A Rare case of Fracture in an Arthrodesed Scoliotic Spine
Suddhajit Sen & Ian Peter Wright
Cite this article as: BJMP 2019;12(1):a005
|
|
Abstract An arthrodesed scoliotic spine behaves like a long bone when fractured, with a transverse fracture configuration. This poses a problem of delayed union or non-union of these fractures. We describe a patient with fracture of her arthrodesed scoliotic spine following a trivial injury. Despite the potential severity, conservative treatment was successful in treating this injury. These injuries are extremely rare and we have not found any description of conservative treatment for these injuries elsewhere. Keywords: Arthrodesed Scoliotic spinal fracture, conservative treatment |
Introduction
Fractures in surgically fused scoliotic spines are very uncommon and only a few cases have been reported in the literature. It is not possible to predict the outcome of traumatic injuries in fused spines. There is no reported prevalence or prognostic data in the published literature and all we have are a few case reports from different parts of the world.
In this case report we describe an unusual case of a spinal fracture in a 60-year-old patient, who had surgical fusion of her scoliotic spine 50 years ago.
Case Report
A 60-year-old lady presented to A&E after a trivial fall on an icy path approximately 10 days before presentation. She had pain in her back since the fall, gradually getting worse despite escalating doses of opiate analgesics. Past medical history revealed that she had congenital lympho-haemangioma causing deformity in her back and left foot. At the age of 6 months she underwent an extensive surgical excision of the tumour along with amputation of her left foot. Subsequently she developed scoliosis at the age of 6 years, which was treated conservatively in a Milwaukee brace between the ages of 7 and 10. At the age of 10 she underwent an extensive thoraco-lumbar postero-lateral inter-transverse fusion using iliac crest bone graft without instrumentation to treat her progressive scoliotic curve. She was supported in a Milwaukee brace for further 6 months. Following this she had no problems in her back although she had a considerable residual deformity.
After this recent fall she developed pain in her right-sided thoracic hump. A full neurological examination revealed normal motor & sensory function in both lower limbs. Plain radiographs showed a thoracic scoliosis convex to the left and a broad fusion mass extending approximately from T4 to L1. There was no fracture seen. She was discharged from the A&E department with further analgesia. 3 days later she returned to A&E with increasing pain and respiratory depression due to excessive opiate usage. Investigations also revealed a very high level of serum lithium from her regular lithium medication combined with dehydration and deranged renal function. She was admitted in the high dependency unit for supportive care while the symptoms of pain and discomfort were progressively worsening. Another radiograph of her spine was again inconclusive of any bony injury. A CT scan was performed at this juncture. The CT scan (Fig. 1) showed a fracture line at the junction of T9-T10 extending through the fusion mass, with minimal displacement. She was neurologically stable on clinical examination.
The feasibility of surgical fixation of this fracture was discussed with a specialist scoliosis surgeon and a decision was made to pursue conservative treatment, considering her ongoing medical condition. Surgical fixation was deemed to be technically challenging and very risky. She was not found to be suitable for bracing either. She was advised bed rest with symptomatic management of pain, which was followed by protected and supervised mobilisation.
Further CT scans were performed after 6 weeks and after 12 weeks. These showed the fracture had remained stable but minimal signs of healing were observed with persistent gas shadows in the disc space. Throughout this she remained free of any neurological deficiency and her pain was under control. She was allowed mobilisation within the limits of comfort and under supervision. Serial CT scans were performed at the 7th month, which showed a stable spine and some callus formation at the fracture site. The latest follow up scans performed at the 12th month showed bony union had taken place (Fig 2 & 3). She was followed up in the outpatient clinic. She has resumed her normal activities and is now not requiring regular analgesia.

Figure 1- Coronal and Saggital CT Images of the Fracture from January 2011
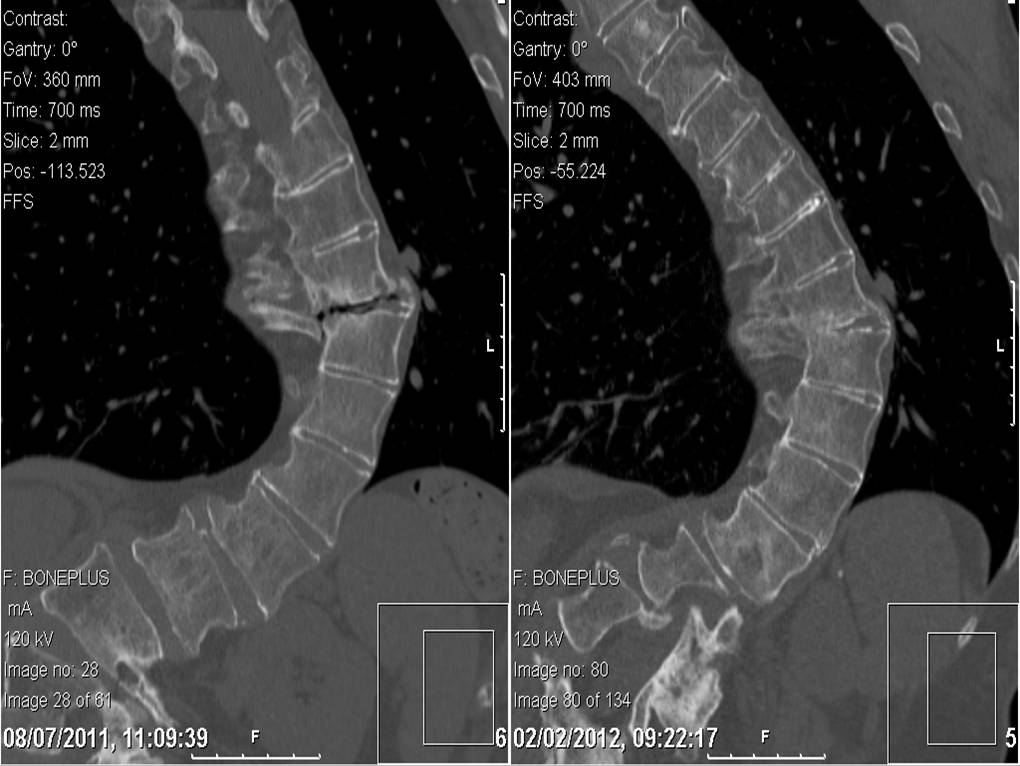
Figure 2- Coronal Images compared between July 2011 and February 2012 showing healing
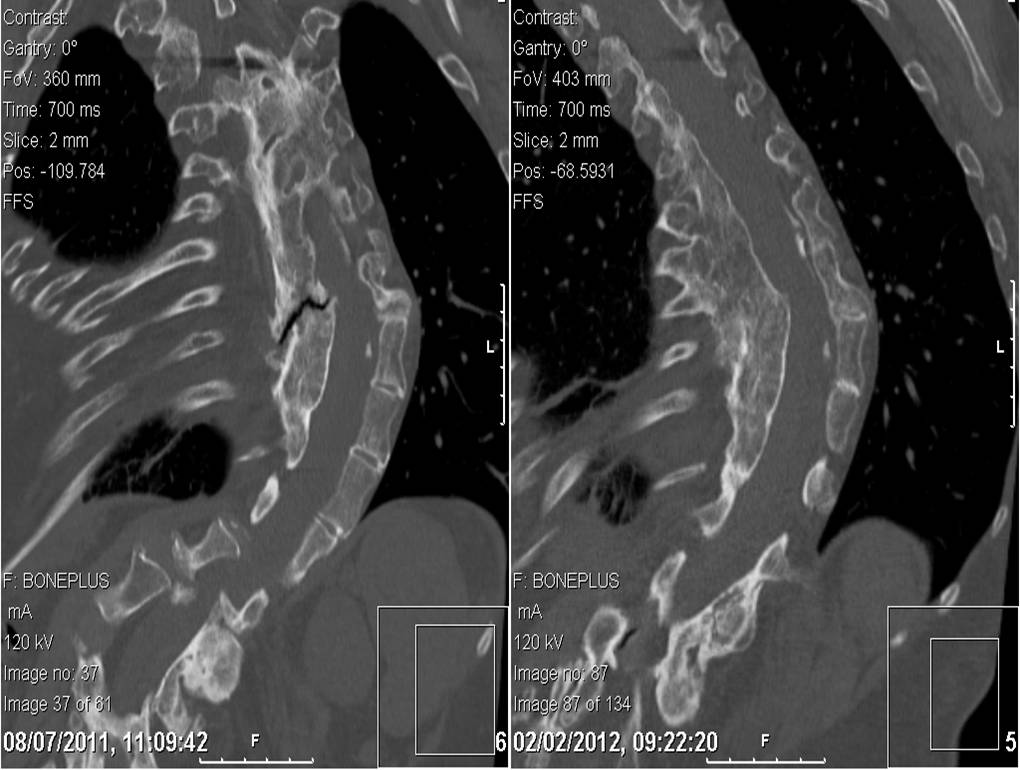
Figure 3- Saggital Images compared between July 2011 and February 2012 showing healing
Discussion
Fracture through a fused scoliotic spine is an uncommon entity. Healing of that fracture by conservative measure is fairly uncommon. Most authors point out that “the ankylosed spine breaks like a long bone, transversely, as a result of a bending force” (Bergmann)1. This fracture configuration results in higher rates of non-union and delayed union. In this light we have presented here a unique case report where a fractured fusion mass has healed without surgical intervention.
There are very few reported incidences of fracture through a spinal fusion mass after scoliosis surgery in the published literature in English. Two patients reported by Moskowitz et al2 had injuries as a result of traffic accidents. The exact mechanisms of the injuries were not described and their management was not discussed. One fractured through the fusion mass 20 years after surgery, the other 14 months after surgery.
King and Bradford3 described a fracture-dislocation of T11-T12 in a patient treated with Harrington rods. They decided to operate because of rod angulation and severe trunk de-compensation.
Tuffley and McPhee4 described a patient treated with posterior spinal fusion without instrumentation. The patient sustained a transverse fracture through the fusion mass without displacement after a fall. Posterior fixation with Harrington instrumentation was carried out.
Bagó et al5 described a 30 year old woman who had undergone anterior and posterior fusion with Cotrel-Dubousset instrumentation for progressive idiopathic scoliosis. Two years after surgery, she was in a car accident. A radiographic study and computer tomographic scanning depicted a fracture of T11 and bending of the rods. Observation was instituted and symptoms resolved.
Chung6 reported a post polio patient whose spine was fused from T7 to L4 as a teenager by spinal instrumentation, which was removed after achieving fusion. She fell down stairs fracturing the body of L2 without any neurological deficit. She was treated conservatively for 3 months after which non-union was observed. The fusion mass was fixed with an AO/ASIF broad dynamic compression plate rather than the convention spinal systems such as pedicle screws, Harrington or Luque system because of the absence of normal anatomical landmarks.
All the described case reports were from high-energy trauma unlike our case where the injury was very inconspicuous. We stress upon the fact that these injuries are very rare and can be very difficult to diagnose from plain radiographs. Our patient was fortunate not to have damaged her spinal cord, which is probably because of the low energy trauma she sustained. Our conservative management has worked well in alleviating her symptoms and achieving bony union.
|
Competing Interests None declared Author Details SUDDHAJIT SEN, FRCS(TR & ORTH), MCh ORTH, MRCS, D-ORTH, MBBS, Noble's Hospital, Isle of Man. IAN PETER WRIGHT, FRCS (TR & ORTH), MBBS, Noble's Hospital, Isle of Man. CORRESPONDENCE: SUDDHAJIT SEN, Noble's Hospital, Isle of Man, UK. Email: suddhajits@gmail.com |
References
- Bergmann, FW. Fractures of the ankylosed spine. Journal of Bone & Joint Surgery 1949;31-A: 669-671
- Moskowitz A, Moe JH, Winter RB, Binner H. Long-term follow-up of scoliosis fusion. Journal of Bone & Joint Surgery 1980; 62A: 364-76.
- King HA, Bradford DS. Fracture-dislocation of the spine after spine fusion and Harrington Instrumentation for idiopathic scoliosis. A case report. Journal of Bone & Joint Surgery 1980; 62-A: 1374-6
- Tuffley DJ, McPhee IB. Fracture of the spine after spinal fusion for idiopathic scoliosis. Spine 1984; 9:538-9
- Bagó J; Sala M; Sirera J; Villanueva C. Vertebral Fracture in a Fused Spine for Scoliosis: A Case Report; Spine: 1998 - Volume 23 - Issue 2 - pp 270-272
- Chung OM Department of Orthopaedics and Traumatology, Yan Chai Hospital, Hong Kong

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




