Assessment of different concentration of Ketofol in procedural operation
Mohamed Daabiss, Medhat Elsherbiny and Rashed Alotibi
Cite this article as: BJMP 2009:2(1) 27-31
|
Abstract
Propofol is an IV anesthetic that is often used as an adjuvant during monitored anesthesia care, the addition of ketamine to propofol may counteract the cardiorespiratory depression seen with propofol used alone. Ketofol (ketamine/propofol combination) was used for procedural sedation and analgesia. However, evaluation of the effectiveness of different concentrations of Ketofol in procedural operation regarding changes in haemodynamics, emergence phenomena, recovery time, the doses, and adverse effects was not yet studied, so this randomized, double blinded study was designed to compare the quality of analgesia and side effects of intravenous different concentrations of ketofol in hundred children of both sex undergoing procedural operation, e.g. esophgoscopy, rectoscopy, bone marrow aspiration and liver biopsy participated in this randomized, double-blinded study. Patients received an infusion of a solution containing either combination of propofol: ketamine (1:1) (Group I) or propofol: ketamine (4:1) (Group II). Subsequent infusion rates to a predetermined sedation level using Ramsay Sedation Scale. Heart rate, noninvasive arterial blood pressure (NIBP), oxygen saturation (SpO2), end tidal carbon dioxide (Etco2) and incidence of any side effects were recorded. There were no significant hemodynamic changes in both groups after induction. However, there was an increase in postoperative nausea , psychomimetic side effects, and delay in discharge times with the largest ketamine dosage (Group I). We concluded that the adjunctive use of smaller dose of ketamine in ketofol combination minimizes the psychomimetic side effects and shorten the time to discharge.
Key words: ketofol, procedural operation, psychomimetic effect.
Procedural operations, are procedures outside the operating room, which developed from a facilitation of diagnostic and therapeutic procedures into an independent subspecialty. Procedural sedation and analgesia is a minimally depressed level of consciousness that retains the patient's ability to maintain a patent airway independently and continuously(1).
Propofol is a short-acting intravenous sedative agent used for the induction and maintenance of general anesthesia for adults and children, sedation for intubated, mechanically ventilated adults in Intensive Care Units (ICU), and in procedures such as colonoscopy. It provides no analgesia(2). Ketamine is classified as an NMDA receptor antagonist and has also been found to bind to opioid receptors and sigma receptors. It induces a state referred to as "dissociative anesthesia"(3).
Ketofol (ketamine/propofol combination) was used for procedural sedation and analgesia. Ketamine and propofol are physically compatible for 1 hr at 23oC with no increase in particle content at Y site injection (4). Ketamine and propofol administered in combination have offered effective sedation for spinal anesthesia and for gynecologic, ophthalmologic, and cardiovascular procedures in all age groups. The opposing hemodynamic and respiratory effects of each drug may enhance the utility of this drug combination, increasing both safety and efficacy and allowing reduction in the dose of propofol required to achieve sedation.
However, evaluation of the effectiveness of different concentrations of Ketofol in procedural operation regarding changes in hemodynamic, emergence phenomena, recovery time, the doses, and adverse effects was not yet studied, so this randomized, double blinded study was designed to compare the quality of analgesia and side effects of intravenous different concentrations of ketofol in children scheduled for procedural operations.
Methods:
A hundred patients, American Society of Anesthesia (ASA) class I or II scheduled for procedural operation, ages 3 to 12 years were enrolled in this study. After obtaining approval from the local research ethics committee, all patients and their parents were informed about the procedure and the anesthetic technique and an informed written consent was obtained from each. Patients with clinically significant cardiovascular, respiratory, hepatic diseases or epileptic patients, longer procedures more than one hour and sensitivity to the drugs were excluded from the study.
Patients were randomized into two equal groups each of 50 patients going for procedural operation, e.g. esophgoscopy, rectoscopy, bone marrow aspiration and liver biopsy. Pre procedural visit was done to evaluate if that patient fulfils the criteria of study and for fasting instruction. In the preoperative waiting area, an IV catheter was placed after applying emla cream. Baseline measurements included Non Invasive Blood Pressure (NIBP), heart rate, respiratory rate, and pain faces scale which is recommended for children aged 3 years and older (Fig1)(5). The level of sedation was determined by Ramsay Sedation Scale(6). A separate observer who was blind to the drug combination being used assessed the depth of sedation of such patients.
*Ramsay Sedation Scale(6)
Patient is anxious and agitated or restless, or both
Patient is co-operative, oriented, and tranquil
Patient responds to commands only
Patient exhibits brisk response to light glabellar tap or loud auditory stimulus
Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus
Patient exhibits no response
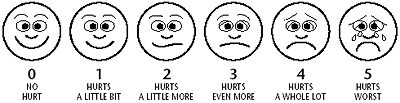
Fig 1: Pain Faces Scale.
A propofol/ketamine admixture was prepared by an assistant who was not involved in the clinical management of the study patients. According to a prestudy randomization schedule of study group assignment, a ketofol (1:1): propofol 14.285 mg, ketamine 14.285 mg/ml by mixing 10 ml propofol 2% (20 mg/ml) with 4 ml ketamine (50 mg/ml) in group I, while in group II ketofol (4:1): propofol 18.1818 mg , ketamine 4.5454 mg/ml by mixing 10 ml propofol 2% (20 mg/ml) with 1 ml ketamine (50 mg/ml).
Both bolus and maintenance doses were given using syringe pump (B/Braun). Set up for delivery of Ketofol in both groups as an initial bolus of 600 g/kg IV (calculated as dose of propofol in these infusions for simplicity), followed by an initial maintenance infusion at 100 g/kg/min by anesthetist who was blinded to the identity of study infusion.The level of sedation was assessed at 1- 3 minutes intervals, and the initial infusion rate was adjusted (in 25 g/kg/min increments) to achieve Ramsay Sedation Scale of 5 before starting the procedure.
During the procedure, patients were kept on oxygen nasal prongs with a CO2 sampling port. All patients were monitored with NIBP, electrocardiography (ECG), Pulse oximetry(SpO2), heart rate (HR), and end tidal carbondioxide( EtCO2). The measurement started before commencement of the intravenous (IV) line and continued five minutes after induction. The patients were also assessed for apnoea, which was defined as the loss of respiratory efforts for more than 20 seconds or fall of SpO2 below 95%. Complaints of pain/discomfort were treated by an incremental increase in the study drug infusion rate.
The study drug infusion was discontinued at the end of the surgical procedure, and the total drug requirements were noted. After the completion of the procedure, patients were transferred to recovery room when an Aldrete score(7) 9-10 was confirmed, and kept there till ready for discharge. The recovery room nurses were blinded to the study medication received by the patients. The incidence of any episode of postoperative nausea and vomiting (PONV) or any other side effects (e.g. hallucinations, agitation or pain) was noted. The patients vital signs were assessed at 5-min intervals. Patients were considered "ready for discharge" when they had stable vital signs, oriented, able to ambulate unassisted, had no intractable nausea or vomiting, and had minimal pain. Discharge times were determined from the time the study drug infusion was discontinued. Outpatients were given written discharge instructions regarding post-procedure precautions and a telephone number to use in case of emergency.
Descriptive variables were analyzed using Students t-test and X2 test as appropriate using SPSS software statistical computer package version 15. Differences between the groups in mean blood pressure (BP),heart rate( HR), end-tidalCO2, oxygen saturation and ketofol requirements were compared using analysis of variance with repeated measures. A P value < 0.05 was considered to be statistically significant. Values are expressed as meanSD.
Results:
There were no significant differences among patients in both groups regarding number of patients, age, sex, weight, ASA physical status, and duration of ketofol infusion (table 1). There was 2 patients excluded in group I; one had a history of epilepsy and the other was acute lymphocytic leukemia on corticosteroids, while in group II only one patient was excluded due to history of epilepsy (Table 1).
Sedation scores were similar in both groups. The average ketofol initial dose in group I was 600 g /kg followed by an average infusion rate of 116 24 g/kg/min, while in group II the average ketofol initial dose was 600 g/Kg followed by an average infusion rate of 132 36 g/kg/min with a significant difference between groups (P <0.05).
There was a minimal decrease in mean arterial blood pressure (MAP) from baseline in both groups following the initial dose of ketofol. Significant hypotension was noted in 2 patients in group I (4%) and in 3 patients in group II (6%) which was corrected by a bolus of Ringers solution 10 ml/kg IV. The diffrence between the groups was statistically insignificant . All the patients had increase in pulse rate compared to the baseline. The change was least in group II (p <0.05), but no patient had severe tachycardia requiring treatment in both groups.
There was increase in Etco2 in both groups after induction with statistically insignificant difference between groups. Patients in both groups had decrease in arterial oxygen saturation (SpO2) after induction. Five patients (10%) in group I and three patients (6%) in group II had apnea and hypoxia after induction (SpO2 <95%). Excessive salivation was noted in 15 patients (31%) in group I but only two patients (4%) in group II. Eight patients (16%) in group I and two patients (4%) in group II experienced airway obstruction or apnea which required airway support. These changes were statistically significant between both groups.
Table 1. Demographic Characteristics, Intraoperative Management, and Recovery Times of Patients in the Study Groups
|
|
Group 1 |
Group 2 |
|
Number |
50 |
50 |
|
Age (yr) |
6.6 3.6 |
7 3.1 |
|
Weight (kg) |
21 8 |
23 7.5 |
|
ASA physical status |
(III) |
(III) |
|
Duration of infusion (min) |
25.312.4 |
23.8 14.8 |
|
Average propofol concentration (mg/ml) |
14.3 |
18.18 |
|
Average ketamine concentration (mg/ml) |
14.3 |
4.54 |
|
ketofol bolus dose (g /kg) |
600 |
600 |
|
Average Ketofol infusion rate (g/kg/min) |
116 24 |
132 36* |
|
Time to ambulation (min) |
15.4 9.5 |
8.2 6.7* |
|
Ready for discharge (min) |
26.511.3 |
15.3 8.4* |
|
Time to actual discharge (min) |
38.813.5 |
28.2 8.9* |
|
-Data are mean SD, median (range). -Group I propofol/ketamine (1:1), Group II = propofol/ketamine (4:1) -ASA = American Society of Anesthesiologists. -Average bolus dose were calculated as dose of propofol in infusion. Average infusion rates were calculated as total drug (propofol) divided by weight and case duration. * Significant difference (P < 0.05) versus group I. |
||
Two patients in group II (4%) and one patient in group I (2%) had pain and discomfort during the procedure which was overcome by incremental boluses of infusions. In group I, one patient (2%) complained of postoperative nausea, four patients (8%) experienced bad dreams and hallucinations and five patients (10%) complained of agitations with no psychomimetic changes in group II
The time to ambulation in group I and II patients was 15.4 9.5 and 8.2 6.7 minutes respectively, while readiness to discharge was 26.5 11.3 in group I and 15.3 8.4 minutes in group II. The time to actual discharge was 38.8 13.5 minutes in group I and 28.2 8.9 minutes in group II. These changes in recovery timings were statistically significant.
Discussion:
The goals of procedural sedation are to provide an adequate level of sedation while minimizing pain and anxiety, maximizing amnesia, minimizing the potential for adverse drug-related events, controlling behavior, and maintaining a stable cardiovascular and respiratory status. A number of studies have demonstrated that the combination of ketamine and Propofol (ketofol) for sedation is safe and effective. The combination of the two agents appears to reduce side effects of each medication used alone, and allows for a rapid recovery time(1).
We compared the safety and efficacy of different concentrations of ketofol in procedural operations in children. The rate of ketofol infusion in group II was higher than in group I due to due to incremental doses of ketofol given to get the desired depth of sedation and abort pain sensation which was due to less ketamine content in such infusion compared to group I. Propofol in the recommended dose of 2-2.5 mg/kg almost always causes fall in blood pressure and the extent of fall depends upon the dose and adjuvant drugs used. Because we used an initial infusion dose of only 600 g/kg, the fall in MAP was mild (6%) and similar in both groups. The induction doses of propofol are reduced considerably by combination with small doses of ketamine. Ketamine had the additional advantage of better hemodynamic stability. Our results are consistent with Furuya et al and Hui et al who suggested that the minimal change observed in arterial pressure may be dose related and also because sympathomimetic actions of ketamine were effective in counter-acting the hemodynamic depression of propofol. There was a trend for pulse rate to increase after the induction in all the groups, but there was no occurrence of profound tachycardia in any group(8,9).
Akin et al published a trial of 60 patients between one month and 13 years of age undergoing cardiac catheterization who received sedation with propofol or propofol plus ketamine (3:1). They found a significant (decrease in MAP in 11 patients in the propofol monotherapy group and three patients in the ketofol group. They concluded that the addition of low-dose ketamine to propofol preserved MAP without prolonging recovery or increasing the incidence of adverse events(10). While, Goh et al published a 90 patients having a laryngeal mask airway (LMA) placed received propofol with either ketamine (5:1), fentanyl (1 g /kg), or placebo normal saline. They found the ketofol group had a significantly higher systolic blood pressure than the other two groups. They concluded that ketofol provided equivalent LMA insertion conditions while maximizing hemodynamics and minimizing apnea(11).
End-tidal CO2 increased slightly after induction in both groups. In agreement with our results, Mildh et al and Persson et al who reported that ketamine-induced sympathoadrenal activation may account for improved ventilation, also arousal secondary to the subjective side effects of ketamine (e.g., perceptual changes and anxiety) may also contribute (12,13). Also our results have confirmed the previous reports of Frey et al and Badrinath et al (14,15), suggesting that the combination of a small-dose ketamine with propofol improves ventilation during sedation.
We expect that the apnea and desaturation recorded in group I (10%) was due to the excessive salivation complicated the higher dose of ketamine in this group which led to impaired breathing and required airway support in 16% of such patients. While apnea and desaturation which happened in group II could be due to the higher infusion rate of propofol in ketofol combination.
Willman and Andolfatto published a study of 114 patients requiring procedural sedation and analgesia mainly for orthopedic procedures were given a 1:1 mixture of propofol and ketamine. Transient hypoxia occurred in 2.6% of patients, out of them one patient required bag valve mask ventilation. Three patients had an emergence reaction, one of whom received midazolam. No patient had vomiting or aspiration. Procedural success rate in this study without the use of adjunctive medications was 96.5%. Median time until recovery was 15 minutes (range 5 to 45 minutes) (16). Furthermore, Akin et al compared propofol to propofol plus ketamine (3:1) in 60 patients between one and 13 years of age undergoing auditory brainstem response testing. There were no cases of desaturation in the ketofol group, but in the propofol group 4/30 experienced desaturation and 6/30 had apnea. The authors concluded that the addition of low dose ketamine to propofol reduced the risk of respiratory depression and the need for repeat medication administration(17).
The incidence of clinically significant psychotomimetic effects was noted in the large-dose ketamine group (group I). This could be a dose-dependent interaction of the excitatory anesthetic ketamine with a pure central nervous system depressant, such as propofol (18,19). There were no post procedural psychotomimetic symptoms recorded in group II. In addition, the patients mood was significantly better in the recovery room and cognitive function recovered more rapidly in such group than those given higher dose of ketamine. Nagata et al and Mortero et al are coinciding with our results as they suggested that ketamine in sedative doses is associated with electroencephalographic activation. Furthermore, small-dose ketamine increases thalamic sensory output and arousal. Sedative effects of propofol may be partially antagonized by the arousal effects of ketamine(20,21). While Akin et al in a trial of 40 adult patients undergoing endometrial biopsy, reported that the combination of propofol (1 mg/kg) plus fentanyl (1 g/kg) was compared to the combination of propofol plus ketamine (2:1). Time to recovery was similar; however time to discharge was longer in the ketofol group secondary to the increased presence of adverse events including nausea, vertigo, and visual disturbances. These authors concluded that although both regimens seem safe, ketofol (2:1) had more adverse events leading to a longer time until discharge and had a lower overall patient satisfaction(22).
Badrinath et al, published One hundred female outpatients undergoing breast biopsy procedures under local anesthesia received an infusion of a solution containing propofol in combination with different doses of ketamine . The sedative infusion rate was varied to maintain a deep level of sedation and normal respiratory and hemodynamic functions. They reported that combination of propofol and ketamine (5:1) provides effective sedation/analgesia during monitored anesthesia care(15). Our results suggest that our combination propofol and ketamine (4:1) was more suitable in procedural operations as Badrinath et al used their preferred combination (5:1) only in monitored anesthesia care and they supplement their sedation with local anesthesia infiltration.
In conclusion, propofol combined with ketamine (4:1) infusion for procedural operations contributed adequate sedation and analgesia without hemodynamic and respiratory depression or psychotomimetic side effects and appears to be a safe and useful technique for procedural operations in the ambulatory setting.
COMPETING INTERESTS
None Declared
AUTHOR DETAILS
MOHAMED DAABISS, MEDHAT ELSHERBINY, RASHED ALOTIBI, Department of Anesthesia, Riyadh Armed forces Hospital, Kingdom of Saudi Arabia.
CORRESPONDENCE: DR MOHAMED DAABIS, P.O.Box 7897 - D186, Riyadh 11159, Saudi Arabia
Email: madaabiss@yahoo.com
References
-
Aouad MT, Moussa AR, Dagher CM. Addition of ketamine to propofol for initiation of procedural anesthesia in children reduces propofol consumption and preserves hemodynamic stability. Acta Anaesthesiol Scand; 2008, 52 (4) : 561-5.
-
Miner JR, Burton JH. Clinical practice advisory. Emergency department procedural sedation with propofol. Ann Emerg Med. 2007;50(2):182-7
-
Harrison N, Simmonds M. "Quantitative studies on some antagonists of N-methyl D-aspartate in slices of rat cerebral cortex". Br J Pharmacol 1985; 84 (2): 38191.
-
Trissl LA, Gilbert DL, and Martinez JF: compatibility of propofol injectable emulsion with selected drugs during simulated Y-site administration, Am J Health-Syst Pharm 1997;54:1287-92
-
Wong DL, Hockenberry-Eaton M, Wilson D, Windelstein ML, Schwartz P. Wong's Essentials of Pediatric Nursing, 6th Edition.St. Louis: 2001; page 1301.
-
Griffiths RD, Jones C. Recovery from intensive care. British Medical Journal 1999; 319: 427 9.
-
Furuya A, Matsukawa T, Czaki M, Nishiyama T, Kume M, Kumazawa T. Intravenous ketamine attenuates arterial pressurechanges during induction of anesthesia with propofol. Eur JAnesthesiol 2001; 18: 88-92.
-
Hui TW, Short TG, Hong W, Suen T, Gin T, Plummer J. Additive interactions between propofol and ketaminewhen used for anesthesia induction in female patients.Anesthesiology 1995; 82: 641-48.
-
Akin A, Esmaoglu A, Guler G, et al. Propofol and propofol-ketamine in
-
Pediatric patients undergoing cardiac catheterization. Pediatr Cardiol. 2005; 26:553-557.
-
Goh PK, Chiu CL, Wang CY, et al. Randomized double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care. 2005; 33:223-8.
-
Mildh L, Taittonen M, Leino K, KirvelO. The effect of low-dose ketamine on fentanyl-induced respiratory depression. Anaesthesia 1998; 53: 96570.
-
Persson J, Scheinin H, Hellstrm G, et al. Ketamine antagonizes alfentanil-induced hypo-ventilation in healthy male volunteers. Acta Anaesthesiol Scand 1999; 43: 74452
-
Frey K, Sukhani R, Pawlowski J, et al. Propofol versus propofol-ketamine sedation for retrobulbar nerve block: comparison of sedation quality, intraocular pressure changes, and recovery profiles. Anesth Analg 1999;89:31721.
-
Badrinath S, Avramov MN, Shadrick M, et al. The use of a ketamine-propofol combination during monitored anesthesia care. Anesth Analg 2000; 90: 85862
-
Willman EV, Andolfatto G. A prospective evaluation of ketofol (ketamine/propofol combination for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2007; 49:23-30.
-
Akin A, Esmaoglu A, Tosun Z, et al. Comparison of propofol with propofol-ketamine combination in pediatric patients undergoing auditory brainstem response testing. Int J Pediatr Otorhinolaryngol. 2005; 69:1541-1545.
-
Mori K, Kawamata M, Mitani H, et al. A neurophysiologic study of ketamine anesthesia in the cat. Anesthesiology 1971;35:37383.
-
Tomoda K, Shingu K, Osawa M, et al. Comparison of CNS effects of propofol and thiopentone in cats. Br J Anaesth 1993;71:3837.
-
Nagata A, Nakao S, Miyamoto E, et al. Propofol inhibits ketamine-induced expression in the rat posterior cingulate cortex. Anesth Analg1998;87:141620.
-
Mortero RF, Clark LD, Tolan MM, et al. The Effects of Small-Dose Ketamine on Propofol Sedation: Respiration, Postoperative Mood, Perception, Cognition, and Pain. Anesth Analg 2001;92:1465-9
-
Akin A, Guler G, Esmaoglu A, et al. A comparison of fentanyl-propofol with a ketamine-propofol combination for sedation during endometrial biopsy. J Clin Anesth. 2005; 17:187-90.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




