Cutaneous Polyarteritis Nodosa: A case report
Harish J, Manjunath M N and Chaithanya C Nair
Cite this article as: BJMP 2014;7(4):a734
|
|
Abstract Cutaneous polyarteritis nodosa is a rare vasculitis of childhood relating to small-to-medium-sized arteries. Its etiology is unknown. Clinical manifestations include tender subcutaneous nodules, livedo reticularis, cutaneous ulcers and necrosis. Although it is distinct from systemic polyarteritris nodosa in that it lacks significant internal organ involvement, extra-cutaneous manifestations may be evident. The diagnosis is by skin biopsy as there is no other specific serological tests and characteristic pathologic feature is a leukocytoclastic vasculitis in the small to medium-sized arterioles of the dermis with or without fibrinoid necrosis. Mild cases may resolve with nonsteroidal anti-inflammatory drugs. If more severe, treatment with systemic corticosteroids generally achieves adequate response. We report a 10 year old girl with cutaneous PAN, who presented to us with arthralgia and swelling of left knee joint and both ankle joints and fever , with multiple tender subcutaneous nodules on both upper and lower limbs. Keywords: Cutaneous polyarteritis nodosa, subcutaneous nodules, vasculitis.Abbreviations: cPAN- Cutaneous polyarteritis nodosa, PSM- pansystolic murmur. CRP- c reactive protein, ASLO- anti streptococcal lysin O |
Polyarteritis nodosa (PAN) is a rare vasculitis in childhood. Since first described by Kussmaul and Maier in 1866 1, there have been approximately 140 pediatric case reports in the literature. Traditionally, children were classified as having one of three forms: infantile, cutaneous, and systemic. Infantile PAN is now recognized as a severe form of Kawasaki disease. Criteria for a diagnosis of systemic PAN in childhood have been proposed but not validated2.
Cutaneous PAN (cPAN) is recognized as a separate entity but there are no diagnostic criteria for cPAN2. cPAN is characterized by disease affecting the skin with no major organ system involvement. The cutaneous symptoms are similar to systemic PAN and mild fever, muscle, joint, and peripheral nervous system involvement may also occur. Fever, rash, and musculoskeletal symptoms are common in children and cPAN needs to be differentiated from other diagnostic entities. Definitive diagnosis is by histopathologic evidence of necrotizing inflammation of the medium and small-sized arteries. There is a paucity of knowledge of the spectrum of clinical presentation and management of children with cPAN. Here we describe a case of cPAN and summarize the clinical manifestations, laboratory data and treatment regimens of our patient.
Case report
This 10 year old female adolescent presented with pain in both the elbow joints followed by pain in the left knee joint and both the ankle joints in a course of 8 days and fever for the past 2 days .On admission her vitals were stable, both the elbow joints were tender and the knee and ankle joints were swollen and tender .She had multiple subcutaneous nodules over extensor aspect of both her forearms, both her tibial shins and few on her thighs. Systemic examination showed presence of a soft PSM of grade 2 intensity over left sternal edge. Blood investigations showed leucocytosis, elevated CRP, elevated ASLO titres and 2Decho revealed a mild tricuspid regurgitation. An initial diagnosis of acute rheumatic fever was made and child was started on penicillin and Aspirin. But child continued to have excruciating arthralgia and hence a rheumatologist opinion was taken. Child was advised a skin biopsy from the nodular lesions which showed small and medium vessel vasculitis suggestive of cutaneous polyarteritis nodosa. Hence she was stopped with aspirin therapy , given pulse therapy with methyl prednisolone and continued with penicillin therapy .Her arthralgia subsided within a day of pulse therapy and the subcutaneous nodules gradually disappeared .On discharge child was put on oral steroid therapy and penicillin prophylaxis and advised regular follow up.
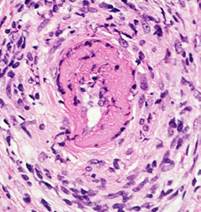
Fig1 showing segmental fibrinoid necrosis with inflammatory infiltrates of small artery.
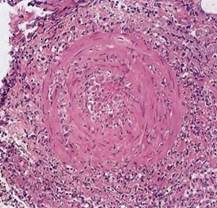
Fig2 showing leukocystoclastic vasculitis with fragmentation of neutrophils in and around blood vessels.
DISCUSSION:
cPAN is not common in the pediatric population with approximately 140 cases reported in the literature. Disease is limited to skin, joints, and muscles in the majority with a minority having nerve involvement. Constitutional symptoms are common. Most children have a chronic and relapsing benign course.
The precise etiology of cPAN remains to be unknown. However, an immune mediated mechanism has been postulated. Several infectious and noninfectious conditions have been associated both to initiation and relapse of the disease3,4,5. Among them, streptococcal infection has been commonly implicated6,7. Although some evidence of streptococcal infection as an initiating factor for cPAN is present, caution must be exercised when interpreting elevations in the serologic markers of streptococcal infection in the absence of an appropriate clinical presentation.
Cutaneous and systemic PAN share the same histopathologic features of necrotizing arteritis of small and medium sized vessels. Kussmaul and Meier described the first case of systemic PAN in 1866 1. Early reports 8,9 confirm that cPAN is a separate entity to systemic PAN. We have limited our definition of cPAN to disease affecting the skin, muscle, joints, and peripheral nervous system, with corresponding biopsy confirmation. Any evidence of visceral involvement, either clinically (central nervous system, pulmonary, cardiac, gastrointestinal, or renal), radiographically (abnormal angiography), or by histology (visceral biopsy) were classified as systemic PAN. Nakamura et al 10 proposed further restriction of the definition of cutaneous PAN in that any extracutaneous involvement such as peripheral neuropathy and myalgias must be limited to the same area as skin lesions. Systemic PAN and cPAN appear to be fairly distinct entities on a clinical continuum. There are only 5 reported cases of cPAN evolving into systemic PAN 11,12.
On review of treatment regimens reported in the literature, most children respond to corticosteroids. Penicillin should be considered in children with increased ASO titres 13,14. Recent case series report success with low-dose methotrexate, cyclophosphamide, intravenous immunoglobulin, and biologic therapies 15,16.
In summary, cPAN can be challenging to diagnose and manage. A diagnosis of cPAN should be considered in a child with fever, tender subcutaneous nodules, livido reticularis, and arthralgias/arthritis. Most children respond to corticosteroids and have a benign course, but some children may be corticosteroid dependent or corticosteroid resistant, necessitating other immunosuppressive agents including DMARDs and biologic therapy. Multicentre pediatric vasculitis disease registries are necessary to inform development and standardization of best clinical practice for childhood cPAN.
|
Acknowledgements Department Of Pediatrics and Medical Records Department, Kempegowda Institute Of Medical Science, Bangalore, India. Competing Interests None declared Author Details HARISH J, MD, Assistant Professor, Department of Pediatrics, Kempegowda Institute of Medical Science, Bangalore, India. MANJUNATH M N, Junior Resident, Department of Pediatrics, Kempegowda Institute of Medical Science, Bangalore, India. CHAITHANYA NAIR , Junior Resident, Department of Pediatrics, Kempegowda Institute of Medical Science, Bangalore, India. CORRESPONDENCE: DR MANJUNATH M N, Junior Resident, Department Of Pediatrics, Kempegowda Institute Of Medical Science, K R Road, VV Puram, Bangalore 560004, India. Email: drmanju.drmanju@gmail.com |
References
- Kussmaul A, Maier R. Über eine bisher nicht beschriebene Arterienerkrankung (Periarteritis nodosa), die mit Morbus Brightii und mit rapid fortschreitender allgemeiner Muskellähmung einhergeht. Deutsches Archiv für Klinische Medizin. 1866;1:484–518.
- Ozen S, Pistorio A, Iusan SM, et al. EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: final classification criteria. Annals of the Rheumatic Diseases. 2010;69(5):798–806.
- 3.Daoud MS, Hutton KP, Gibson LE. Cutaneous periarteritis nodosa: a clinicopathological study of 79 cases. Br J Dermatol. 1997;136:706–713.
- Misago N, Mochizuki Y, Sekiyama-Kodera H, Shirotani M, Suzuki K, Inokuchi A, Narisawa Y. Cutaneous polyarteritis nodosa: therapy and clinical course in four cases. J Dermatol. 2001;28:719–727.
- Dohmen K, Miyamoto Y, Irie K, Takeshita T, Ishibashi H. Manifestation of cutaneous polyarteritis nodosa during interferon therapy for chronic hepatitis C associated with primary biliary cirrhosis. J Gastroenterol. 2000;35:789–793.
- Till SH, Amos RS. Long-term follow-up of juvenile-onset cutaneous polyarteritis nodosa associated with streptococcal infection. Br J Rheumatol. 1997;36:909–911
- Albornoz MA, Benedetto AV, Korman M, McFall S, Tourtellotte CD, Myers AR. Relapsing cutaneous polyarteritis nodosa associated with streptococcal infections. Int J Dermatol. 1998;37:664–666.
- Diaz-Perez JL, Winkelmann RK. Cutaneous periarteritis nodosa. Archives of Dermatology. 1974;110(3):407–414.
- Borrie P. Cutaneous polyarteritis nodosa. British Journal of Dermatology. 1972;87(2):87–95.
- Nakamura T, Kanazawa N, Ikeda T, et al. Cutaneous polyarteritis nodosa: revisiting its definition and diagnostic criteria. Archives of Dermatological Research. 2009;301(1):117–121.
- Magilavy DB, Petty RE, Cassidy JT, Sullivan DB. A syndrome of childhood polyarteritis. Journal of Pediatrics. 1977;91(1):25–30.
- David J, Ansell BM, Woo P. Polyarteritis nodosa associated with streptococcus. Archives of Disease in Childhood. 1993;69(6):685–688
- Kumar L, Thapa BR, Sarkar B, Walia BNS. Benign cutaneous polyarteritis nodosa in children below 10 years of age—a clinical experience. Annals of the Rheumatic Diseases. 1995;54(2):134–136.
- Fink CW. The role of the streptococcus in poststreptococcal reactive arthritis and childhood polyarteritis nodosa. Journal of Rheumatology. 1991;18(29):14–20
- 15.Eleftheriou D, Melo M, Marks SD, et al. Biologic therapy in primary systemic vasculitis of the young. Rheumatology. 2009;48(8):978–986.
- Ozen S, Anton J, Arisoy N, et al. Juvenile polyarteritis: results of a multicenter survey of 110 children. Journal of Pediatrics. 2004;145(4):517–522.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




