COVID-19, Diagnostic Difficulties and Acute Psychosis
Abhinav Vepa, Amer Saleem, Diana Dharmaraj & Qasim Afzaal
Cite this article as: BJMP 2020;13(1):a002
|
|
Abstract Background: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) or COVID-19, has emerged as an epidemic contributing to more than 247,000 deaths worldwide as of 4th May 2020. It commonly presents with respiratory and occasionally gastrointestinal symptoms. Here we describe a rare case of COVID-19 presenting with acute psychosis which was also complicated by a false negative RT-PCR nasopharyngeal swab upon hospital admission. Case Report: A 40 year old, previously fit and healthy male, presented to accident and emergency with respiratory tract symptoms and fever during the COVID-19 outbreak. His first RT-PCR nasopharyngeal swab tested negative for COVID-19, but due to a strong clinical suspicion of COVID-19, CT imaging was conducted which justified the sending of a repeat swab. In the meantime, he started to exhibit symptoms of acute psychosis such as hallucinations, paranoid delusions, an attempted suicide, derealisation and depersonalization. Due to failed conservative measures and haloperidol in managing acute psychosis, the patient was intubated for 24 hours. After extubating the patient recovered to baseline within 2 days. Discussion: There are two clinically relevant learning points to be noted from this case report. Firstly, RT-PCR nasopharyngeal COVID-19 swabs are estimated to be only 70-75% sensitive, whereas CT scan changes are estimated to be as high as 97%-98% sensitive. CT imaging can thus be useful when there is a strong suspicion of COVID-19 despite negative nasopharyngeal swabs. Secondly, in order to reduce the work of breathing secondary to agitation, the cross-infection risks to others, and the risk of repeated suicide attempts, this patient was successfully managed with intubation and ventilation, despite the absence of respiratory failure. Conclusion: False negative rate with RT-PCR COVID-19 nasopharyngeal swabs is high and this identifies a crucial diagnostic role for CT Thorax in swab-negative, symptomatic patients with suspected COVID-19. Secondly, acute psychosis is an emerging indication for intubation to consider when managing patients with highly virulent respiratory infections, such as COVID -19. Keywords: COVID-19; Case Report; nasopharyngeal swab; acute psychosis; intubation; diagnosis; cross-infectionAbbreviations: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2, or, COVID-19), World Health Organisation (WHO), Real Time-Polymerase Chain Reaction (RT-PCR), Respiratory Syncytial Virus (RSV), Antero-Posterior (AP), Computerized Tomography (CT), Ground-Glass Opacification (GGO) |
Background:
In December 2019, the Wuhan province of China was struck by an outbreak of viral pneumonia due to the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) or COVID-19.1 On the 30th of January, WHO declared a state of global emergency due to the rapid spread of COVID 19 2 and since then it has developed into an epidemic, contributing to over 247,000 global deaths as of 4th May 2020. COVID-19 has commonly presented with respiratory symptoms, but some gastrointestinal symptoms have also been described.3, 4 Here we describe a rare case of COVID-19 presenting with acute psychosis with initially false negative RT-PCR nasopharyngeal swab upon hospital admission.
Case Review
A 40 year old, previously fit and healthy male, with a six day history of dry cough, breathlessness and nasal congestion, presented to accident and emergency via ambulance. Prior to the respiratory tract symptoms, he had a progressively worsening fever, anosmia and intermittent diarrhoea for four days. His observations included a temperature of 39⁰C, oxygen saturations of 95% on room air and a respiratory rate of 30. His initial laboratory tests are shown in Table 1 and imaging in Figure 1.
Table 1: Table showing the relevant laboratory results of the patient upon admission
| Investigations | Value | Reference Range |
| White cell count (x109/L) | 12.0 | 3.7 - 11.1 |
| Neutrophil count (x109/L) | 10.3 | 1.7 - 7.5 |
| Lymphocyte count (x109/L) | 1.1 | 0.9 - 3.2 |
| C-reactive protein (mg/L) | 190 | 0 - 6 |
| Cerebrospinal Fluid Protein (g/L) | 2.4 | 0.15 - 0.45 |
| Cerebrospinal Fluid Glucose (mmol/L) | 3.7 | 2.5 - 4.5 |
| Cerebrospinal Fluid White Cells (/µL) | 0 | 0 - 5 |
| Influenza A, B and RSV nasopharyngeal swab | Negative | |
| COVID-19 nasopharyngeal swab | Negative | |
| Pneumococcal urine antigen | Negative | |
| Legionella urine antigen | Negative | |
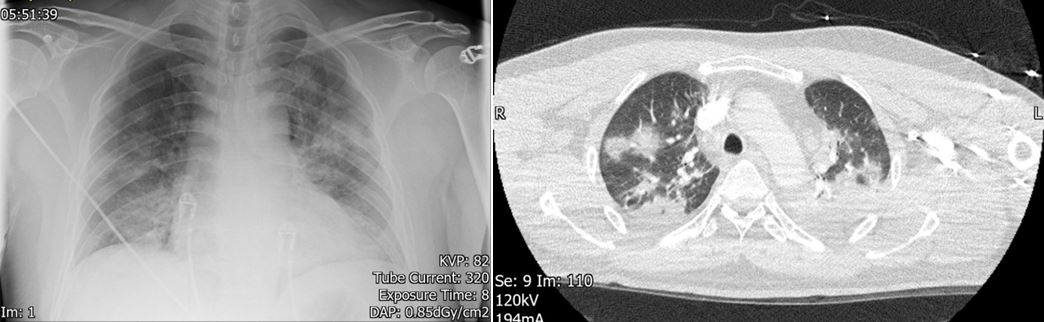
Figure 1: (Left) An AP X-ray showing bilateral patchy consolidation. (Right) A cross-sectional CT thorax image showing multifocal, peripheral, bilateral, ground-glass opacities with bilateral consolidation.
Over the course of the next two days, he developed acute confusion. A CT scan of his head was done in the first instance to identify any intracranial cause of confusion, but the scan was unremarkable. His behaviour included severe anxiety, aggression, wandering and agitation. His wife confirmed that he had never behaved like this before and had no history of psychiatric illness. He felt as if he was living in a dream, exhibiting derealisation and depersonalization. Worryingly, he also experienced suicidal ideation which he hoped would bring him back to reality. One of the ways in which he tried to kill himself was by jumping out of the hospital window. Due to verbal and non-verbal de-escalations being ineffective, 5mg of Haloperidol was given, but failed to settle the patient. This was the maximum daily dose of haloperidol in accordance with the British Geriatric Society Guidelines for the management of COVID-19 related confusion5. Subsequently, the patient was successfully managed with intubation and ventilation for 24 hours, despite the absence of respiratory failure. After extubating, he recovered back to baseline over 2 days, during which a 2nd RT-PCR nasopharyngeal swab result returned positive for COVID-19. After recovery, he had insight into the events that took place prior to intubation. Retrospectively, he reported auditory hallucinations of hospital staff talking about him all day and night, and the delusions that the hospital staff were against him, and that he was in a dream which could only be escaped by committing suicide.
Discussion
There are two clinically relevant learning points to convey from this case relating to, firstly, the difficulties encountered in diagnosis and, secondly, the management of acute psychosis in COVID-19 with intubation. The diagnosis of COVID-19 was confounded by the first nasopharyngeal RT-PCR swab being negative. Since his symptoms were typical of COVID-19 and with strongly suggestive radiographic findings, it was deemed appropriate to send a repeat COVID-19 nasopharyngeal RT-PCR swab (which indeed came back positive). This patient thus had COVID-19 pneumonia and the official diagnosis was delayed due to a false negative nasopharyngeal RT-PCR swab upon hospital admission.
Various studies have identified a high false negative rate with the COVID-19 swab.6, 7 Ai et al., describes 287 patients (n=1014) who had radiographic findings suggestive of COVID-19 with negative nasopharyngeal swabs.8 It is important for clinicians to be aware of the poor sensitivity of the RT-PCR COVID-19 swab so that it can be interpreted appropriately when being used to make clinical decisions. Various studies have estimated the RT-PCR COVID-19 swab sensitivity to be approximately 70-75%.9 This is hypothesised to be even lower if clinical staff do not use the correct technique when taking the nasopharyngeal swab. Subsequently, there is a growing clinical need for more sensitive laboratory tests for COVID-19 such as antibody tests.10
Chest radiographs may be normal in early or mild disease, but can assist diagnosis. Of patients with COVID-19 requiring hospitalisation, only 69% had an abnormal chest radiograph at the initial time of admission. Findings are most extensive about 10-12 days after symptom onset. The most frequent findings are bi-basal, peripheral, consolidative and ground-glass airspace opacities. In contrast to parenchymal abnormalities, pleural effusion is rare.11, 12 Indeed, this patient’s chest radiograph shown in Figure 1 (left) was performed after 10 days of symptoms, showing features of COVID-19.
The primary findings on CT have been reported in multiple studies to include ground glass opacification, ‘crazy-paving’ texture, air space consolidation, broncho vascular thickening, adjacent pleural thickening and traction bronchiectasis. The ground glass, or consolidative, opacities are usually bi-basal, peripheral and ill-defined.13-18 Four stages on CT have been described, as shown in Table 2 below.19, 20 This patient’s CT Thorax shown above in Figure 1 (right), was performed after 12 days of symptoms and displays features in keeping with the ‘peak’ stage.
Table 2: Table showing the radiographic staging of COVID-19
| Stage | Timescale | Radiographic Findings |
| Early/initial stage | 0-4 days | Normal CT or GGO only |
| Progressive stage | 5-8 days | Increased GGO and crazy paving appearance |
| Peak stage | 9-13 days | Consolidation |
| Absorption stage | 14 days< | With an improvement in the disease course, "fibrous stripes" appear and the abnormalities resolve at one month and beyond |
It is important to mention that in a retrospective, COVID-19 case-controlled study of 104 patients, 54% of asymptomatic patients had CT radiographic features in keeping with COVID-19.21 CT scan changes are estimated to be as high as 97%-98% sensitive and can thus be useful when there is a strong suspicion of COVID-19 despite negative nasopharyngeal swabs.8, 9, 22 This can avoid clinicians having a false sense of security when managing potential COVID-19 patients who may otherwise be nursed in open bays, consequently exposing unprotected clinical staff and patients; a common problem that we unfortunately encounter in our clinical practise.
The second interesting learning point in this case is with regards to the clinical reasoning behind why this patient was intubated. Patients with severe COVID-19 symptoms such as hypoxaemia, respiratory distress, shock or an SpO2 of <90% are usually commenced on supplemental oxygen therapy of 5L/min, which should then be titrated to maintain an SpO2 of >94%. Continuous positive airway pressure or non-invasive ventilation can then be trialled, and if ineffective, the patient can be intubated for ventilation.23 This patient’s SpO2 prior to intubation was 94%. Interestingly in this case, the clinical reasoning behind intubation was not respiratory failure, but instead acute psychosis secondary to COVID-19 which had failed to respond to conservative de-escalation measures, as well as haloperidol.
The intubation of this patient aimed to reduce respiratory effort, cross-infection risk, as well as prevent further suicide attempts. As mentioned in the history above, this patient was non-compliant with isolation regulations as he was severely confused and wandering around clinical areas, thus posing a cross-infection risk to staff and other patients.24 Self-isolation precautions have been heavily implemented in the UK because COVID-19 is an extremely virulent infectious disease.25 The basic reproductive number of COVID-19 has been estimated to be 1.55-5.5,26,27 making it more infectious than the seasonal influenza, at 1.28.28 This highlights the importance of strictly following isolation protocols, and thus, the rationale behind intubation.
Conclusion
There are two primary learning points to be appreciated from this case report. Firstly, the false negative rate with RT-PCR COVID-19 nasopharyngeal swabs is high, and this identifies a crucial diagnostic role for CT Thorax in ‘swab-negative’, symptomatic patients with suspected COVID-19. Secondly, acute psychosis is an emerging indication for intubation to consider when managing patients with highly virulent respiratory infections, such as COVID -19. The mechanisms behind COVID-19 induced acute psychosis remained yet to be elucidated, but, in this case, COVID-19-induced encephalitis was amongst the differential diagnoses.
|
Competing Interests None declared Author Details ABHINAV VEPA, BSC, MBBS, Milton Keynes University Hospital, Standing Way, Eaglestone, Milton Keynes, MK6 5LD, UK. AMER SALEEM; BSC, MBBS, MCPS MEDICINE (PAK), MRCP (UK), FCPS Pulmonology ((PAK), FRCP (Glasgow), FCCP (USA), european diploma in adult respiratory Medicine, Speciality Certificate In Respiratory Medicine (RCP UK); Consultant Chest Physician, Respiratory Medicine, Milton Keynes University Hospital, Standing Way, Eaglestone, Milton Keynes, MK6 5LD, UK. DIANA DHARMARAJ, MUDR, Milton Keynes University Hospital, Standing Way, Eaglestone, Milton Keynes, MK6 5LD, UK. QASIM AFZAAL, BSC, MBBS, Milton Keynes University Hospital, Standing Way, Eaglestone, Milton Keynes, MK6 5LD, UK. CORRESPONDENCE: ABHINAV VEPA, Milton Keynes University Hospital, Standing Way, Eaglestone, Milton Keynes, MK6 5LD, UK. Email: Dr_a_vepa@hotmail.com |
References
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 March 28;395(10229):1054-1062.
- Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. 2020 Mar;25(3):278-80.
- Lovato A, De Filippis C, Marioni G. Upper airway symptoms in coronavirus disease 2019 (COVID-19). Am J Otolaryngol. 2020 Apr;4:102474.
- D'Amico F, Baumgart DC, Danese S, et al. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention and management. Clin Gastroenterol Hepatol. 2020 Apr;8:S1542-3565(20):30481-X.
- British Geriatric Society. Coronavirus: Managing delirium in confirmed and suspected cases [Internet]. Good Practise Guide 2020 [Updated 2020 25th March, Cited 2020 20th April]. Available from: https://www.bgs.org.uk/resources/coronavirus-managing-delirium-in-confirmed-and-suspected-cases
- Li D, Wang D, Dong J, et al. False-Negative Results of Real-Time Reverse-Transcriptase Polymerase Chain Reaction for Severe Acute Respiratory Syndrome Coronavirus 2: Role of Deep-Learning-Based CT Diagnosis and Insights from Two Cases. Korean J Radiol. 2020 Apr;21(4):505-508.
- Winichakoon P, Chaiwarith R, Liwsrisakun C, et al. Negative Nasopharyngeal and Oropharyngeal Swab Does Not Rule Out COVID-19. J Clin Microbiol. 2020 Feb 26. doi: 10.1128/JCM.00297-20.
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020 Feb;26:200642.
- Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;19:200432
- Petherick A. Developing antibody tests for SARS-CoV-2. Lancet. 2020 Apr;4:395(10230):1101-1102.
- Wong HYF, Lam HYS, Fong AH, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology. 2019 March;27:201160.
- Rodrigues J.C.L., Hare S.S., Edey A. An update on COVID-19 for the radiologist: a British society of Thoracic Imaging statement. Clin Radiol. 2020 May;75(5):323–325
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020 Apr;20(4):425-434.
- Xu X, Yu C, Qu J, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020 May;47(5):1275-1280.
- Xu YH, Dong JH, An WM, et al. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect. 2020 Apr;80(4):394-400.
- Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020 Apr;80(4):388-393.
- Wang K, Kang S, Tian R, et al. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin Radiol. 2020 May;75(5):341-347.
- Li X, Zeng W, Li X, et al. CT imaging changes of corona virus disease 2019(COVID-19): a multi-center study in Southwest China. J Transl Med. 2020 Apr 6;18(1):154.
- Pan F, Ye T, Sun P, et al. Time Course of Lung Changes on Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology. Doi:10.1148/radiol.2020200370.
- Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. Doi:10.1007/s00330-020-06731-x.
- Inui S, Fujikawa A, Jitsu M et al. Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiol Cardiothorac Imaging . 2020;2(2):e200110.
- Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. Am J Roentgenol. 2020 Mar 4:1-7.
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020 Mar 28.doi:10.1007/s00134-020-06022-5.
- Ferioli M, Cisternino C, Leo V, et al. Protecting healthcare workers from SARS-CoV-2 infection: practical indications. Eur Respir Rev. 2020 Apr 3;29(155).
- Mahase E. Coronavirus covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020 Feb 18;368:m641.
- Wu JT, Leung K, Bushman M, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. 2020 (1-5). doi: 10.1038/s41591-020-0822-7.
- Zhao S, Ran J, Musa SS, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214-217.
- Biggerstaff, M., Cauchemez, S., Reed, C. et al. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infect Dis 14, 480 (2014). https://doi.org/10.1186/1471-2334-14-480

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




