Work-life balance among junior doctors
Emily Pettifor, Charlotte Harman-Jones, Ben Harman-Jones & M Aamer Sarfraz
Cite this article as: BJMP 2020;14(1):a009
|
|
Abstract Junior doctors are known to have poor work-life balance. In this cross-sectional study, we sought to investigate factors affecting their work-life balance, and compare that seen in those working in a psychiatric and non-psychiatric healthcare setting. An existing questionnaire, the SWING, was distributed to local junior doctors working in both settings. Basic demographic data were also collected. Responses were returned by 99 junior doctors; 54 in non-psychiatric setting, and 45 in psychiatric setting. Key findings included a high negative impact of work on home life in both settings, lower levels of negative impact of home life on work, but higher in the psychiatric setting, and higher positive impact of home life on work, and work on home life, in the psychiatric setting than in the non-psychiatric setting. Correlations in results were examined and various causative associations considered. In particular, having children under 18 seemed to be a particular important association. Keywords: Wellbeing, Junior doctors, work-life balance |
Introduction
It is widely acknowledged that medicine can be a high-stress profession. The reasons behind this observation have been the focus of research over recent years, because concerns over the welfare of doctors have grown due to its relevance to burnout of individuals and safeguard of healthcare systems. However, a recent survey of hospital doctors still showed that 80% experienced workplace stress, and the junior doctors surveyed suffered significantly higher burnout rates than their consultants.1 Separate research has specifically found that junior doctors have a poor work-life balance, a composite measure of individual factors affecting wellbeing.2 There seem to be differences in the wellbeing of doctors in different specialities studied – a study in 2016 showed higher levels of leisure time enjoyed by general practitioners compared to doctors working in other specialities.3 Another survey showed that psychiatrists experienced lower levels of burnout than surgeons did.4 Furthermore, different burnout rates have been observed between consultants and junior doctors working in Psychaitry.5
We sought to build on existing research by studying the work-life balance of junior doctors and how some factors might affect that. We also decided to explore what factors might contribute to the differences in wellbeing between medical specialties and professional grades.
Method
Junior doctors working across an English county in general practice, medical and surgical specialities (the “non-psychiatric setting”), and in psychiatric specialities (the “psychiatric setting”), were recruited into a cross-sectional study between September and December 2019. To enable appropriate comparison between groups, junior doctors must have worked between the level of Foundation Year 2 (FY2) and consultant in their relevant speciality. This was necessary because the on-call responsibility of Foundation Year 1 (FY1) doctors in this locality varies significantly from that of more senior doctors.
All doctors were required to complete the SWING (Survey Work-home Interaction-NijmeGen), questionnaire6; a validated instrument measuring four aspects of work-home interaction. This questionnaire is split into negative (questions 1-12) and positive (questions 13-22) subscales, where lower and higher scores are better respectively. For each question four responses ranging from never to always could be returned. Demographic information was also collected to assess participant group similarity and identify any effect of these variables. These included age, gender, and whether they have children under the age of 18. No identifying information was requested to allow for staff anonymity, and no incentive was offered for participating.
Ethical approval for the study was granted by the local Medical Education Departments. Data from completed questionnaires was recorded in an Excel spreadsheet, which was used for collation and analysis. Significance of the between-group differences was calculated using the Chi-Squared test, with the threshold for statistical significance set at p<0.05. In order to allow comparison between the answers given for each questionnaire item, 1, 2, and 3 points were respectively allocated to each “sometimes”, “often”, or “always” response. The sum of these points for each question gave the “overall question score”, with lower and higher scores reflecting better work-life-balance on negative and positive subscales respectively. Overall question scores were also calculated as percentages of the maximum possible score for each question or subscale (i.e. if every respondent had answered “always”).
Results
Questionnaires were returned by 99 junior doctors (54 working in the non-psychiatric setting, and 45 working in the psychiatric setting). Demographic details are shown in Table 1. Not all respondents returned demographic details. There were no significant differences in the ages and genders of respondents between the two settings, but there were significantly more doctors with children <18 years in the psychiatric setting.
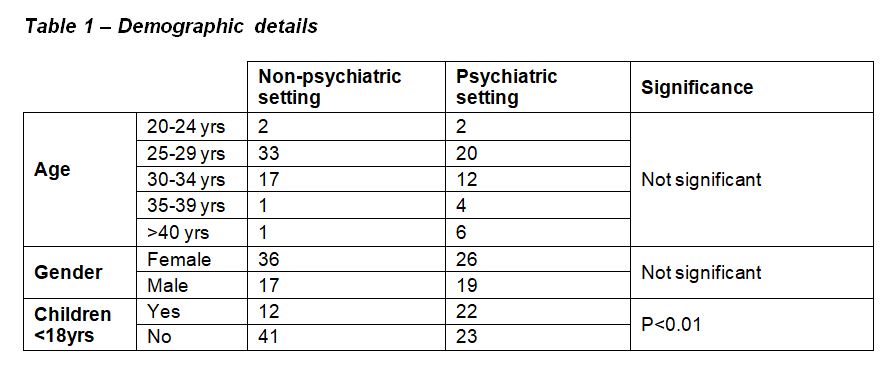
Table 1
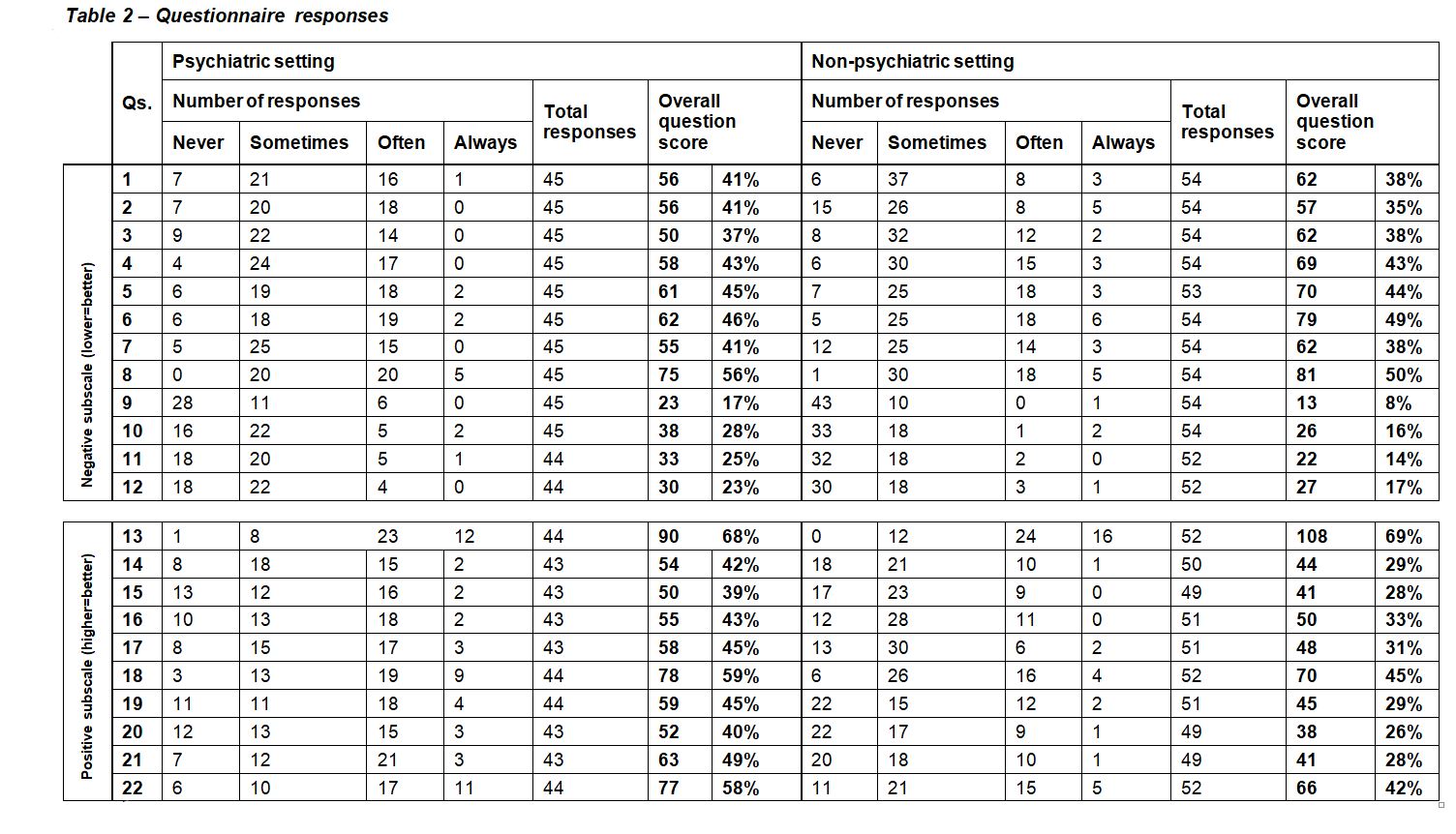
Table 2
Questionnaire responses are shown in Table 2, along with calculated overall question scores and overall subscale scores for each subscale in both settings. Differences in overall question scores between settings are shown in Figure 1 and Figure 2.
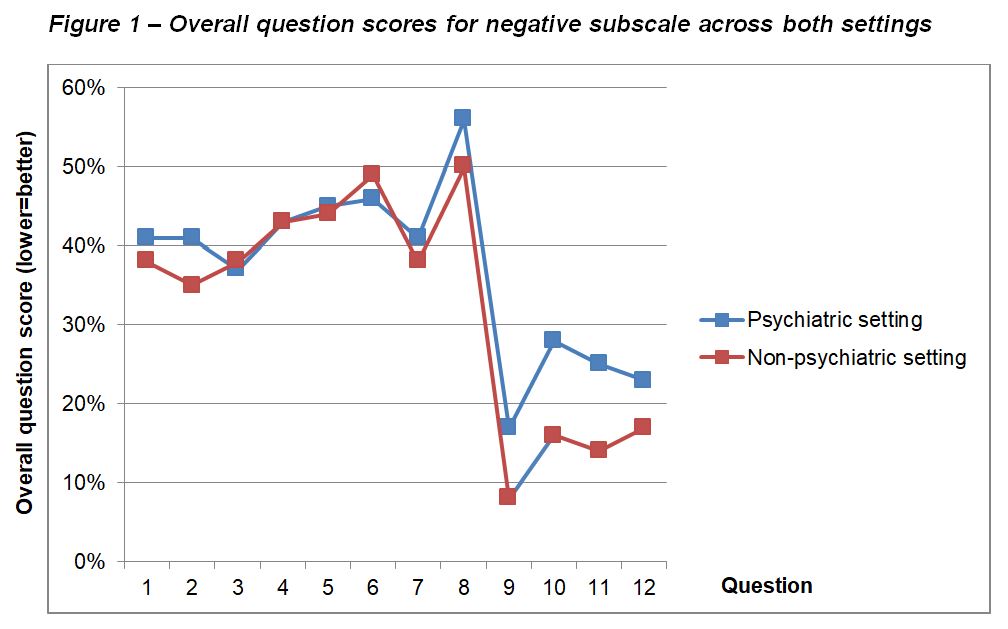
Figure1
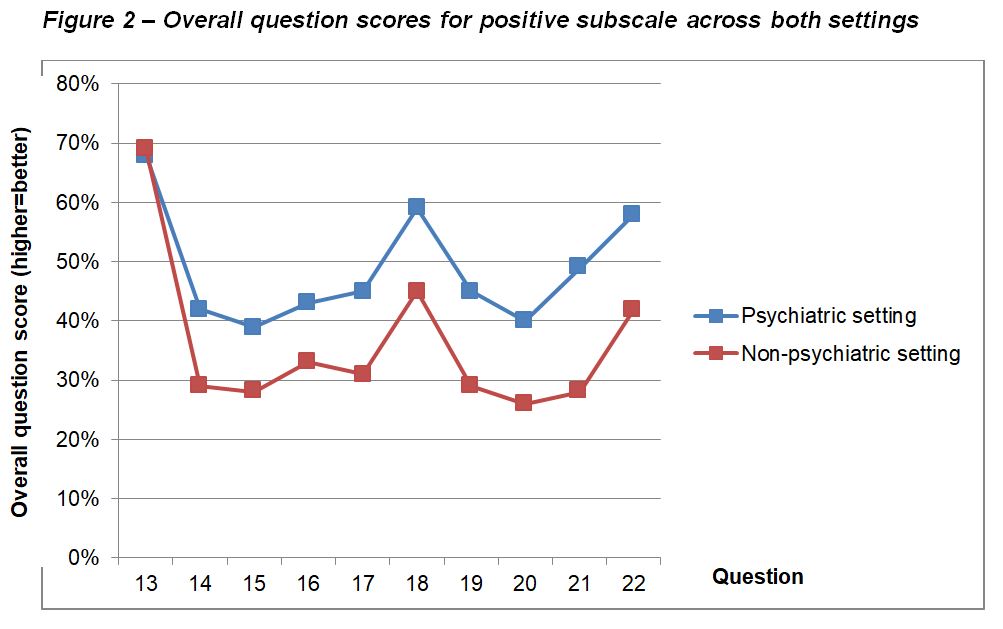
Figure 2
Overall question scores across the negative subscale were generally high, indicating a high incidence of negative work-home interaction among all respondents. Scores for questions 1-8, which ask about negative impact of work on home life, showed little/no difference between the two settings. Questions 9-12, which ask about negative impact of home life on work, recorded much lower scores in both settings, but there was separation between the settings, with scores in the psychiatric setting being higher than those in the non-psychiatric setting.
In the positive subscale, questions 13-17 ask about positive impact of work on home life, and questions 18-22 ask about positive impact of home life on work. Overall, there was a much more clear separation in scores between the two settings than that seen in the negative subscale. Aside from question 13, scores in the psychiatric setting being consistently higher than those in the non-psychiatric setting.
Main findings of this study can therefore be summarised as:
- High negative impact of work on home life in both settings
- Lower levels of negative impact of home life on work, but higher in the psychiatric setting
- Higher positive impact of home life on work, and work on home life, in the psychiatric setting than in the non-psychiatric setting
Discussion
There has been a great interest in the wellbeing of junior doctors in recent years, resulting in a number of changes in working patterns, such as the move away from the old “firm” structure to medical training, and the introduction of the European Working Time Directive.7 However, the perceived wellbeing of junior doctors in the UK seems to still be poor, and has resulted in a so-called “Drexit” of junior doctors to other countries, such as Australia, providing a better quality of life or away from medicine altogether.7 One survey shockingly revealed that almost half of UK junior doctors have considered leaving the National Health Service, citing concerns over wellbeing.7 It is, therefore, unsurprising that in 2018, only 38% of FY2 doctors continued into speciality training.8
Various aspects of junior doctor wellbeing and contributory factors have been researched. For example, a large survey of Australian junior doctors published in 2020 showed that those working only a few more hours than the average were more than twice as likely to report common mental disorders.9 Many interacting themes have been qualitatively identified, such as those found in a recent Australian qualitative survey.10 These ranged from institutional issues such as discouragement to claim overtime, to cultural issues such as not wanting to ask for assistance, to personal issues such as time for personal care. Another study found multiple factors to be correlated with higher rates of burnout in hospital doctors, including male sex, younger age, and lower years of practice.1
It seems that wellbeing in junior doctors is a highly complex, multifactorial issue with many interacting contributory factors. In addition to considering the individual factors at work, it is also necessary to consider how these factors interact on a larger scale. One way which researchers have done this, and which we have replicated, is to consider the concept of “work-life balance”, which explores the interaction between work and home life, and vice-versa. Existing research in junior doctors has found work-life balance to be particularly poor in those with children and in women, who frequently cited that this had resulted in a change in career direction.2
Unsurprisingly, we have found high levels of work negatively impacting on home life in both psychiatric and non-psychiatric settings. Since work-life balance involves many interacting components, we speculated that it may differ between junior doctors working in different medical specialities. Indeed, we detected such differences, with the reported negative impact of home life on work being higher among those trainees in the psychiatric setting than those in the non-psychiatric setting. In a cross-sectional study like ours, it is not possible to comment on causality but we noted that there were significantly more trainees in the psychiatric setting who had children. This correlates with previous findings,2 and raises the possibility of a causative relationship between having children under 18 and negative impact on work. A study of stress in psychiatrists which gathered responses from 449 participants found that sickness of children and arranging childcare were among the top five stressors identified.11
Trainees in the psychiatric setting have consistently reported higher levels of positive impact of work on home life and vice-versa. One possible explanation is that the nature of psychiatry is inherently different to other areas of medicine, with a focus on promoting the quality of patient interaction, and training time dedicated to exploring this in detail. Supervision of patient contact is also conducted more thoroughly than in other specialities, which may lead to a greater sense of being supported in clinical decision making when trainees work in psychiatry.
Strengths and limitations
Regarding strengths of this study, we used an innovative method in seeking to compare trainees across two different settings. The questionnaire used was validated and holistic in examining bidirectional interaction between work and home life. Groups were well-matched in terms of the selection of trainees with broadly similar working rotas, and in their age and sex, which have been shown to be important variables which can affect work-life balance. We also used an innovative method in analysing the questionnaire responses which enabled us to compare directly between the two settings.
There are several limitations with this methodology which identify possible interesting and important areas for future research. For example, we did not investigate for differences in work-life balance between staff working in inpatient and community settings. Additionally, it was not possible to make conclusions about causality with this cross-sectional methodology, and the use of a longitudinal method with a more detailed exploration of demographic factors may provide interesting insights in the future. Due to local factors in the way psychiatric and general healthcare services are set up in our area, it was not practical to measure participant engagement with the study, and this would have presented a barrier making this study impossible. There were however 99 responses included in this study, with similar representation in both healthcare settings, which relative to the local population of doctors in the settings studied represents a good sample.
There will inherently be local differences in working patterns, and therefore the results of this study are not directly generalizable to a national or international population. The non-psychiatric setting is broad in its scope and includes trainees undertaking varied forms of medical and surgical training, and therefore there are likely to be more subtle variations which were missed in this approach.
Conclusion
This study adds to the literature on work-life balance in junior doctors, which is an important area of research in order to promote the wellbeing of the current and future medical workforce. It also explores how factors affecting wellbeing might interact on a higher level than when studied in isolation, and how these interactions may differ depending on the medical speciality in which the respective doctors work.
Because of the local variations in working patterns, we would suggest a replication of this research in other areas in the UK and abroad. We would also suggest that an interesting area for future research may be the exploration of differences in work-life balance between narrower groups of trainees, which may aid developmental policy generation in supporting doctors to maintain a healthy work-life balance across different specialities. The group we feel would benefit from further research in particular is the trainees with young children, as we found a possible negative association between this and impact of home life on work.
|
Competing Interests None Author Details EMILY PETTIFOR, Foundation Trainee. CHARLOTTE HARMAN-JONES, Psychiatry Trainee. BEN HARMAN-JONES, Psychiatry Trainee. M AAMER SARFRAZ, Consultant Psychiatrist and Director of Medical Education. CORRESPONDENCE: Dr M. Aamer Sarfraz, Elizabeth Raybould Centre, Bow Arrow Lane, Dartford, Kent DA2 6PB, UK. Email: masarfraz@aol.com |
References
- Hayes B et al. Doctors don’t Do-little: a national cross-sectional study of workplace well-being of hospital doctors in Ireland. BMJ Open 2019; 9: e025433.
- Rich A et al. ‘You can't be a person and a doctor’: the work–life balance of doctors in training—a qualitative study. BMJ Open 2016; 6: e013897.
- Surman G, Lambert TW, Goldacre M. Doctors’ enjoyment of their work and satisfaction with time available for leisure: UK time trend questionnaire-based study. Postgrad Med J 2016; 92: 194-200.
- Pejuskovic B, Lecic-Tosevski D, Priebe S. Burnout in psychiatrists, general practitioners and surgeons. World Psychiatry 2011; 10: 1.
- Guthrie E et al. Sources of stress, psychological distress and burnout in psychiatrists. Psychiatric Bulletin 1999; 23: 207-12.
- Geurts SAE et al. Work-home interaction from a work psychological perspective: Development and validation of a new questionnaire, the SWING. Work & Stress 2005; 19 (4): 319-39.
- Forsyth RO and Suttie SA. Enhancing junior doctors’ working lives. Surgery (Oxf). 2020; 38 (10): 607-11.
- Rimmer A. Number of FY2 doctors moving straight into specialty training falls again. BMJ 2019; 364: l523.
- Petrie K et al. Working hours, common mental disorder and suicidal ideation among junior doctors in Australia: a cross-sectional survey. BMJ Open. 2020; 10 (1): e033525.
- Forbes MP, Iyengar S, and Kay M. Barriers to the psychological well-being of Australian junior doctors: a qualitative analysis. BMJ Open 2019; 9 (6): e027558.
- Rathod S et al. Stress in psychiatrists: Coping with a decade of rapid change. The Psychiatrist 2011; 35 (4): 130-134.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




