Calcinosis Cutis in a Neonate
Murtaza Rashid, Bader Alotaibi, Imran Shah, Mostafa Alsomali, Mohammed Badawy & Qurat ul Ain Khawar Raza
Cite this article as: BJMP 2019;12(2):a009
|
|
Abstract Calcinosis Cutis corresponds to deposition of calcium salts in skin. It most commonly occurs in adults who have connective tissue disorders. It is rarely seen in neonates. We describe a case in which a neonate with leg swelling presented and imaging showed calcium deposits underneath the skin. Calcium gluconate is frequently used in the neonatal age group to correct hypocalcemia which if extravasated can lead to calcinosis cutis. Treatment is mostly supportive but excluding other potential causes, especially infection, is essential. Keywords: Calcinosis Cutis, calcium Gluconate, Neonate |
Introduction
Calcinosis cutis involves deposition of calcium salts in skin and subcutaneous tissue. It is commonly associated with autoimmune connective tissue diseases and can be a source of pain and disability1. It can occur in damaged or devitalized tissues in the presence of abnormal or even normal calcium/phosphorus metabolism. These calcifications can lead to contractures, muscle atrophy, skin ulceration and infections2. There are four types of calcinosis cutis: idiopathic, dystrophic, metastatic, and iatrogenic. Determining the type of calcinosis is very important for accurate management3.Calcinosis cutis is a condition seen in the middle to elderly aged population and has rarely been described in neonates in the medical literature. We discuss a neonate in the succeeding text who presented to our Emergency department with a leg swelling.
Case Report
A 20 days old full term neonate was brought to our Emergency department with right leg swelling for the past ten days. He was feeding well and was afebrile. On examination there was swelling of right lower leg including the right foot with minimal redness of overlying skin. We did x-rays of the right foot and right leg, which showed a sheath of cutaneous calcification in right foot (Image A and Image B) and anterior-lateral of right leg (Image C and Image D).

Image A
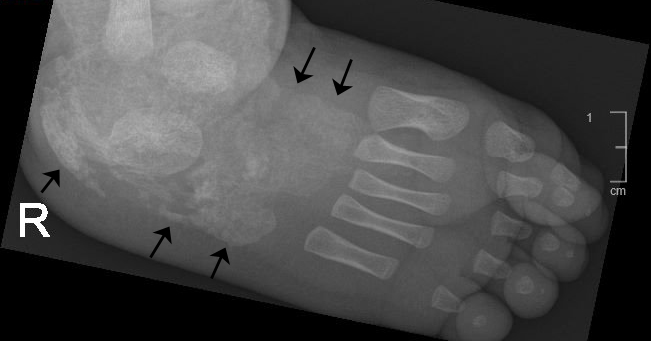
Image B
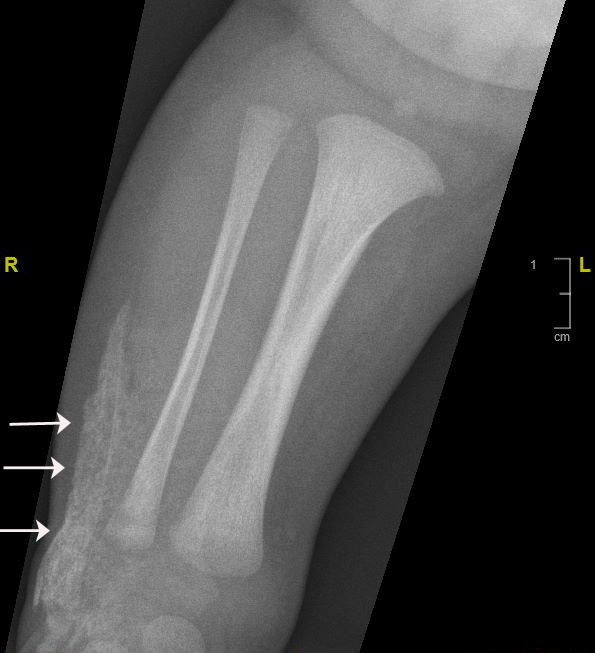
Image C
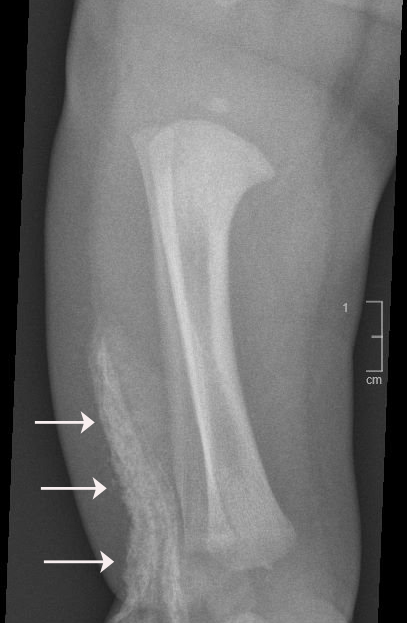
Image D
There was no evidence of any bony destruction. White cell count and other inflammatory markers were normal. Upon reviewing the previous records we found that soon after the birth the neonate was admitted with pneumonia and during the hospital admission there was extravasation of calcium gluconate infusion at the dorsum of the right foot which explains the whitish sheath seen in the imaging. Musculoskeletal ultrasound did not reveal any signs of fluid collection or periosteal swelling. The patient was treated conservatively and regular follow up was insignificant and showed complete regression of the swelling three months later.
Discussion
Calcinosis cutis is an uncommon disorder caused by an abnormal deposit of calcium phosphate in the skin in various parts of the body. It is often noted in the subcutaneous tissues of connective tissues diseases primarily systemic lupus erythematosus, scleroderma and juvenile dermatomyositis4,7. Four main types of calcinosis cutis have been recognized according to etiology: associated with localized or widespread tissue changes or damage (dystrophic calcification), that associated with an abnormal calcium and phosphorus metabolism (metastatic calcification), not associated with any tissue damage or demonstrable metabolic disorder (idiopathic calcification), and Iatrogenic2-3,6-7.
It is recommended that patients be evaluated for abnormalities of calcium and phosphorus metabolism and that they be assessed for associated systemic conditions, such as collagen vascular diseases, renal insufficiency, and vitamin D poisoning. Determining the exact type of calcinosis cutis is very important for selecting accurate management3. Many agents have been used for treatment of calcinosis but none has been accepted as a standard therapy. Case studies have shown that aggressive treatment of the underling inflammatory condition with intravenous immunoglobulin, anti TNF agents, thalidomide and haematopoietic stem cell transplantation has also led to improvement of the calcinosis1,3. Moreover, agents such as warfarin, bisphosphonates and diltiazem have been aimed at treating the process of calcinosis with varying success3.Some experts have advocated surgical excision in severe resistant cases4.Calcinosis cutis has been rarely reported in neonates. It almost exclusively occurs due to iatrogenic causes8. Calcium gluconate has been widely used in the treatment of neonatal hypocalcemia which is a common problem confronted in this age group. When extravasation of calcium gluconate occurs; swelling, erythema, signs of soft tissue necrosis or infection may be seen. Rarely local calcification appears, called calcinosis cutis9-10.
Plain radiography is gold standard for diagnosis but are initially negative because calcium solutions used therapeutically are radiolucent. X-ray findings usually appear within 1-3 weeks9.This is consistent with our case. The pathogenesis of calcinosis cutis caused by extravasation of IV calcium is degeneration and soft tissue necrosis11. If extravasation of calcium gluconate is suspected; the IV line must be removed immediately. Cold packs should be applied for 15 minutes four times a day to treat edema at extravasation sites and limb elevation for 48 hours is suggested12. Supportive care remains the main element of the treatment and only in case of skin necrosis and secondary infection, debridement and antibiotics should be used8.
Calcinosis cutis in neonate can be easily misdiagnosed ascellulitis, arthritis, pyogenic abscess, osteomyelitis and thrombophelibitis8.In the present case also initially we were suspecting an infectious etiology. Initial x-rays can be misleadingly normal as it take about ten days to precipitate. The clinical and radiological findings usually disappear over a span of 2-6 months which is compatible with our case too13.
|
Acknowledgements Nil Competing Interests None declared Author Details MURTAZA RASHID; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. BADER ALOTAIBI; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. IMRAN SHAH; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. MOSTAFA ALSOMALI; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. MOHAMMED BADAWY; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. QURAT UL AIN KHAWAR RAZA; Department of Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. CORRESPONDENCE: MURTAZA RASHID, Department Of Emergency Medicine, Royal Commission Hospital Jubail Industrial City, 31961, Saudi Arabia. Email: dr.murtazarashid@gmail.com |
References
- Chander S, Gordon P. Soft tissue and subcutaneous calcification in connective tissue diseases. Curren Opi Rheumatol. 2012 Mar;24(2):158-64
- Boulman N, Slobodin G, Rozenbaum M, Rosner I. Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005 Jun;34(6):805-12.
- Alsaif F, Abduljabbar A.M. Unilateral Idiopathic Calcinosis Cutis: A Case Report. Case Rep Dermatol 2017;9:20–24
- Gutierrez A Jr, Wetter DA. Calcinosis cutis in autoimmune connective tissue diseases. Dermatol Ther. 2012 Mar-Apr;25(2):195-206
- Venkatesh Gupta SK, Balaga RR, Banik SK. Idiopathic Calcinosis Cutis over Elbow in a 12-Year Old Child. Case Rep Orthop. 2013;2013:241891
- James WD, Berger TG, Elston DM: Andrews’ Diseases of the Skin: Clinical Dermatology, ed 11. Philadelphia, Elsevier Saunders, 2011
- Balin SJ, Wetter DA, Andersen LK, Davis MD. Calcinosis cutis occurring in association with autoimmune connective tissue disease: the Mayo Clinic experience with 78 patients, 1996-2009. Arch Dermatol. 2012 Apr;148(4):455-62.
- Aktas S, Turkyilmaz C, Unal S, Ergenekon E. Calcinosis Cutis Mimicking Infection in a Preterm Infant. Ann Pediatr Child Health. 2015 3(7): 1077.
- Tuncer S, Aydin A, Erer M. Extravasation of calcium solution leading to calcinosis cutis surrounding the dorsal cutaneous branch of the ulnar nerve. J Hand Surg Br. 2006; 31: 288-289.
- Moss J, Syrengelas A, Antaya R, et al. Calcinosis cutis: a complication of intravenous administration of calcium gluconate. J Cutan Pathol 2006;33
- Puvabanditsin S, Garrow E, Titapiwatanakun R, Getachew R, Patel JB. Severe calcinosis cutis in an infant. Pediatr Radiol. 2005; 35: 539-542.
- Millard TP, Harris AJ, MacDonald DM. Calcinosis cutis following intravenous infusion of calcium gluconate. Br J Dermatol. 1999; 140: 184-186.
- Soon SL, Chen S, Warshaw E, Caughman SW. Calcinosis cutis as a complication of parenteral calcium gluconate therapy. J Pediatr. 2001; 138: 778.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




