The less common presentation of pituitary apoplexy and its management: A case report
Huzairi Sani & Nada Syazana Zulkufli
Cite this article as: BJMP 2020;13(1):a006
|
|
Abstract Pituitary apoplexy is the event of haemorrhage, infarction or both affecting the pituitary gland. It commonly occurs in non-functioning pituitary adenoma. This case study reports an uncommon presentation of pituitary apoplexy where the patient only presented with a 2-week history of visual symptoms and was otherwise clinically stable, causing the disastrous pituitary event to be unsuspected on initial presentation. Keywords: pituitary disease, pituitary apoplexy, pituitary haemorrhage, pituitary infarction |
INTRODUCTION
The pituitary gland is a tiny gland located at the base of the brain and is connected to the hypothalamus. Dubbed as the body’s “master gland”, it produces important hormones that control many bodily functions such as those involved in the control of haemodynamics, glucose, fight or flight response, body growth and many more. Any of the pituitary hormones may be affected in pituitary disease, with acute adrenocorticotropic hormone (ACTH) deficiency being the most catastrophic and life-threatening.
Pituitary apoplexy occurs following acute haemorrhage or infarction of the pituitary gland, causing patients to be acutely unwell due to hormonal as well as local compressive effects. These effects cause the usual presentation of pituitary apoplexy such as severe headache, diplopia, visual loss and hypopituitarism.
We report a case of pituitary apoplexy that presented with a 2-week history of loss of peripheral vision and lethargy with stable vital signs.
CASE PRESENTATION
A 49 years of age gentleman complained of loss of peripheral vision in the left eye and lethargy for 2 weeks. The loss of vision was sudden, painless and non-progressive and had caused him considerable difficulties with driving where he would shift into the wrong lane and was honked at. He had no known medical or surgical history of note. Prior to presentation, he had no history of eye pain, eye redness or a history of trauma to the left eye. There were no headaches, neurological deficits or constitutional symptoms.
Clinically, he had bitemporal hemianopia with no other cranial nerve deficits. His Glasgow Coma Scale was 15/15, vital signs were stable and there was no postural change in blood pressure. Examination of other systems was unremarkable. Blood investigations revealed a decreased morning cortisol of 46 nmol/L and a normal thyroid stimulating hormone (TSH) with borderline low free thyroxine. Serum electrolytes, plasma glucose and all other anterior pituitary hormones were within reference range.
A computed tomography (CT) of the brain showed an enlarged pituitary sella with a large well-circumscribed and heterogeneously enhancing mass within. This mass measured 3.5cm x2.7cm x3.5cm (AP xW xCC) and had no calcifications within. It was also compressing onto the optic chiasm.
Two days later, a brain pituitary Magnetic Resonance Imaging (MRI) was done which reported a heterogeneous mass occupying the sella with suprasellar extension measuring 2.7 x2.8 x2.9cm (AP xW xCC) (Figures 1.1 & 1.2). This mass returned mixed solid-cystic intensity with significant enhancement post-contrast administration. There was evidence of layering within the cystic component of this mass. Inferiorly, the right border ended lower than the left (Figures 2.1 & 2.2).
Following consultations with endocrinologists, neurosurgeons and radiologists, a clinical diagnosis of pituitary apoplexy with hypocortisolism and central hypothyroidism was reached. The patient was started on oral hydrocortisone 20mg in the morning and 10mg in the evening; and oral L-thyroxine 100mcg in the morning before he was referred to the neurosurgeon for trans-sphenoidal surgery. While awaiting surgery, no clinical deterioration was reported. An endoscopic trans-sphenoidal surgery successfully took place a week later which revealed an enlarged haemorrhagic pituitary gland (Figure 3.0). The patient was discharged well a week post-surgery.
His histopathology report later confirmed pituitary adenoma where monomorphic tumour cells arranged in nests and trabeculae and some pseudorosettes were seen. The tumour cells exhibited mild pleomorphism with moderate amount of cytoplasm. The stroma was highly vascularised. No necrosis, calcification or mitosis was seen. Immunohistochemistry studies were positive for follicle-stimulating hormone (FSH) and luteinising hormone (LH) and negative for ACTH, growth hormone, prolactin and TSH.
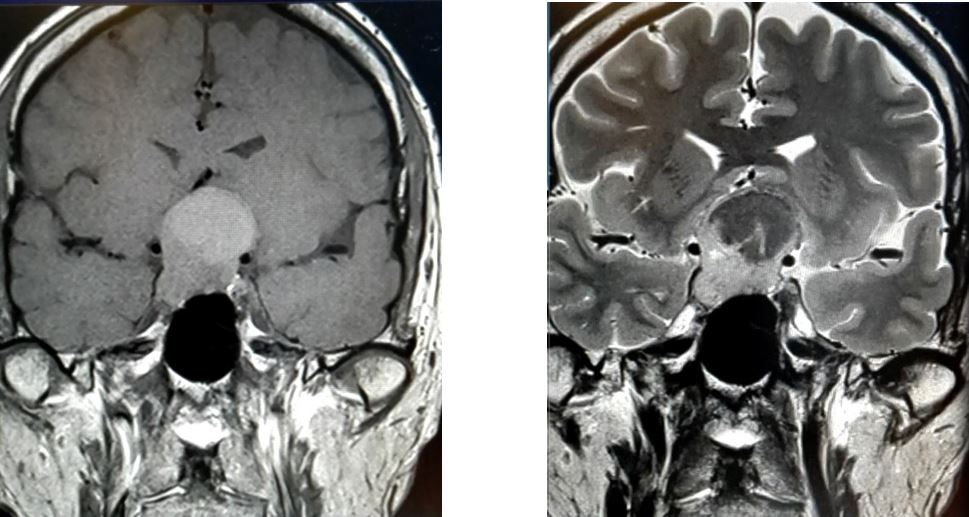
Figure 1.1 and 1.2: MRI brain on coronal view illustrating well-defined and heterogenous suprasellar mass
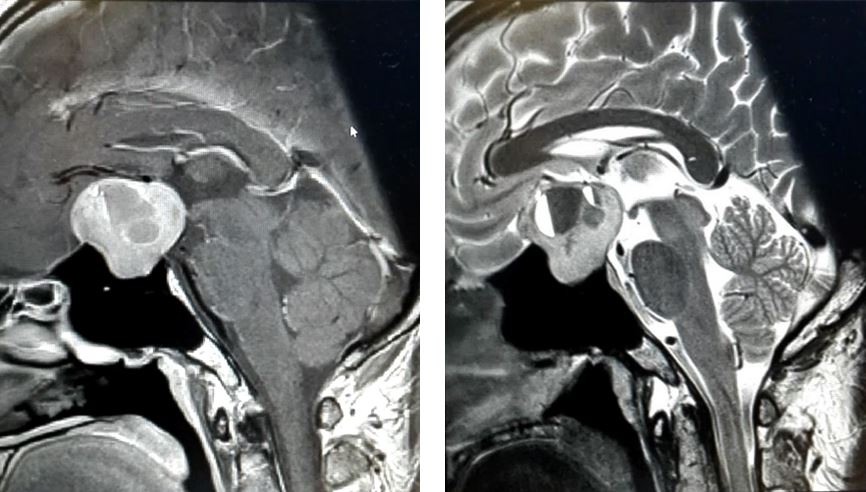
Figure 2.1 and 2.2: MRI brain on sagittal view illustrating mixed solid-cystic intensity pituitary mass
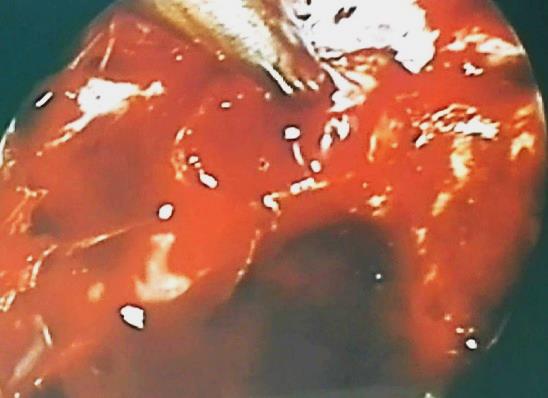
Figure 3.0: Intraoperative finding showing haemorrhage of the pituitary gland
DISCUSSION
Pituitary apoplexy is a potentially fatal condition caused by haemorrhage or infarction or both. Most cases occur during the fifth decade of life, predominantly in males.1 In the majority of cases, it is associated with a pre-existing non-functioning macro-adenoma which accounts for 14-54% of pituitary adenomas and has a prevalence of 7-41.3/100,000 population. The standardised incidence rate is 0.65-2.34/100,00.2
The many clinical presentations of pituitary apoplexy result from local compression of adjacent structures or deficiency of pituitary hormones – the former being more common where affected individuals present with headaches, visual disturbances and other symptoms of raised intracranial pressure.3
Subclinical haemorrhages refer to asymptomatic individuals with evidence of pituitary haemorrhage on MRI. In a 2018 retrospective transversal analysis involving 64 patients, 34.38% had subclinical haemorrhage within a non-functional adenoma.4 In another retrospective overview by Turgut et al, 186 cases of apoplectic pituitary adenoma presenting with monocular or binocular blindness were published in the last century.5 In a case report by Sasaki et al, a 65-year-old gentleman was only diagnosed with pituitary apoplexy following weeks of blood investigations for hyponatraemia and repeat imaging. His only presenting complaints were anorexia, low energy and fever for two weeks.6 These studies show that while an early correct diagnosis of pituitary apoplexy is important, it is not necessarily urgent.
On the other end of the spectrum, pituitary apoplexy may also present as a life-threatening situation where patients are unconscious and hemodynamically unstable due to hypopituitarism. In its acutely deficient state, ACTH causes acute adrenal insufficiency hence resulting in hypotension, hypoglycaemia, hyponatraemia and hyperkalaemia. Sometimes, non-specific symptoms precede the symptoms of hypocortisolism. A drop in consciousness level may be due to the tumour’s mass effect transmitting pressure to the brainstem or causing hypothalamic compression.7 Espinosa et al reported a 48-year-old gentleman with pituitary apoplexy who presented with the worst headache of his life, requiring urgent neurosurgical intervention which proved to be life-saving.8
Complex as it already is, diagnosing pituitary apoplexy may be further complicated when non-specific symptoms can be explained by other causes such as post-general anaesthesia drowsiness, hyponatraemia in a patient on diuretics and headaches in post-partum women receiving spinal anaesthesia.9, 10
While most patients consequently suffer from pituitary insufficiency, the extent, type and duration of therapy differs between patients. Cases of spontaneous recoveries whether a surgical or conservative approach was adopted have also been reported.11, 12 However, robust control studies comparing the outcome of surgical with conservative management in patients with pituitary apoplexy have yet to emerge. Nonetheless, studies have proven that visual outcomes significantly improve with surgery.13, 14
Having discussed the varied presentations of pituitary apoplexy, it can be agreed upon that the life-threatening endocrinal condition should be considered in any patient with abrupt neuro-ophthalmic deficits despite the state of clinical stability. This is imperative as prompt medical and surgical management may not only be life-saving, but also significantly improve visual and cranial nerve outcomes.15
CONCLUSION
Pituitary apoplexy is an endocrinal emergency which requires immediate investigation and treatment. Despite its disastrous pathology, there have been cases where affected patients present with isolated visual disturbances or with no symptoms at all. It is therefore important to have early suspicion of pituitary apoplexy in stable patients with eye complaints as early detection and management are life-saving and significantly improve neuro-ophthalmic outcome.
|
Acknowledgements We would like to thank all doctors from the Department of Endocrinology, Putrajaya Hospital, Malaysia for their expert opinion, effort and support. Competing Interests None declared Author Details HUZAIRI SANI, MBBS MRCPI MMED, Medical faculty, Universiti Teknologi MARA, Selangor, Malaysia. NADA SYAZANA ZULKUFLI, MBBS MRCPI MPATH, Department of Pathology, Penang General Hospital, Malaysia. CORRESPONDENCE: HUZAIRI SANI, Medical faculty, Universiti Teknologi MARA, Selangor, Malaysia. Email: huzairi_s@hotmail.com |
References
- Glezer A, Bronstein MD. Pituitary apoplexy: pathophysiology, diagnosis and management. Arch Endocrinol Metab. 2015;59(3):259-64.
- Ntali G, Wass JA. Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary. 2018;21(2):111-8.
- Wildemberg LE, Glezer A, Bronstein MD, Gadelha MR. Apoplexy in nonfunctioning pituitary adenomas. Pituitary. 2018;21(2):138-44.
- Cebula H, Fasciglione E, Santin MDN, Todeschi J, Severac F, Proust F, et al. Subclinical haemorrhage in non-functional adenomas. Neurochirurgie. 2018;64(1):44-8.
- Turgut M, Ozsunar Y, Basak S, Guney E, Kir E, Meteoglu I. Pituitary apoplexy: an overview of 186 cases published during the last century. Acta Neurochir (Wien). 2010;152(5):749-61.
- Sasaki Y, Nakata K, Suzuki K, Ando Y. Pituitary apoplexy presenting with anorexia and hyponatraemia. BMJ Case Rep. 2015;2015.
- Verrees M, Arafah BM, Selman WR. Pituitary tumor apoplexy: characteristics, treatment, and outcomes. Neurosurg Focus. 2004;16(4):E6.
- Espinosa PS, Choudry B, Wilbourn R, Espinosa PH, Vaishnav AG. Pituitary apoplexy: a neurological emergency case report. J Ky Med Assoc. 2007;105(11):538-40.
- Madhusudhan S, Madhusudhan TR, Haslett RS, Sinha A. Pituitary apoplexy following shoulder arthroplasty: a case report. J Med Case Rep. 2011;5:284.
- Mathur D, Lim LF, Mathur M, Sng BL. Pituitary apoplexy with reversible cerebral vasoconstrictive syndrome after spinal anaesthesia for emergency caesarean section: an uncommon cause for postpartum headache. Anaesth Intensive Care. 2014;42(1):99-105.
- Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P. Pituitary Apoplexy. Endocr Rev. 2015;36(6):622-45.
- Rajasekaran S, Vanderpump M, Baldeweg S, Drake W, Reddy N, Lanyon M, et al. UK guidelines for the management of pituitary apoplexy. Clin Endocrinol (Oxf). 2011;74(1):9-20.
- Agrawal D, Mahapatra AK. Visual outcome of blind eyes in pituitary apoplexy after transsphenoidal surgery: a series of 14 eyes. Surg Neurol. 2005;63(1):42-6; discussion 6.
- Muthukumar N, Rossette D, Soundaram M, Senthilbabu S, Badrinarayanan T. Blindness following pituitary apoplexy: timing of surgery and neuro-ophthalmic outcome. J Clin Neurosci. 2008;15(8):873-9.
- Simon S, Torpy D, Brophy B, Blumbergs P, Selva D, Crompton JL. Neuro-ophthalmic manifestations and outcomes of pituitary apoplexy--a life and sight-threatening emergency. N Z Med J. 2011;124(1335):52-9.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




