Training for anaesthetists in a new healthcare system: pathway to learning & development
Purnima Narasimhan & Krishnan Melarkode
Cite this article as: BJMP 2021;14(1):a001
|
|
Abstract Every year, a number of overseas anaesthetists move to the UK under MTI, which is a training programme to assist doctors with proven capability in anaesthesia/Intensive Care/Pain Medicine from low and middle income countries to undertake further training in anaesthesia in the UK. This initiative benefits both the trainees and the NHS. The whole process involves a lot of work and is stressful too, as the trainee has to adapt to a new environment. The awareness of these is essential for both the trainees and the supervisors, as these form barriers to learning and need to be addressed before any learning begins. The MTI trainees are adult learners with a self-image and pre-existing knowledge. Therefore, any learning strategy for them should begin with assessment of the educational needs followed by constructivism, feedback and reflection without criticism. They should be encouraged to use the same learning platform as the UK trainees for an all-round development. The supervisors can provide advance structures upon which the MTIs can continue to build opportunities and gain confidence to rehearse and apply their new knowledge. An organised induction programme, a period of familiarisation and good mentorship with patience helps to remove the barriers to learning for the MTI trainees. A dynamic trainee-supervisor relationship to accommodate the changing educational goals and an appropriate mix of strategies can help the MTI trainees attain medical competence. Keywords: Anaesthesia, Adult learning, Medical Training Initiative Abbreviations: MTI- Medical Training Initiative, NHS- National Health Service, UK- United Kingdom |
What is the MTI scheme?
The Medical Training Initiative (MTI) is a training programme to assist doctors with proven capability in anaesthesia/Intensive Care/Pain Medicine from low and middle income countries to undertake further anaesthesia training in the UK, for a maximum of 24 months1.
Why MTI?
It offers an opportunity not only to fine-tune their clinical acumen, but also to assimilate non-clinical skills (medical education, leadership and management, quality improvement projects) 2. The exposure most of the MTIs receive overseas is heterogeneous - in terms of level of supervision/independence, access to modern equipment and medications, lines of management, level of expectations and communication or interaction with patients. Funding received by training hospitals overseas can be variable thereby impacting on the resources available to provide standardised training. Under the MTI scheme, anaesthetic trainees can also take the FRCA examination.
From home to UK
A general awareness of the scheme helps the department to provide the MTIs with an appropriate support system. Details of the MTI scheme are available on the Royal College of Anaesthetists (RCoA) website.
It takes about 3-6 months after verification of the educational qualification by Educational Commission for Foreign Medical Graduates (ECFMG) via Electronic Portfolio of International Credentials (EPIC). The planning involves resignation from the current job, applying for a Tier 5 Visa to be in time for the GMC identity check (3 month deadline) and collecting the Biometric Residence Permit to be able to start work in the UK.
Medical staffing has more paperwork, one of which is the Disclosure and Barring Service (DBS). Prior intimation to the MTIs on the need for police verification from their home country would be of great benefit to make the process smoother. Hospital accommodation should be offered and organised in advance.
Acquaintance with the system
The MTI trainees often join at a time that doesn’t coincide with the UK training programme. Hence, a one-to-one induction customised towards overseas doctors will be beneficial. In addition to a named Educational supervisor (a mandatory requirement stipulated by the RCoA), the MTIs will benefit from having a nominated mentor within the department. The trainees can also get familiarised to the new healthcare system via the RCoA approved training courses – ‘Simulation for MTIs’ and ‘New to NHS’.
Allocating MTIs to theatre lists with only a select number of consultants in the initial stages helps them to settle in a new healthcare environment before they commence on-call (out of hours) duties. The MTIs should be encouraged to attend resuscitation courses like Advanced Life Support (ALS) as most of them follow the Advanced Cardiac Life Support (ACLS). They should be encouraged to document their progress like any other UK trainee via the RCoA Lifelong Learning Platform (LLP).
Anaesthetic training in the UK is very structured. The three stages of training (core, intermediate and higher/advanced) are well defined. The curriculum is well laid out and assists trainees to not only develop clinical but also gain non-technical skills. A six-monthly ARCP (Annual Review of Competence Progression) like assessment with annual anonymised multi-source feedback helps to create professional development plans, monitor progress and put supportive plans in place (if needed ) for a struggling trainee. The curriculum provides an opportunity for all-round development to every overseas trainee.
Gaining experience in non-technical skills (leadership and management, medical education and QI/audit projects) can be lacking in some home countries as the curriculum back home could be heavily biased towards the development of clinical acumen only.
What to expect from an MTI?
The MTIs have at least 3-5 years (may be more) of anaesthetic experience. The NHS benefits from their skills and experience. Their experience helps the department to allocate them to provide out of hours work (on-call) sooner than a UK trainee after an appropriate period of induction. The journey of patient experience also improves with the presence of experienced staff on the shop floor.
Departments gain from increased service provision too. As an example, after obtaining the initial assessment of competency (IAC), the MTI anaesthetists can be allocated to do solo theatre lists with a named supervising consultant anaesthetist present within the theatre suite. The reliance on locum staff is reduced thereby reducing unnecessary cancellations of theatre lists for lack of permanent staff. It reduces the financial burden on the NHS as staffing the department with locums can add to increased costs.
Patient safety is of paramount importance in any healthcare setting. Since the MTIs have a two year working contract, they are familiar with the department policies and guidelines unlike a locum doctor who does the odd shift in a hospital.
Equally, new skills gained by the MTIs are ultrasound guided regional anaesthesia, using a fibre-optic scope and different airway gadgets, ICU training, experience in geriatric and bariatric anaesthesia, total intravenous anaesthesia (TIVA) / target controlled infusion (TCI) alongside access to new medications like remifentanil, sugammadex which may not be available in low to middle income countries. The NHS provides excellent opportunities in simulation training and teaching courses.
However, a system of protocols can be unnerving to the MTIs. One may find them taking a step back when it comes to ‘decision making’ as they are not sure if it would be approved or criticised. At times, some of the MTIs may come across as unyielding despite adequate teaching. It is essential to remember that the process of unlearning to re-learning takes time, and therefore, patience is the key. This is where the concept of teaching experienced medical practitioners with knowledge comes in handy.
Training learners with knowledge
Medical education comprises three inter-linked domains - knowledge, skills and attitude.3 Though trainees may differ in terms of their motivation for learning, it can manifest only after the basic needs are satisfied - the external barriers to motivation such as life events and transitions, opportunities, and barriers to learning or obtaining information are addressed and they feel respected in the educational environment. The MTIs are essentially adult learners with pre-existing knowledge, who bring a great deal of first-hand experience to any work-place. Learning should, therefore, be integrative, which forms the basis of constructivism theory of learning4. New knowledge and skills should be integrated into the existing bank of knowledge. They also have pre-set strong tastes and habits which can be a real asset or a hindrance to effective learning. The educational supervisor should be able to encourage or curb them accordingly5.
Being adults, MTIs enter training situations with a self-image as independent, mature beings as they have already passed the qualifying exams in their home country. They can direct their own learning, including decision making and plans for taking examinations. The supervisors should engage with the trainees in activities that create a sense of self-responsibility to facilitate better learning opportunities.
Many adult learners suffer from a fear of failure and living up to expectations6 and thus, educational supervisors should be cautious to avoid unnecessary criticism. Instead the focus should be to offer constructive positive feedback. Any educational plan for them should start with an awareness of their prior acquired knowledge, an assessment of their educational needs along with room for motivation and reflection. This helps the trainees retain the original “frame of reference” while continuing to constantly challenge and transform practice via reflection on-action and reflection in-action. The educational supervisors need to provide a supporting educational environment, a structured guide for reflection and constructive feedback to develop the trainees’ reflective practice7.
A simple multi-step approach involving active participation from both the trainee and the educational supervisor can be summarised into a model as below (Figure 1) 8. This model begins with the trainee’s prior knowledge.
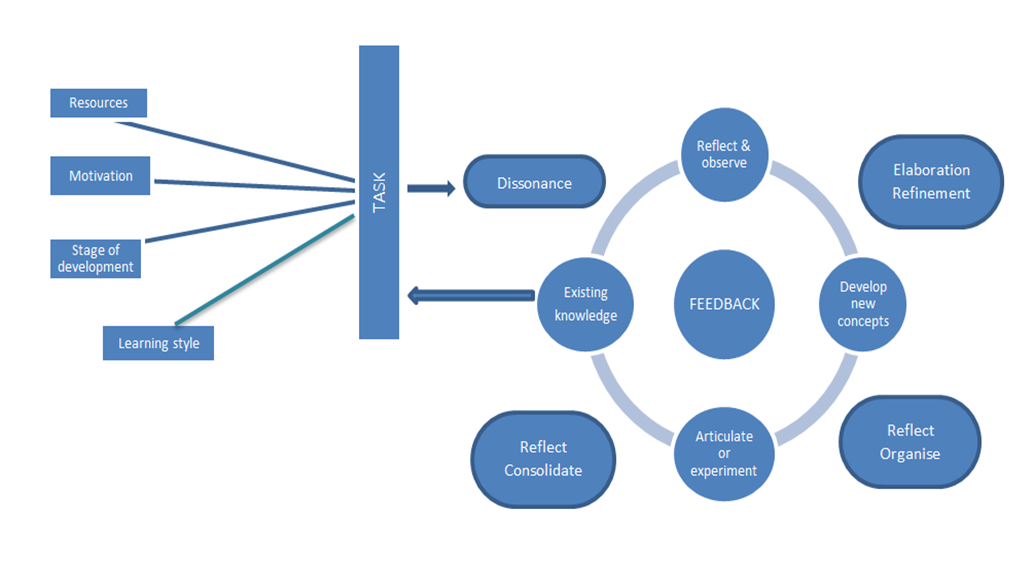
Figure 1: Multi-step approach to training
The RCoA LLP, work-place based assessments and multi-source feedback along with the six-monthly meeting with educational supervisor are useful tools to deliver a holistic learning experience. It helps to refine the existing knowledge, reflect and provide constructive feedback. The supervisor can provide advance structures upon which the MTI can continue to build opportunities and gain confidence to rehearse and apply their new knowledge.
Summary
An organised induction programme, a period of familiarisation and good mentorship with patience helps to remove the barriers to learning for the MTI trainees. A dynamic trainee-supervisor relationship to accommodate the changing educational goals and an appropriate mix of strategies can help the MTI trainees attain medical competence, which is defined as “the habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values and reflection in daily practice for the benefit of the individual and the community being served3.”
|
Competing Interests None declared Author Details PURNIMA NARASIMHAN, MBBS, MD, DNB Anaesthesiology, Pinderfields General Hospital, Wakfield, UK. KRISHNAN MELARKODE, MBBS, MD, DNB, FRCA, PGCert (medical education), Pinderfields General Hospital, Wakfield, UK. CORRESPONDENCE: Dr PURNIMA NARASIMHAN, Department of Anaesthesia, Pinderfields General Hospital, Wakefield, UK WF1 4DG Email: purni89@yahoo.com |
References
- RCoA. https://www.rcoa.ac.uk/about-college/global-partnerships/overseas-doctors-training-uk/medical-training-initiative
- World Federation of Societies of Anaesthesiologists. Medical Training Initiative. https://www.wfsahq.org/medical-training-initiative
- Abela J. Adult Learning Theories and Medical Education: a Review. Malta Medical Journal.2009; 21:11-18
- Badyal DK, Singh T. Learning Theories: The Basics to Learn in Medical Education. Int J Appl Basic Med Res. 2017 Dec; 7(Suppl 1): S1–S3.doi: 10.4103/ijabmr.IJABMR_385_17
- Thoms KJ. They’re not just big kids: motivating adult learners. http://www.mtsu.edu/∼itconf/proceed01/22.pdf
- Kennedy RC. Applying Principles of Adult Learning: The Key to More Effective Training Programs. http://www.ncjrs.gov/App/publications/abstract.aspx?ID=199990
- Mukhalalati BA, Taylor A. Adult Learning Theories in Context: A Quick Guide for Healthcare Professional Educators. Journal of Medical Education and Curricular Development. January 2019. doi: 10.1177/2382120519840332
- David C. M. Taylor & Hossam Hamdy (2013) Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83, Medical Teacher, 35:11, e1561-e1572, doi: 10.3109/0142159X.2013.828153

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




