routinely assess the TMJ as part of the physical examination for symptoms of TMD whereas TMJ assessment was not included in primary health care screening. Similarly to Cope et al 2015 5 another qualitative study in the North-west of England GMPs experiences of chronic orofacial pain, including TMD, revealed primary health care providers consider themselves unable to meet the diagnostic and management challenges of TMD 14 .GMPs in the face to face interviews explained that despite these limitations, they do offer TMD patients pharmacological and other complimentary approaches, particularly acupuncture. Similar experiences of GMPs are also reflected in our current findings.
Strength and limitations
The main strength of this survey is that, to the best of the authors' knowledge, it was the first study which determined Knowledge and experience of GMPs towards Management of TMD. In simple language but a comprehensive and pilot tested questionnaire was designed to assess GMPs knowledge of TMD which they were expected to have gained from available literature.
There were mainly two limitations in our survey. Firstly, the sample size was small as the study was confined only to the participant GMPs practising in Leicester City, hence it may not be representative of all GMPs across the country. Despite this weakness the results may serve as a scoping study to justify further research such as qualitative surveys. Secondly, there was a relatively low but acceptable response rate (48.6%). Although this raises concerns about the research validity, but studies have demonstrated that there is no direct correlation between response rate and validity 15. Also, Surveys with comparatively low response are only marginally less accurate than those with much higher reported response rates 16.
Implications for research and practice
In addition to other main areas of practice, the Royal College of General Practitioners (RCGP) curriculum also highlights the importance of Specialist GMP trainees attaining competency in learning about common oral and maxillofacial conditions 17. Considering the frequent attendance of patients with oral and facial diseases in primary care and the limited undergraduate Medical training, valuable suggestions have been made for GMPs to promote attendance at specialist oral medicine and oral surgery clinics to enhance exposure to common maxillofacial diseases. Despite these recommendations, surprisingly little no active interest has yet been shown by GMPs trainees. There is a need to integrate GMP training with some exposure to the specialty of Oral and Maxillofacial surgery to improve expertise in the management of TMD and other oral diseases, especially in view of the increasing trend for patients to initially present to their GMP for advice about TMD and other chronic orofacial pain conditions. .
Evidence based literature regarding dealing with TMD at a non-specialist level have been published in the medical literature 18-20. This provides clinicians including GMPs with sufficient knowledge to diagnose and refer TMD to the relevant clinician. The British association of Oral and Maxillofacial Surgeons (BAOMS) TMD commissioning guide 2014 8 suggests GMPs to refer TMD patients to a GDP in the first instance to start initial treatment. Early diagnosis, counselling and management of TMD tend to improve prognosis and reduces the severity of impact on the quality of life 21, 22. It is crucial that GMPs are have sufficient knowledge to make an early referral to an appropriate clinician in order to commence conservative measures including education and advice, use of a bite guard, medications and self-directed physical therapy. The limited access to dental care within the UK, despite a National Health Service (NHS), is a well-recognised challenge. There are multiple barriers to accessing dental care 23 including delays or failure in getting appointments which results in the patient turning to General Medical Practice for advice 4. GMPs have also expressed concerns regarding accessibility to and the collegiate relationship with GDPs in the management of chronic facial pain including TMD 14. Whether the aforementioned limitations are system related or simply patient factors, they are certainly hindrances to timely assessment and intervention. We suggest that suitably trained GMPs should be able to commence the initial conservative management of TMD patients whilst simultaneously referring patients to a GDP or appropriate specialist so as to optimize the management and possibly reduce subsequent referrals in the long term. There is an immense potential for primary care to be integral part of initial management of TMD. A large scale nationwide study could potentially help future planning for care within the community.
Conclusion:
Respondent GMPs in East midlands England, demonstrated limited knowledge and confidence related to the diagnosis and management of TMD. Appropriate post-graduate training and educational opportunities for ongoing continuing professional development related activities would improve the knowledge and awareness of TMD management, potentially leading to more effective care within the community.
|
Acknowledgements The authors thank Mr. Muhammad Azam Baqa for his technical assistance. We are also grateful to all GMPs who participated in this survey. Competing Interests None declared Author Details Siddiq Ahmed, BDS, FFDRCSI, Oral and Maxillofacial Surgery Department, Wythenshawe Hospital, UK. CORRESPONDENCE: siddiqahmed76@yahoo.co.uk Email: siddiqahmed76@yahoo.co.uk |
References
- List T, Wahlund K, Wenneberg B et al. TMD in children and adolescents: prevalence of pain, gender differences, and perceived treatment need.J Orofac Pain. 1999 Winter;13(1):9-20.
- Anderson R, Richmond S, Thomas DW.Patient presentation at medical practices with dental problems: an analysis of the 1996 General Practice Morbidity Database for Wales. Br Dent J. 1999 Mar 27;186(6):297-300.
- Bint A. NHS dentistry: general practitioners are doing dentists’ work. BMJ 2008;336:1088
- Cope AL, Wood F, Francis NA et al. Patients’ reasons for consulting a GP when experiencing a dental problem: a qualitative study.Br J Gen Pract 2018; 68 (677): e877-e883. DOI: https://doi.org/10.3399/bjgp18X699749
- Cope AL, Wood F, Francis NA et al. General practitioners' attitudes towards the management of dental conditions and use of antibiotics in these consultations: a qualitative study.BMJ Open. 2015 Oct 1;5(10):e008551. doi: 10.1136/bmjopen-2015-008551.
- Norman A. Sprott.Minor Derangement of the Temporo-mandibular Joint. Br Med J. 1957 Dec 7; 2(5057): 1371.
- NHS Leicester City Clinical Commissioning Group. Finding GP services https://www.leicestercityccg.nhs.uk . Accessed January 10, 2018.
- Dworkin SF & LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. Journal of Craniomandibular Disorders. 6(4):301-55, 1992
- British Association Of Oral and Maxillofacial Surgeons (BAOMS) Commissioning guide: Temporomandibular joint disorders 2014. Royal college of surgeons. https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/tmj-commissioning-guide/. Accessed November 15, 2018
- Tegelberg A, Wenneberg B, List T. General practice dentists' knowledge of temporomandibular disorders in children and adolescents. Eur J Dent Educ. 2007 Nov;11(4):216-21.
- Baharvand M, Sedaghat Monfared M, et al. Temporomandibular Disorders: Knowledge, Attitude and Practice among Dentists in Tehran, Iran. J Dent Res Dent Clin Dent Prospects. 2010;4(3):90–94. doi:10.5681/joddd.2010.023
- Gnauck M, Magnusson T, Ekberg E. Knowledge and competence in temporomandibular disorders among Swedish general dental practitioners and dental hygienists. Acta Odontol Scand. 2017 Aug;75(6):429-436. doi: 10.1080/00016357.2017.1331373. Epub 2017 May 29.
- St John Crean A, Pilcher R, Isenberg DA. Health screening: the temporomandibular joint. Ann Rheum Dis. 1993;52(9):696.
- Peters S, Goldthorpe J, McElroy C et al. Managing chronic orofacial pain: A qualitative study of patients', doctors', and dentists' experiences. Br J Health Psychol. 2015 Nov;20(4):777-91.
- Holbrook A, Krosnick J, Pfent A. The causes and consequences of response rates in surveys by the news media and government contractor survey research firms.In: Lepkowski JM, Tucker NC, Brick JM, De Leeuw ED, Japec L, Lavrakas PJ, et al, editors. Advances in Telephone Survey Methodology. New York (NY):Wiley; 2007.
- Mealing NM, Banks E, Jorm LR et al. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med Res Methodol. 2010;10:26.
- Royal College of General Practitioners. GP curriculum: overview https://www.rcgp.org.uk/training-exams/training/gp-curriculum-overview/document-version.aspx. Accessed April 10, 2019.
- George Dimitroulis. Temporomandibular disorders: a clinical update BMJ 1998;317:190-4
- Durham J, Newton-John TR, Zakrzewska JM.Temporomandibular disorders..BMJ 2015;350:h1154.
- McNeal S,Temporomandibular joint syndrome. BMJ Best practice , June 2018
- Durham J, Steele J G ,Wassell R W et al. Living with uncertainty: temporomandibular disorders. JDentRes 2010;89:827-30.
- Durham J, Breckons M, Araujo-Soares V et al. Developing Effective and Efficient care pathways in chronic Pain :DEEP study protocol.BMC Oral Health 2014;14:6.
- Freeman R. Barriers to accessing dental care: patient factor. British Dental Journal volume 187, pages141–144 (14 August 1999).

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




