Enhancing complex communications skills in foundation doctors through simulation
Leila Jamal, Yathooshan Ramesh, Adam Monsell & Shivanthi Sathanandan
Cite this article as: BJMP 2021;14(1):a004
|
|
Abstract Background: The benefit of simulation among junior doctors is well established. Simulation programmes focussing on communication skills in medical settings have tended to focus on specific procedural aims (e.g. capacity assessments or breaking bad news). However, simulation opportunities allowing doctors to focus on meeting the needs of mental health patients in a medical setting has not been a focus of research. This is important, as people with mental health diagnoses are likely to be encountered in medical settings and junior doctors have been shown to lack confidence in approaching and managing this patient group. Method: All foundation year doctors rotating through North and East London over a 12-month period were invited to attend a simulation programme involving six patients with mental health diagnoses presenting to a medical setting. Data regarding their confidence in four domains were collected before and after the simulation, using a 5-point Likert scale. Qualitative data were also obtained and validated. Results: 121 foundation year doctors took part in the programme between May 2019 and April 2020 (N=121). Results showed a consistent increase in confidence (0.83 to 1.27 points) across all domains measured following participation in the simulation session. Increases were consistent across different sites and at different times during the programme delivery. Qualitative data were supportive of the simulation’s benefit. Conclusions: Simulation provides a useful mechanism to build junior doctors’ confidence in approaching, assessing and managing patients with mental health diagnoses in medical settings. It could be further integrated into regional teaching programmes in foundation schools. Keywords: Psychiatry, Simulated Patient, Communication Skills, Medical Education.Abbreviations: F1 - Foundation Year 1 doctor; F2 - Foundation Year 2 doctor. |
INTRODUCTION
There is considerable evidence for the benefit of simulation among foundation year doctors.1 Simulation training delivered during the 2 years has tended to focus on the management of the acutely unwell patient, procedures and practical aspects of delivering medical care, such as DNAR discussions, breaking bad news and capacity assessments.2-5 However, to date, there has been less focus on the benefits of developing more complex communication skills that may assist foundation year doctors in dealing with patients with mental health diagnoses or needs. These skills may include performing risk assessments, managing the agitated patient and forming initial management plans for patients in medical settings with mental health problems. This is important, as people with mental health needs have a higher burden of physical morbidity and are hence likely to be encountered in acute care settings.6
Since Health Education England’s Broadening the Foundation Programme report in 2014, there has been a surge in the number of foundation trainees working in psychiatry.7 The development of complex communication skills was an expected natural outcome of these rotations.8 However, this has not always happened – foundation trainees on a psychiatry rotation have stated that they are often recognised only for their medical skills, and that assessment and management was predominantly senior-led.9
Taking this into account, we set out to develop a simulation-based complex communication skills programme available for all F1s and F2s based in the North Central and East London Foundation School. Our focus was on the development of the transferable skills in communication and management that would be useful for dealing with patients with mental health diagnoses in a medical setting.
METHOD
Following a pilot study in 2018, funding was secured for 2019 from Health Education England to run half-day simulation sessions to foundation trainees in complex communication skills and the management of common mental health presentations to primary and secondary care settings.
Half-day sessions took place in hospitals in North and East London hospitals. A total of 121 foundation year doctors took part in the sessions; a breakdown of this can be seen in Table 1. All sessions took place between May 2019 and March 2020.
Table 1: Participants by Site and Year
| Year | Region | Site | Cohort | Number of trainees |
|
2019 |
North London |
Whittington | FY1 & FY2 | 9 |
| Royal Free | FY1 & FY2 | 11 | ||
| Barnet | FY1 & FY2 | 8 | ||
|
East London |
Homerton | FY2 | 16 | |
| Homerton | FY1 | 14 | ||
| Royal London | FY1 & FY2 | 3 | ||
|
2020 |
North London | Whittington | FY1 & FY2 | 19 |
|
East London |
Homerton | FY1 & FY2 | 33 | |
| Whipp’s Cross | FY1 & FY2 | 8 |
Facilitators
Each simulation group had one facilitator who offered feedback to participants. Facilitators were consultants, higher trainees and core trainees from the North and East London deaneries.
Session organisers
A session organiser was present at every session. They delivered the introductory briefing for participating doctors, provided a briefing for the actors, time-kept and held a feedback session at the end.
Venues
Four half-day sessions were run in North London, and five half-day sessions were run in East London. Three sessions were cancelled due to too few doctors registering to participate, and a further session was cancelled due to COVID-19.
Scenarios
Participants were presented with six scenarios in each session (Box 1), covering presentations in a range of settings: acute general hospitals, accident and emergency, general outpatient clinics and general practice. The sessions required skills in history taking and management when interviewing patients with complex communication needs.
| Box 1 Scenarios
1. Attempting to de-escalate an elated patient with manic symptoms and explain the need for a physical medical examination 2. Conducting a risk assessment and liaising with the psychiatric team regarding a patient who has attempted suicide and taken a paracetamol overdose 3. Assessing a patient with drug-seeking behaviour requesting a benzodiazepine prescription 4. Conducting a capacity assessment in a depressed patient who is refusing carers following a recent myocardial infarction 5. Managing an agitated patient with antisocial personality disorder who is experiencing chest pain 6. Assessment of a patient with a likely eating disorder and formulating a preliminary management plan |
Timing
Each session lasted 3 hours. Scenarios were 20 minutes each, with 10 minutes for participants to complete the set task, and 10 minutes for feedback from the facilitator, actor, and other participating doctors.
Data collection
Quantitative data
Foundation doctors were asked to complete pre- and post-session anonymous feedback forms, to ascertain their level of confidence in four domains (see Box 2): Participants were asked to rate their confidence level on a Likert scale from 1 (strongly disagree) to 5 (strongly agree) for each of these components.
| Box 2 Quantitative data statements
“I feel confident in assessing patients with mental health diagnoses” “I feel confident in making initial management plans for patients with mental health diagnoses” “I feel confident in performing initial risk assessments in a medical setting” “I feel confident in dealing with agitated patients in a medical setting” |
Post-session feedback forms also included three questions, asking if anything could have been done differently about the day, if anything was done well, and a white space for any other comments.
Qualitative data
Qualitative data was recorded in the form of the written feedback documented post session and cross-checked by three members of the organising team.
Moderations to 2020 model
Minor changes to the format of the programme were made in August 2019, following presentation of interim findings to Health Education England. These were based on feedback generated from doctors and facilitators and are shown in Table 2. The logistics of the set-up on the day, scenarios, methods of feedback collection and analysis of data remained the same as in 2019.
Table 2: Moderations to 2020 Model
| Feedback from 2019 Sessions | Updates made to 2020 Sessions |
| Title for the sessions ‘Psychiatry Communication Skills’ may have discouraged foundation trainees who were not interested in a career in psychiatry | Title changed to ‘Complex Communication Skills’ |
| The sign-up process for foundation trainees required simplification | Foundation trainees were able to book onto the session via a centralised system, which also enabled their attendance to be tracked |
| Difficulties with room availability | Medical education managers contacted early in the academic year, with centralising to larger, well-equipped sites, improving room availability |
| Some trainees were less incentivised to attend with sessions held late in the academic year | Sessions held earlier in the academic year |
| Low trainee/facilitator numbers, limiting the ability to run scenarios simultaneously | Sessions centralised with the aim to run 2 sessions in North London & 2 sessions in East London |
| Clarity of brief needed on capacity assessment scenario | Slight amendments to scenario made with
input from old age psychiatry consultant, including more details on occupational therapy assessment in the doctors’ and actors’ brief |
RESULTS
Quantitative data
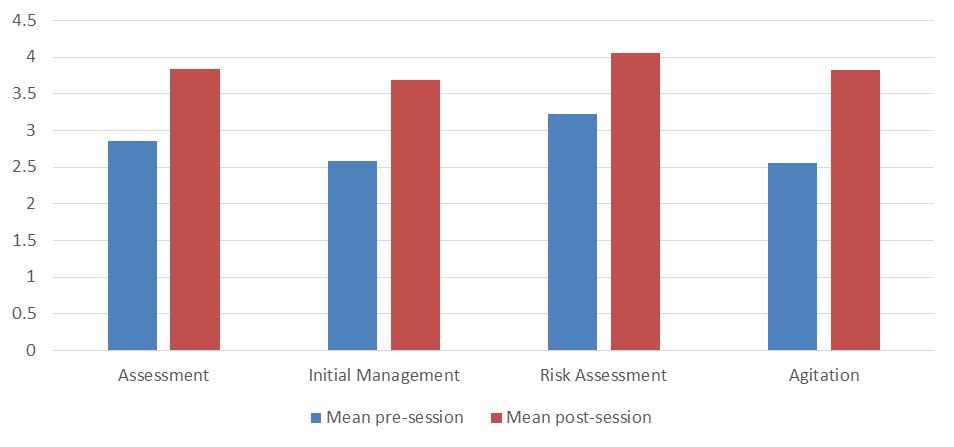
Results showed a consistent increase in confidence across all domains following participation in the simulation session. Increases ranged from 0.83 (“I feel confident in performing initial risk assessments in a medical setting”) to 1.27 points (“I feel confident in dealing with agitated patients in a medical setting”).
Figure 1: Trainee confidence pre- and post-session by domain
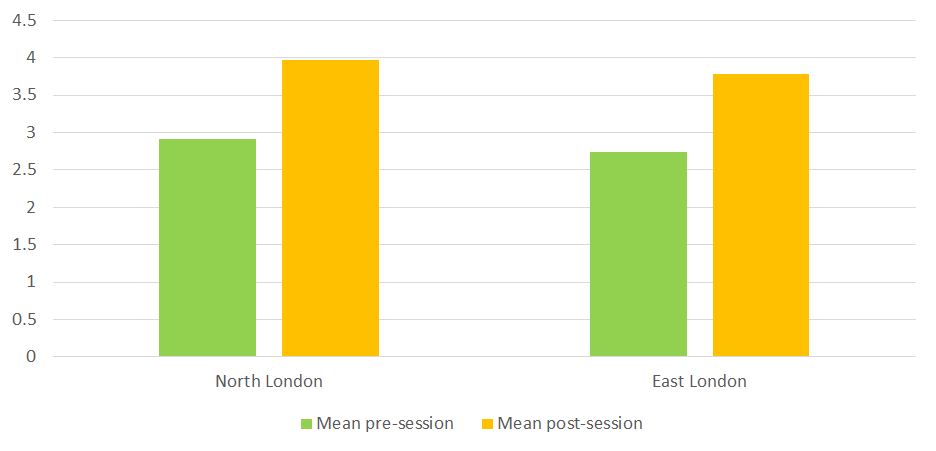
There were consistent increases in overall confidence ratings at every site, ranging from 1.03 to 1.25. Similar increases in overall confidence were observed in North London (1.04) and East London (1.06).
Figure 2: Trainee confidence pre- and post-session by region
There was a 94% (n=114) completion rate of pre-session feedback forms, and a 91% completion rate (n=110) of post-session feedback forms.
Qualitative data
No changes were made to the themes following cross-checking for validity.
Thematic analysis of the free text in the post-session questionnaires generated the following themes, as below.
Quality of the stations
Trainees consistently reported positive experiences regarding the quality of the scenarios (48), actors (43), feedback (30) and facilitators (20). In particular, there was a good breadth of scenarios, they were realisticand pitched at an appropriate level. Feedback was constructive and individualised.
“enjoyed how challenging and how true to life the scenarios were”
“right level of difficulty. Took me out of my comfort zone!”
“really good to have an agitated patient as it was a very challenging scenario”
“quite clever to have capacity assessment in somebody with capacity because it’s harder in some ways!”
Five trainees would have liked to have had more scenarios, and three suggested that it would have been useful for the facilitator to have demonstrated a ‘model’ example of a scenario at the end of the session.
Environment/logistics of the circuit
General comments included that the circuits were well organised, and that there was a comfortable atmosphere for giving and receiving feedback. Eight trainees commented that the group size was too big (all were attendees at the Homerton session in 2020, which was the largest session run with 33 trainees in attendance).
Preparation of candidates for the circuit
Ten trainees (seven in 2019; three in 2020) said they would have liked clearer briefings or objectives for the scenarios – two trainees specified that this was in relation to the capacity assessment station.
DISCUSSION
Our results suggest that simulation training involving actors with mental health diagnoses can help foundation year doctors build confidence in their approach to such patients in a medical setting.
The greatest increase occurred in participants’ confidence in dealing with an agitated patient. It is likely that participants felt the most anxious about this prior to and during the session. Thus, they were able to gain a more immediate sense of progress in this domain by being able to practice this in a ‘safe space’ and after being able to see a visible de-escalation of the patient during the station. Participants also valued receiving supportive feedback from the actor, facilitator and their peers.
Participants also demonstrated large increases in confidence with respect to formulating initial management plans. This was the domain trainees were second least confident in prior to the session. It is likely that some trainees would be anxious about whether they have enough clinical knowledge when formulating an initial management plan for mental health patients. The chance to practice this in a controlled setting, with pertinent feedback, appears to have bolstered confidence.
Results were consistent between sites, suggesting that the content of the course, the experience of being in the roleplay itself, and the chance to receive feedback from experienced clinicians were of the most importance to participants, and local variations in delivery did not impact on participants’ experience to a great extent. The wide participation among foundation trainees in North and East London (121 trainees across two regions of London, over nine simulation sessions) suggests that there is a demand for such sessions and there might be an unmet need across other deaneries.
Qualitative data analysis showed positive feedback relating to the quality of the actors, the facilitators and the scenarios themselves. This likely contributed to the trainees reporting that the simulation was realistic and pitched at the right level, hence they were able to find benefit from them.
Limitations
There was a large difference in the number of participants enrolled in each session (three in the smallest, 33 in the largest). This will have given rise to a difference in experience between these participants, with the smallest group being able to partake in all six scenarios, and the largest group only being able to partake in one. This may have meant that those undertaking all six scenarios may have been exhausted by their experience, whereas those undertaking one may have felt that they did not get enough opportunity to practise. Confidence scores between these two groups were relatively similar, but it is unclear whether there would have been a difference if they were of similar size.
Linking of pre- and post-session feedback questionnaires to the respective trainees would have also enabled testing for statistical significance. A paired t-test could have been used to assess the increase in confidence observed by our simulation sessions in each domain.
This study tracked changes in confidence among foundation year doctors following a simulation session, but it did not assess the impact on their actual practice. This would be important to ascertain, to see if the session has allowed foundation year doctors to build on their experience of assessing and managing mental health patients in a medical setting. As a result, a cohort of participants has been selected for future contact regarding this to determine the potential impact on their clinical work.
|
Competing Interests None declared Author Details LEILA JAMAL, MBBS MRCPsych, Camden and Islington NHS Foundation Trust, London, UK. YATHOOSHAN RAMESH, MBBS MRCPsych, Barnet, Enfield & Haringey Mental Health NHS Trust, London, UK. ADAM MONSELL, MBBS MRCPsych, Camden and Islington NHS Foundation Trust, London, UK. SHIVANTHI SATHANANDAN, MBBS MRCPsych, Camden and Islington NHS Foundation Trust, London, UK. CORRESPONDENCE: YATHOOSHAN RAMESH, Barnet, Enfield & Haringey Mental Health NHS Trust, Chase Farm Hospital, 127 The Ridgeway, Enfield, EN2 8JL, UK. Email: y.ramesh@nhs.net |
References
- Patel P, Sockalingam I. Acute care simulation training for foundation doctors: the perceived impact on practice in the workplace. Acute Medicine. 2013;12(3):151-158.
- Dave S. Simulation in psychiatric teaching. Advances in Psychiatric Treatment. 2012;18(4): 292-298.
- Haire E, Woods S, Wiggins N. Improving communication and documentation of end of life conversations, a simulation based project. BMJ Supportive & Palliative Care 2020;10:A17.
- Clayton J, Butow P, Waters A, et al. Evaluation of a novel individualised communication-skills training intervention to improve doctors' confidence and skills in end-of-life communication. Palliative Medicine. 2013;27(3):236-243.
- Tobler K, Grant E, Marczinski C. Evaluation of the impact of a simulation-enhanced breaking bad news workshop in pediatrics. Simulation in Healthcare. 2014;9(4):213-219.
- Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675-712.
- Perry J, Ryland H, Thoms L, Boyle A. Psychiatry in the Foundation Programme: An overview for supervisors. BJPsych Advances. 2017;23(2):123-130.
- Boyle A, Perry J. A guide to Psychiatry in the Foundation programme for supervisors. RCPsych. 2015
- Beattie S, Crampton PES, Schwarzlose C, et al. Junior doctor psychiatry placements in hospital and community settings: a phenomenological study. BMJ Open. 2017;7e017584

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




